Pleural tenting as an effective adjunct in patients with pneumothorax secondary to emphysema evaluated with computed tomography scan
Introduction
Thoracoscopic blebectomy or wedge resection followed by pleurodesis has been regarded as effective procedures in the management and prevention for recurrence in primary spontaneous pneumothorax (1). Its efficacy in the treatment of secondary spontaneous pneumothorax (SSP), which mostly resulted from tobacco smoking, however, was often attenuated by the generalized emphysematous parenchyma and the resultant prolonged air leak. Chest computed tomographic (CT) scan serves as a critical preoperative adjunct in the evaluation of patients with secondary pneumothorax (2), although its efficacy for primary spontaneous pneumothorax is considered limited (3,4). As pleurodesis requires approximation of visceral and parietal pleura, prolonged air leak, which was commonly encountered postoperatively in patients operated on for secondary pneumothorax, may compromise the efficacy of surgical intervention (3).
Pleural tenting, first described in 1956 by Miscall and colleagues (5) and later by Hansen (6) and Rainer Newby (7), is performed in the field of thoracic surgery to prevent air leaks, reduce the residual intrapleural air space, and decrease the period of hospital stay in upper lobectomy (8), lung volume reduction surgery (9), and complicated primary spontaneous pneumothorax (10). Its efficacy in the treatment for secondary pneumothorax, however, has not been elucidated in the literature. We herein retrospectively reviewed our surgical results and delineate the efficacy of pleural tenting and its association with preoperative chest computed tomography (CT) scan in patients with SSP.
Methods
Study subjects and methods
The image and medical records of patients undergoing surgical treatment for SSP in our institution from September 2005 to December 2014 were reviewed. The data was collected on age, sex, smoking status, preoperative chest CT scan image, surgical procedure, blood loss, operative time, duration of tube thoracostomy, and hospital stay. Informed consent was waived because the study was retrospective, and the review of medical records was approved by the Institutional Review Board of National Cheng Kung University Hospital (B-ER-104-141). Patients without preoperative chest CT scan or complete clinical data were excluded. Contralateral SSP was recorded as a new event instead of recurrence, and hence the surgery for contralateral SSP. Recurrence was defined as an ipsilateral pneumothorax after removal of all chest tube. Secondary procedure included re-operation, intrapleural instillation of autologous blood, and bronchoscopic instillation of autologous blood for persistent air leak. Air leak more than 14 days, pneumonia, respiratory failure, cardiac dysrhythmias were included as complications. Mortality was defined as in-hospital death after surgery.
Evaluation of chest CT scan
For evaluation of emphysematous change on preoperative CT image, the visual scoring system described by Goddard et al. (11) was used by two radiologists who were blinded to the patients’ clinical information. Emphysematous change was identified as areas of hypovascularity with low attenuation and was graded with a five-point scale based on the percentage of lung involved; 0 as no emphysematous change in the lung parenchyma, 1 as up to 25% of lung parenchyma was emphysema, 2 as between 26% and 50% of lung parenchyma were involved, 3 as between 51% and 75% of lung parenchyma were involved, and 4 as between 76% and 100% of lung parenchyma were involved. Because the Goddard score had significant association with the outcome (12), the patients were further separated and grouped according to Goddard score (group 1 = Goddard score ≤2, group 2 = Goddard score >2).
Surgical treatment
All patients underwent video-assisted thoracoscopic surgery (VATS) initially. Conversion to a utility thoracotomy was indicated in patients with diffuse bullae, giant bullae, or serious pleural adhesions. Bullectomy was performed with ECHELON FLEXTM ENDOPATH® Staplers, Endo GIATM Ultra Universal Staplers, ECHELON FLEXTM Powered ENDOPATH® Stapler, or iDriveTM Ultra Powered Stapler. Chemical pleurodesis with tetracycline 1,000 mg was routinely performed. At the end of the surgery, one or two 24 Fr chest tubes were placed in the intrapleural or extrapleural space with free drainage. Low-pressure suction (10–20 cmH2O) may be applied if prolonged air leak or progressive subcutaneous emphysema.
Follow-up
The follow-up at out-patient department after discharge continued for 1–3 months, and the long-term follow-up were obtained by telephone interviews and medical record.
