
Penetrating chest trauma caused by a falling metallic bar: a case report
Highlight box
Key findings
• For penetrating chest trauma, if the condition permits as in our case, direct removal of foreign bodies is an attractive and better option.
What is known and what is new?
• Thoracotomy and video-assisted thoracic surgery (VATS) are considered the standard treatment for the emergency management of chest trauma;
• Direct removal of foreign bodies could be applied if the patient has no organ damage or active bleeding.
What are the implications, and what should change now?
• For penetrating chest traumas, thoracotomy and VATS are not the only surgical methods, and foreign bodies can be removed directly for patients who are in a similar condition to that described in this case report. Therefore, we should comprehensively evaluate the actual condition of the patient and take the most beneficial surgical approach based on the patient’s situation.
Introduction
Impaled penetrating chest trauma poses an extremely challenging situation for emergency physicians and surgeons. These injuries have a very high mortality rate due to the critical anatomical structures in the region (1). Therefore, a high level of efficiency is needed to rapidly evaluate and identify patients who require surgical intervention.
The presence of foreign bodies in the chest usually results from trauma with a firearm but can include other objects such as broken glass or metal splinters (2). Although there is still considerable controversy, the approach with these cases should always be evaluated based on the risk of removing the object and the complications that could potentially arise after his removal. The appropriate surgical method can be selected after a quick but decisive evaluation. In this report, we describe the case of a 63-year-old man who suffered a penetrating wound caused by a falling metallic bar into his chest, which was a very peculiar case. We present this article in accordance with the CARE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-767/rc).
Case presentation
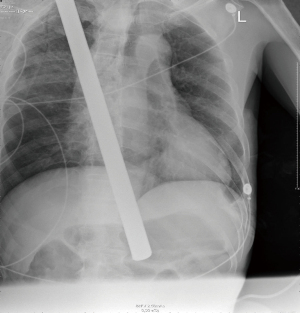
A 63-year-old man presented to the emergency room of Ningbo No. 2 Hospital after being hit by a T-shaped metallic bar falling from a height of 16 meters above the ground. The patient was fully conscious, complained of right chest pain, and was hemodynamically stable. Physical examination revealed a blood pressure of 190/95 mmHg, a pulse rate of 63 bpm, and an oxyhemoglobin saturation of 99% in room air. Bilateral breath sounds were still equal and clear, and the patient’s heart rhythm was regular without murmurs. Clinical examination revealed a metallic bar traversing from the right supraclavicular region to the right fifth intercostal space close to the sternum, with nearly 30 cm of it penetrating the right thorax (Figure 1). No active bleeding or other external injury was observed. Chest X-ray (CXR) showed a radio-opacity consistent with the metallic bar penetrating through the right thorax and a small infiltrative lesion in the upper and mid fields of the right lung, but no obvious pneumothorax or hemothorax was seen (Figure 2). A preoperative chest computed tomography (CT) scan was not performed because the metallic bar was too long to fit inside the CT machine. On the basis of preoperative radiographs, chest ultrasonography, and color Doppler echocardiography, we judged that the thoracic organs of the patient were not injured. Meanwhile, two hours had elapsed between the time of injury and admission, and the patient’s vital signs were stable. At the same time, according to our experience in the treatment of a similar patient, we chose to remove the metallic bar directly instead of using VATS.
The patient was then transferred to the operating room for removal of the metallic bar with general anesthesia and surgical standby. The exposed L-shaped metallic bar on the head side was cut off carefully: the free metal was fastened in a vice. No electric saw was used. Next, the rest of the bar was pulled out from the entry site after disinfection (Figures 3-5). Closed chest tube drainage was promptly performed, with chest tubes inserted through the entry and exit sites (Figure 4). Chest CT was performed immediately after the operation and demonstrated a small subcutaneous emphysema on the right chest wall, mild right pneumothorax, and pleural effusion. Chest CT was performed again on postoperative day 7 and showed decreased right pneumothorax but increased right pleural effusion. However, the patient’s vital signs were stable. Thus, the patient underwent thoracentesis with an additional chest tube in place for 6 days, cultures of pleural effusion showed no bacterial or fungal growth, the patient was discharged on postoperative day 14 in good condition. Regular telephone follow-ups over 3 years showed that the patient recovered well after discharge.


