
The disappearing hook wire: a case report
Highlight box
Key findings
• In this case report, we summarized the lessons learned when managing lung nodule localization hook wire migration.
What is known and what is new?
• Previous literature has described hook wire migration, though while the positioning needle was finally removed, problems were encountered when searching for it resulting in undesirable procedures, such as lobectomy, thoracotomy, and secondary surgery.
• We summarized how to avoid the migration of a hook wire before positioning, and how to manage wire migration during surgery.
What is the implication, and what should change now?
• Lobectomy is not the best way to find and extract the hook wire for patients with hook wire migration, and for patients similar to those described in this case report, intraoperative chest computed tomography can serve as a satisfactory localization method for a surgeon. By using this technique, further surgical exploration can be avoided.
Introduction
Hook wire placement is currently one of the most utilized approaches for pre-operative localization (1,2). A few studies have reported the serious complications of hook wire migration (3,4). Migration to the pulmonary artery is an extremely rare complication when performing needle localization with hook wire placement preoperatively for lung nodules (5). We present a case in which the hook wire migrated into the main pulmonary artery and was extracted by extending the original surgical incision immediately after intraoperative CT evaluation. Careful surgical approach when managing this complication can avoid secondary surgery and minimize harm to the patient. We present this article in accordance with the CARE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1643/rc).
Case presentation
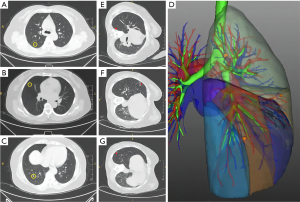
A 50-year-old female was admitted to the hospital due to multiple pulmonary nodules. A right upper lobe posterior segment resection, right middle lobe wedge resection, and right lower lobe S9 + S10b resection by video-assisted thoracoscopic surgery (VATS) were planned (Figure 1A-1D). A total of 3 hook wire localizations (AccuraTM non-repositionable breast localization needles, 20 G, 0.9 mm ×10 cm) of the ground glass nodules (GGNs) were performed in the radiology department (Figure 1E-1G) without any immediate complication. The depth of the hook wire into the lung parenchyma was 3.5 cm in right upper lobe, 2.6 cm in right middle lobe, and 2.2 cm in right lower upper lobe.
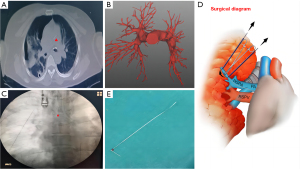
Upon initial thoracoscopic evaluation in the operative room, only the right middle lobe and right lower lobe were observed, whereas the wire to the right upper lobe was unable to be identified. We repeatedly and carefully checked every part of the chest cavity, but failed to find the hook wire positioning needle. We then attempted to locate the positioning needle at the pinhole on the surface of the lung, and took X-rays during the operation, but these efforts were unsuccessful. After careful consideration, in order to determine the position of the hook wire, we temporarily sutured the incision and promptly took the patient for observation with a chest computed tomography (CT) scan. The CT revealed that the positioning needle was located completely in the main pulmonary artery (Figure 2A,2B) and was blocked by the pulmonary valve, with potential severe complications to the patient. Due to the length of positioning needle and the high risk of interventional surgery, the decision was made to extend the original surgical incision to remove the positioning needle. The patient was returned to the operating room and an X-ray (Figure 2C) was performed again to ensure that the positioning needle had not been displaced again. The original surgical incision was extended, the apical subsegment artery of the right lung was isolated, the endovascular positioning needle was touched, the proximal and distal arteries were blocked with line 10, and the artery was cut a small gap with surgical scissors and the tail of the positioning needle from the arterial incision was successfully removed (Figure 2D,2E). The patient was finally discharged 5 days after surgery and without further complications.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
International multidisciplinary team (iMDT) discussion
Discussion among physicians from The Affiliated Hospital of Xuzhou Medical University
After post-operative review by our team, we concluded that the main reason for the displacement of the localization hook wire was due to the lengthy interval between needle positioning and the operation. Additionally, the hook tip was very close in proximity the pulmonary artery during localization, similar to the cases reported by Torigoe (3) and Song (5). Different from the Torigoe’s (3) report of the hook wire migration to the splenic artery, we performed a chest CT immediately during surgery instead of waiting until it was completed. Notably, Chen (4) chose right upper lobectomy to locate the hook wire, and did not choose to perform intraoperative chest CT, finally locating the hook wire in the heart, that was then removed in a second thoracotomy. In this case, we immediately extended the original surgical incision to remove the hook wire, rather than removing it again through the digital subtraction angiography (DSA) or thoracotomy after the operation. This not only reduces the patient burden but also avoids the risk of re-migration of hook wire during the long waiting period.
We believe that some lessons can be learned from this case to avoid this complication in the future. Preoperative techniques: (I) avoid the pulmonary vessels as much as possible during positioning; (II) minimize the interval between positioning and surgery; (III) avoid sharp needle tip positioning needles that may lead to easier migration. Intraoperative techniques: (I) locate the hook wire, remove it and mark on the lung surface before operation; (II) avoid blind surgical planning prior to hook wire localization; (III) determine the position of the hook wire by chest CT if the hook wire cannot be observed.
Several issues on the diagnosis and treatment of this patient were further discussed as follows
Question 1: Presently, there are various non-invasive methods for pulmonary nodule localization, including 3-dimensional reconstruction and injecting indocyanine green (ICG) under electromagnetic navigation bronchoscope guidance. Perhaps the hook wire localization under CT guidance should be discarded?