Statistical analysis
Chi-square tests and ANOVA were conducted respectively to evaluate the discrete and continuous variables of patient’s characteristics. We used ANOVA to compare the blood loss and operative time between the patients who received pleural tent or not. Furthermore, multivariable regression was performed to evaluate the effects of pleural tent, wedge resection, Goddard score, smoking, and age on the duration of tube thoracostomy, hospital stay, the necessity of a secondary procedure, recurrence, morbidity, and mortality. Kaplan-Meier analysis was performed to evaluate if pleural tenting improved the recurrence free rate. A P value of ≤0.05 was set to indicate statistical significance. SPSS system (IBM SPSS Statistics, version 22.0, Armonk, NY, USA) was used for statistical analysis.
Results
From September 2005 to December 2014, there were 96 surgeries on 84 patients with SSP due to pulmonary emphysema. Seven patients underwent bilateral surgeries because of contralateral pneumothorax, and another six patients were repeatedly operated on for ipsilateral recurrence or prolonged air leak. The median age of the patients at the time of surgery was 57 years (range, 31–94 years), 28 patients (29.2%) were older than 70 years, 87 patients (90.6%) were male, and 85 patients (88.5%) had a smoking history. VATS was performed in 86 cases (89.6%) and then converted to thoracotomy in 10 (10.4%). Ninety (93.8%) patients underwent wedge resection, 79 (82.3%) patients received pleurodesis, and 38 (39.6%) patients underwent pleural tenting procedure. The mean operative time was 120.02±53.685 min (range, 44–345 min), and the mean intraoperative blood loss was 51.56±93.458 mL (range, 0–450 mL). There were 5 (5.2%) patients undergoing secondary procedure before removing chest tube, and 10 (10.4%) patients had ipsilateral recurrent pneumothorax during follow-up. The mean duration for postoperative chest tube drainage was 7.38±6.465 days (range, 1–36 days), and the mean duration of hospitalization was 18.35±22.031 days (range, 3–187 days). The overall morbidity rate was 24.0%; 11 (11.5%) patients had prolonged air leak, 10 (10.4%) developed pneumonia, 4 (4.2%) developed respiratory failure, and 1 (1%) had acute exacerbation of underlying heart failure. Five (5.2%) patients died of postoperative pneumonia. The mean follow-up time after surgery was 40.74±34.331 months (range, 3–122 months).
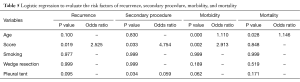
Because the Goddard score had a significant association with the outcome (12), the patients were further separated and grouped according to the Goddard score, where patients with Goddard score ≤2 were in group 1 and those with Goddard score >2 in group 2. The score from each radiologist was tested and proved to be consistent (P<0.001). We used the mean Goddard score to represent the severity of emphysema. The patients’ distribution of each score was listed in the Table 1.
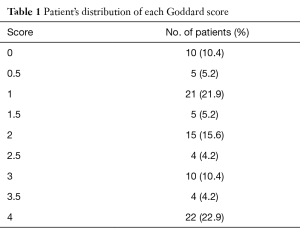
Full table
The patients’ characteristics in group 1 and 2 were listed in Table 2. Patients in group 2 had an older age (P=0.001) and a higher proportion of smoking history (P=0.003). There were fewer patients undergoing wedge resection (P=0.039) and more patients undergoing pleural tenting in group 2 (P=0.001). The patients in group 2 also had a longer duration of tube thoracostomy (P<0.001), longer hospitalization (P<0.001), and higher percentage of postoperative complication (P<0.001), especially prolong air leak (P<0.001) and pneumonia (P=0.001). There was no significant difference between these two groups in operative time, blood loss, recurrence, requirement of a secondary procedure, and mortality. In patients undergoing pleural tenting, we found the patients had significantly more blood loss (P=0.023) and a longer operative time, although the latter did not reach the statistical significance (P=0.087) (Table 3).