All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
International Multidisciplinary Team (iMDT) discussion
For penetrating injuries, the location of all external wounds must be identified as early as possible, as this will determine which areas of the body might be injured and will help to establish the trajectory of the foreign object (3). It is imperative to assess the patient efficiently and perform a targeted examination, particularly with radiologic imaging, which should not delay definitive management (4). If stable and no cardiac injury is suspected, patients should undergo imaging tests before any intervention (2); chest radiographs (CXR) and trauma ultrasound extended focus assessment (eFAST) can quickly identify the presence of intraperitoneal and intrathoracic findings and should be applied early. The CXR presentation combined with clinical features helps to identify the suspected trajectory of the thorax penetration injury. Any embedded foreign bodies should be left in place during the transports and carefully reinforced to avoid being displaced or transmitting force to internal structures (5).
Thoracotomy has long been considered the standard treatment for the emergency management of major chest trauma involving large foreign body (6). However, the large incisions involved in thoracotomy might be associated with significant morbidity and hospitalization, regardless of whether major injuries are found or not (7). With its emergence in the early 1900s, video-assisted thoracic surgery (VATS) has become a safer and more effective approach for the management of chest trauma, but only for the evaluation and management of hemodynamically stable patients (8). For unstable/non-stabilisable patients with a thoracic injury requiring emergency treatment, thoracotomy remains the method of choice, while VATS is recommended for a wide range of indications in the diagnosis and treatment of stable patients with a penetrating or blunt thoracic trauma (9). Many surgeons suggest that for penetrating chest trauma patients in an unstable condition with major vessel or organ injuries, the prudent approach would be early conversion to thoracotomy, and for patients in stable condition without any major vessel or organ damage, an exhaustive radiographic evaluation, including CXR or CT scan, and even angiogram and esophagogram, should be performed before VATS or open thoracotomy (10).
In general, the modality of therapy for chest trauma depends on the patient’s condition and traumatic mechanism. For instance, a previous study described the case of a patient who attempted suicide using a sickle stabbing into the thorax with a 20-cm blade penetrating the superior mediastinum (11). The sickle was simply pulled out from the extended wound. This decision was made based on a CXR, which showed no significant complications, as in our case. The patient in our case did not have any major vessel or organ injuries because of the lucky angle between the metallic bar and the patient’s body. Therefore, simply removing the metallic bar by pulling it out was considered and conducted with ease. Postoperative chest CT and X-ray confirmed no severe complications. Finally, the patient was discharged without subsequent VATS or thoracotomy and recovered well.
Several issues on the diagnosis and treatment of this patient were further discussed as follows:
Question 1: For such cases, how to cut the exposed metallic bar can avoid secondary damage to the tissues and organs in the body caused by the metallic bar displacement?
Expert opinion 1: Dr. Fabrizio Minervini
The metallic bar should be stabilized and pulled out in the operating room under direct visualization in order to have the possibility to control any vascular damage (if one is suspected). A VATS approach is useful because if a thoracotomy is performed the rib spreader can dislodge the bar or put it under tension.
Expert opinion 2: Dr. Tamas F. Molnar
Fix the rod (using a chick/cramp), and adjust the patient’s position, making him/her as comfortable as possible before cutting. Do not use electric devices or chainsaw. Anesthesia: short acting intravenous drug narcosis with O2 support with intubation standby (conversion) if needed. Perform removal in protection of prophylactic intrapleural drain using a different hole. VATS camera improves the safety of the procedure.
Question 2: What should be noticed during the operation of this type of penetrating chest trauma?
Expert opinion 1: Dr. Fabrizio Minervini
A careful inspection of the thorax should be conducted with a VATS or open approach in order to rule out any damage to the thoracic organs.
Expert opinion 2: Dr. Tamas F. Molnar
Cardiorespiratory stability of the patient is the thin red line. Stable patient: line between the entry and exit points (projection) guides decision making. Safe projection life (peripherial location) removes the object (bar), ideally under VATS control. Even slightest suspicion of cardiac/great vessel/hilar involvement is aroused by the projection line, tracheal intubation is mandatory, following drainage of the pleural space. Start with VATS, always ready to proceed into open thoracotomy. Instable patient requires straight forward open thoracotomy, ideally cell saver ready.