Expert opinion 1: Fayez Kheir. CT-guided preoperative localization technique with various methods such as hook-wire has been, traditionally, commonly used technique for localization of pulmonary nodules. However, it has been associated with high complication rate as illustrated by this case. Lesion marking guided by minimally invasive bronchoscopic techniques using navigational bronchoscopy along with advanced imaging such as mobile 3D imaging systems are now increasingly used to localize single or multiple pulmonary nodules without associated adverse events as compared with percutaneous approach.
Expert opinion 2: Ajay Wagh. We agree that there are newer, more novel techniques to localize lung nodules including navigation bronchoscopy. However, these techniques are not always available or successful, and CT-guided wire placement remains a popular technique to localize small lung nodules pre-operatively.
Expert opinion 3: Agathe Seguin-Givelet. In view of the serious complications that can result from harpoon localization, it now seems preferable to carry out localization using other techniques, such as fluorescence staining with ICG, either by an endobronchial route or percutaneously in a hybrid room. In the case of ground-glass lesions in particular, this may allow a coil be dropped at the same time which will enable the lesion to be better targeted.
Question 2: In the clinical experience, have you ever encountered similar cases? How did you solve it?
Expert opinion 1: Fayez Kheir. We typically use robotic assisted navigational bronchoscopy along with mobile 3D imaging for localization of pulmonary nodules followed by medical dye injection or fiducial placement for accurate localization of pulmonary nodules. This approach reduced unnecessary complications from CT-guided percutaneous placement of markers.
Expert opinion 2: Agathe Seguin-Givelet. In our experience, we have not encountered similar intravascular migration, but we have on several occasions encountered migration in the cavity, pneumothorax or hemorrhage caused by the hook wire, which have led us to abandon this technique.
Question 3: What do you think will be the best way to locate pulmonary nodules in the future? Please give your reasons.
Expert opinion 1: Fayez Kheir. Artificial intelligence assisted identification, 3D printing, and intraoperative molecular imaging are new emerging technologies that can help locate pulmonary nodules accurately in the future. However, further rigorous studies are needed before implementing such techniques in clinical practice.
Expert opinion 2: Ajay Wagh. As navigation bronchoscopy techniques and imaging improve, success rates for dye marking peripheral lung nodules and the adjacent pleura will become more popular approaches to pre-operatively localize lung nodules. Historically, navigation bronchoscopy and dye marking techniques have had variable success.
Expert opinion 3: Agathe Seguin-Givelet. The best technique in our experience is fluorescence injection par enbronchial way or even percutaneously depending on location or navigation access performed in a hybrid operating room, which may be secured for depth detection by a coil.
Access to a cone beam computed tomography (CBCT)-equipped room is on the increase, and thoracic surgeons, who are still having to deal with more and more small, non-visible and non-palpable lesions, need to be equipped with on-board imaging in the operating theatre.
Question 4: For multiple pulmonary nodules, the current guidelines recommend surgical resection of the main lesion. Do you recommend surgical treatment for the remaining lesions at the same time?
Expert opinion 1: Fayez Kheir. Multidisciplinary discussion among different subspecialities is needed to evaluate whether all lesions or single lesion should be resected at the same time. This will also depend on several factors such as nodule location, ability to localize nodule accurately pre-operatively, patient tolerance to surgery, medical comorbidities, and likelihood that all nodules are in fact malignant.
Expert opinion 2: Agathe Seguin-Givelet. We do recommend resections of suspicious and evolutive lesions even if there are multiples. But if GGO are non-evolutive, we only treat the main lesions or the most suspicious one. The surgical strategy is therefore discussed according to the etiology (suspicion of primary bronchial cancer or metastatic lesions) and the resections to be carried out: the aim is to be carcinological and to sometimes propose segmentectomies of the upper and lower lobes in the same operating time.
Conclusions
When the exact location of a hook wire placed prior to lung nodule surgery cannot be determined, it is necessary to complete an exhaustive radiographic evaluation prior to further surgical exploration. If conditions permit, it is best to remove the hook wire directly under VATS. Blind decisions should be avoided and intraoperative imaging can avoid secondary surgery and minimize harm to the patient.
Acknowledgments
We thank Tianyue Ma for her help in the picture production of this manuscript.
Funding: This study was supported by funds from
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1643/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1643/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-1643/coif). A.W. has done some consulting work for Noah Medical, Ambu, and Medtronic; speaks for Biodesix and also has also done some medicolegal work in the area of lung nodules. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was provided by the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Cornella KN, Repper DC, Palafox BA, et al. A Surgeon's Guide for Various Lung Nodule Localization Techniques and the Newest Technologies. Innovations (Phila) 2021;16:26-33. [Crossref] [PubMed]
- McDermott S, Frenk NE, Fintelmann FJ, et al. Preoperative CT-guided Fiducial Marker Placement for Surgical Localization of Pulmonary Nodules. Radiol Cardiothorac Imaging 2022;4:e210194. [Crossref] [PubMed]
- Torigoe H, Hirano Y, Ando Y, et al. Migration of a hookwire used as a video-assisted thoracoscopic surgery marker into the splenic artery. Gen Thorac Cardiovasc Surg 2020;68:194-8. [Crossref] [PubMed]
- Chen KH, Wu CH, Wei HJ, et al. Migrating hook wire that travels to the heart via the bloodstream: A case report. Medicine (Baltimore) 2023;102:e33349. [Crossref] [PubMed]
- Song X, Li J, Wang D. A hook wire sliding into pulmonary artery and being extracted under DSA: a case report about a rare complication associated with lung nodule localization. J Cardiothorac Surg 2020;15:63. [Crossref] [PubMed]