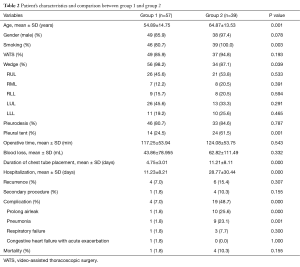
Full table
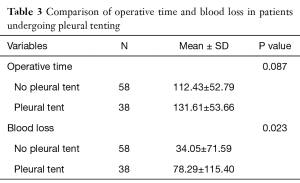
Full table
Patient’s age, Goddard score, smoking history, wedge resection, and pleural tent were all evaluated by mixed models linear regression (Table 4) and binary logistic regression (Table 5) for the impact on the duration of tube thoracostomy, hospital stay, recurrence, the association with a secondary procedure, morbidity, and mortality. In group 1, patient’s age had the most significant effect on hospitalization (P=0.014), while in group 2, patient’s Goddard score and pleural tenting both significantly influenced the duration of tube thoracostomy (P=0.026 and 0.003, respectively). However, there wasn’t a significant factor to influence the hospitalization. The Goddard score was also noticed to have significant impact on recurrence (P=0.019, OR =2.525), the risk of secondary procedure (P=0.033, OR =4.754), and complication (P=0.002, OR =2.913). Pleural tenting was found to decrease the risk of secondary procedure (P=0.034, OR =0.059). For complication and mortality rate, age was an important risk factor (P<0.001, OR =1.110 and P=0.028, OR =1.146).
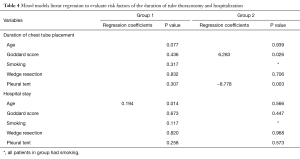
Full table
Full table
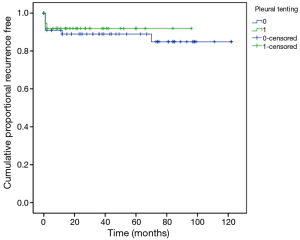
There were totally ten postoperative recurrences in our series; eight occurred within 2 months after the surgery, one at 12th month, and the rest one at 70th month postoperatively. The overall 6-year recurrence free rate was 89.6%. There wasn’t significant difference whether patients received pleural tent or not (P=0.645) (Figure 1).
Discussion
Although the duration of hospitalization was not decreased, we found that pleural tenting significantly reduced the duration of tube thoracostomy in patients with severe emphysema and the resultant pneumothorax. In patients with minor emphysema and pneumothorax, pleural tenting might contribute equally to the recovery as wedge resection of the diseased lung parenchyma and pleurodesis. Patients with severe emphysema are often comorbid with pneumonia and respiratory failure, and cardiovascular complications (12-14), which significantly prolong the hospital stay. Nonetheless, the removal of chest tube often indicated the elimination of residual pleural space and persistent air leak, and the expanded lung parenchyma with improved gas exchange.
Emphysematous change of the lung parenchyma results in bullous formation and SSP. The mainstay of treatment consists of resection of the bulla or diseased lung parenchyma and pleurodesis. Patients with emphysema have increased compliance of lung parenchyma (15), and the pleural space is readily eliminated postoperatively, which is often the case in patients with mild emphysema. The healing process along the resection margin usually is not compromised in mild emphysema and the amount of air leak significantly reduced, and the increased compliance approximates the visceral and parietal pleura and hence facilitates pleurodesis. This explained that in the patients with Goddard score ≤2, neither Goddard score nor pleural tent affected the duration of tube thoracostomy or hospitalization. In patients with severe emphysema, however, the amount of air leak tends to be significant even after the bullous lesion is resected because of the impaired healing capability of lung parenchyma (16). In the patients with Goddard score >2, Goddard score and pleural tent had significant effects on the duration of tube thoracostomy but not hospitalization. Major air leak enlarges the pleural space, preventing the approximation of parietal and visceral pleura, and hence ameliorates the effect of pleurodesis. Pleural tenting was performed via dissection along the extrapleural plane between the parietal pleura and chest wall. The parietal pleura hence falls off the chest wall and attaches the visceral pleura closely because of the intrathoracic negative pressure despite the presence of significant air leak and the subsequently compromised lung expansion (16). The effect of pleurodesis is therefore enhanced and facilitated, which would have otherwise been compromised because of prolonged air leak.
Patients undergoing pleural tent had a lower but not significantly different recurrence rate. Most of the recurrences occurred within 2 months after operation; only one recurred after 12 months and the other after 70 months. Factors such as postoperative complication, patient’s comorbidity, performance status, and the social and financial support system posed substantial impact on the overall hospital stay, especially in those with severe pulmonary emphysema. Hospitalization and mechanical ventilation may increase the risk of recurrence. Besides, near third-one of the patients operated on for pneumothorax were older than 70 years in our study. Some patients died of the comorbidities months later, and the duration of follow-up was therefore limited. Nonetheless, we found that patient’s Goddard score was the independent factor for recurrence, and pleural tent indeed reduced the duration of tube thoracostomy and hence the risk of secondary procedure.