Question 3: Experience of perioperative diagnosis and treatment strategies for patients with penetrating chest trauma?
Expert opinion 1: Dr. Fabrizio Minervini
If the patients in the emergency department is stable a CT Thorax can be performed before going to the OR in order to identify possible damages to the thoracic organs. In presence of Pneumo- or Hemothorax a chest tube should be inserted before surgery.
Expert opinion 2: Dr. Tamas F. Molnar
Again, the circulatory stability is the divisive line with regard to the depth and length of perioperative diagnosis (Actually it is a preoperative one, as there is no need for diagnosis after/postop—so only the first half of the perioperative stage I relevant here). For unstable patient: explore the chest without delay: no images, especially no CT. (Extended FAST: US for chest is a possible exception) Avoid VATS—time consuming preparations, complicated double lumen intubation, the experience of the anesthesia team questionable. One runs against time. Enter the chest cavity as soon as you can, a space full of unwanted surprises. Explore and arrest bleeding, manage lung parenchyma. Stable patient allows imaging, complex planning, usually CT. Patient transfer in protection of prophylactic drainage (blunt dissection method only, never ever trocar/Seldinger technique; tube on Heimlich valve).
Conclusions
We suggest that for penetrating impaled trauma patients in stable condition, it is necessary to complete an exhaustive imaging evaluation to determine the specific position of the foreign body and any injuries to major vessels and organs. If the condition permits as in our case, direct removal of foreign bodies is also an attractive and acceptable option, where the safety of the procedure can be increased by insertion of a camera [non-intubated thoracic surgery (NITS)] even under local anesthesia.
Acknowledgments
Funding: This work was supported by the Ningbo Health Branding Subject Fund (No. PPXK2018-05); the Zhejiang Provincial Natural Science Foundation of China (No. LHDMD23H160001); the HwaMei Research Foundation of Ningbo No. 2 Hospital (No. 2023HMKY32); the Medical Scientific Research Foundation of Zhejiang Province (Nos. 2021KY1009 and 2022KY1138).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-767/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-767/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-767/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okoye OT, Talving P, Teixeira PG, et al. Transmediastinal gunshot wounds in a mature trauma centre: changing perspectives. Injury 2013;44:1198-203. [Crossref] [PubMed]
- Fontelles JLM, da Silva Júnior MF, Rodriguez JER, et al. Thoracic foreign body management after penetrating chest trauma by chainsaw in the Amazon countryside: A case report. Ann Med Surg (Lond) 2021;72:103101. [Crossref] [PubMed]
- Jogiat UM, Strickland M. Transmediastinal penetrating trauma. Mediastinum 2021;5:25. [Crossref] [PubMed]
- Hooda Z, O'kane L, Bustamante JP, et al. Successful surgical management of a combined abdominal and thoracic penetrating injury: a case report. J Surg Case Rep 2023;2023:rjad245. [Crossref] [PubMed]
- Galvagno SM Jr, Nahmias JT, Young DA. Advanced Trauma Life Support® Update 2019: Management and Applications for Adults and Special Populations. Anesthesiol Clin 2019;37:13-32. [Crossref] [PubMed]
- Jones JW, Kitahama A, Webb WR, et al. Emergency thoracoscopy: a logical approach to chest trauma management. J Trauma 1981;21:280-4. [Crossref] [PubMed]
- Bellamy RF. History of surgery for penetrating chest trauma. Chest Surg Clin N Am 2000;10:55-70. viii. [PubMed]
- Manlulu AV, Lee TW, Thung KH, et al. Current indications and results of VATS in the evaluation and management of hemodynamically stable thoracic injuries. Eur J Cardiothorac Surg 2004;25:1048-53. [Crossref] [PubMed]
- Schreyer C, Eckermann C, Neudecker J, et al. VATS in Thorax Trauma. Zentralbl Chir 2023;148:74-84. [PubMed]
- Yokosuka T, Kobayashi T, Fujiogi M, et al. An unusual case of thoracic impalement injury with severe pleural adhesion. Gen Thorac Cardiovasc Surg 2015;63:298-301. [Crossref] [PubMed]
- Ouadnouni Y, Boukatta B. A fortunate survival following a severe penetrating chest trauma. Heart Lung Circ 2014;23:e111. [Crossref] [PubMed]
(English Language Editor: A. Kassem)