There were some limitations in this study. Selection bias existed because we did not include patients with SSP who did not undergoing chest CT scan as the preoperative evaluation. These patients tended to be younger, had a mild degree of emphysema, and usually a better outcome. These factors may also influence prolonged air leak and postoperative complication.
Conclusions
In conclusion, postoperative air leak in patients undergoing surgery for secondary pneumothorax was significantly associated with the patient’s Goddard score. In patients with moderate and severe emphysema, pleural tenting significantly reduced the duration of tube thoracostomy and the risk of secondary procedure.
Acknowledgements
Funding: This study is granted by the National Cheng University Hospital Research Grant NCKUH-10503015.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The review of medical records was approved by the Institutional Review Board of National Cheng Kung University Hospital (B-ER-104-141), and informed consent was waived because the study was retrospective.
References
- Baumann MH. Treatment of spontaneous pneumothorax. Curr Opin Pulm Med 2000;6:275-80. [Crossref] [PubMed]
- MacDuff A, Arnold A, Harvey J, et al. Management of spontaneous pneumothorax: British Thoracic Society Pleural Disease Guideline 2010. Thorax 2010;65 Suppl 2:ii18-31. [Crossref] [PubMed]
- Baumann MH, Strange C, Heffner JE, et al. Management of spontaneous pneumothorax: an American College of Chest Physicians Delphi consensus statement. Chest 2001;119:590-602. [Crossref] [PubMed]
- Kim J, Kim K, Shim YM, et al. Video-assisted thoracic surgery as a primary therapy for primary spontaneous pneumothorax. Decision making by the guideline of high-resolution computed tomography. Surg Endosc 1998;12:1290-3. [Crossref] [PubMed]
- Miscall L, Duffy RW, Nolan RB, et al. The pleural tent as a simultaneous tailoring procedure in combination with pulmonary resection. Am Rev Tuberc 1956;73:831-52. [PubMed]
- Hansen JL. Parietal pleurolysis (the pleural tent) as a simultaneous space-reducing procedure in combination with pulmonary resection. Acta Chir Scand 1957;112:485-8. [PubMed]
- Rainer WG, Newby JP. Prevention of residual space problems after pulmonary resection. Am J Surg 1967;114:744-7. [Crossref] [PubMed]
- Uzzaman MM, Daniel Robb J, Mhandu PC, et al. A meta-analysis assessing the benefits of concomitant pleural tent procedure after upper lobectomy. Ann Thorac Surg 2014;97:365-72. [Crossref] [PubMed]
- Venuta F, De Giacomo T, Rendina EA, et al. Thoracoscopic pleural tent. Ann Thorac Surg 1998;66:1833-4. [Crossref] [PubMed]
- Eren N, Balci AE, Eren S. Pleural tenting in complicated primary spontaneous pneumothorax. J Cardiovasc Surg (Torino) 2004;45:71-5. [PubMed]
- Goddard PR, Nicholson EM, Laszlo G, et al. Computed tomography in pulmonary emphysema. Clin Radiol 1982;33:379-87. [Crossref] [PubMed]
- Isaka M, Asai K, Urabe N. Surgery for secondary spontaneous pneumothorax: risk factors for recurrence and morbidity. Interact Cardiovasc Thorac Surg 2013;17:247-52. [Crossref] [PubMed]
- Nakajima J, Takamoto S, Murakawa T, et al. Outcomes of thoracoscopic management of secondary pneumothorax in patients with COPD and interstitial pulmonary fibrosis. Surg Endosc 2009;23:1536-40. [Crossref] [PubMed]
- Zhang Y, Jiang G, Chen C, et al. Surgical management of secondary spontaneous pneumothorax in elderly patients with chronic obstructive pulmonary disease: retrospective study of 107 cases. Thorac Cardiovasc Surg 2009;57:347-52. [Crossref] [PubMed]
- Brantigan OC, Mueller E, Kress MB. A surgical approach to pulmonary emphysema. Am Rev Respir Dis 1959;80:194-206. [PubMed]
- Cooper JD, Trulock EP, Triantafillou AN, et al. Bilateral pneumectomy (volume reduction) for chronic obstructive pulmonary disease. J Thorac Cardiovasc Surg 1995;109:106-16. [Crossref] [PubMed]


