
The 3rd international symposium on Non-intubated VATS & Uniportal VATS for carinal reconstruction, Lung and thymic surgery will be held on July 6-8, 2016 in the First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China. This symposium will snapshot the cutting-edge techniques in thoracic surgery, including non-intubated, glasses-free 3D and uniportal VATS and their combination.
For a close look at these techniques, a live broadcast of surgery will be available on July 7 (Beijing time 8:30 - 14:30; GMT 1:30 - 7:30), featuring Non-intubated VATS tracheal sleeve resection, Non-intubated VATS carinal resection and reconstruction, Non-intubated VATS carinal resection and reconstruction and non-intubated VATS sleeve lobectomy.
We warmly welcome you to join us in the event and watch the surgery online via the live broadcast platform. If you are interested, please send your name and affiliation to editor@asvide.com and you will receive a link to watch the surgery live.
Introduction of the main surgeon
Jianxing He, MD, FACS, Department of Cardiothoracic Surgery, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, Guangdong, China.
Professor He is the Director and Professor of the Thoracic Surgery Department, First Affiliated Hospital of Guangzhou Medical University, Guangzhou Institute of Respiratory Diseases (GIRD), as well as the President of the First Affiliated Hospital of Guangzhou Medical University, China. He completed his medical studies at Guangzhou Medical University, and attained a higher research doctorate in thoracic surgery at the Guangdong Institute of Cardiovascular Disease while concurrently acting as the Deputy Director of the Thoracic Surgery Department of Guangzhou Medical University. Professor He later became a Fellow of the American College of Surgeons. He has the world-largest clinical experience in video-assisted thoracic surgery and non-intubation minimally invasive thoracic surgery. His other appointments include being the Primary Investigator of the National Key Laboratory of Respiratory Disease, Chief Advisor of National Ministry of Health Clinical Invasive Pathway Technique Advisory Board, Chairman of National Evaluation Committee for Endoscopic Skills, President of Guangdong Thoracic Surgeon Society, Chief Physician and Director of the thoracic surgery department of the First Hospital Affiliated to Guangzhou Medical University, and Primary Investigator of Translational Medicine Lab in the First Affiliated Hospital of Guangzhou Medical University. Professor He has published more than 200 scientific papers in thoracic surgery, including a seminal paper published in Lancet regarding a molecular assay he developed to predict survival in resected non-squamous, non-small-cell lung cancer. He also established the Asian-Pacific Lung Cancer Specimen and Tissue Bank, which has collected more than 20,000 samples including 18 multi-resisted lung cancer cell lines. Professor He has an extensive and impressive array of research experience, currently undertaking more than 30 scientific projects supported by National 863 Program and National Science Foundation.
Professor He has edited two books Video-Assisted Thoracic Surgery and Tubeless Video-Assisted Thoracic Surgery.
Case 1 Non-intubated VATS tracheal sleeve resection
Case introduction:
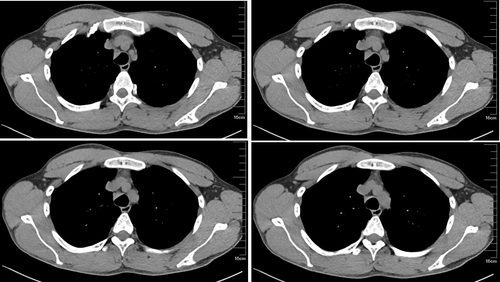
A 34-year-old male patient complained of Cough and expectoration with blood-stained sputum for more than one month.
Tracheoscopy: A neoplasm was visible at the lower trachea. The mucosa was coarse, with obvious congestion and swelling. The fundus mucosa was blue-purple in color, along with sharp carina.
Chest CT: A mass at the middle and lower sections of the trachea.
Previous history: Non-specific
Diagnosis: Tracheal mass; hemangioma?
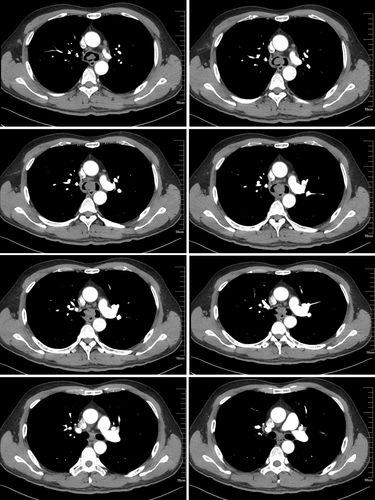
Case 2 Non-intubated VATS carinal resection and reconstruction
Case introduction:
A 72-year-old male patient complained of coughing with hemoptysis for over 1 week.
Tracheoscopy: Squamous cell carcinoma of carina
Chest CT: Carinal mass.
Previous history: hypertension
Diagnosis: Squamous cell carcinoma of carina
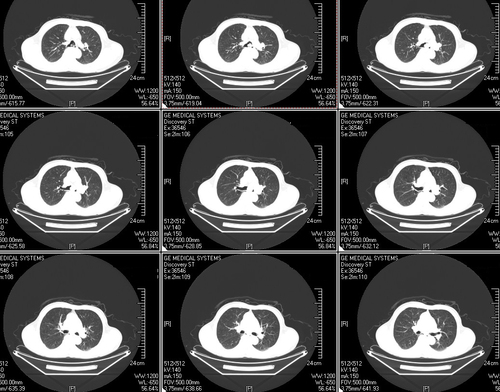
Case 3 Non-intubated VATS carinal resection and reconstruction
Case introduction:
A 55-year-old male patient complained of recurrent cough for over 6 months; blood-stained sputum for more than half month.
Tracheoscopy: The trachea was patent. The carina was coarse, in which a tumor was visible. The remaining lobes and bronchi were patent. Specimens were obtained at 0.5cm/1cm proximal to the carina, 0.5cm/1cm distal to the right side, and 1cm distal to the left side for biopsy. Finally carinal biopsy was performed.
(carinal neoplasm) keratinized squamous cell carcinoma of the lung; No cancer was detected in all five biopsy specimens (0.5cm/1cm proximal to the carina, 0.5cm/1cm distal to the right side, and 1cm distal to the left side).
Chest CT: A soft-tissue mass was seen at the carina of trachea, along with slightly enlarged lymph nodes under the carina.
Lung function: FEV1 2.83 90.1%; FVC 3.83 98%
BMI:23.99 (height, 168cm; weight, 67.7kg)
Previous history: hypertension
Diagnosis: Squamous cell carcinoma of carina
Case 4 Non-intubated VATS sleeve lobectomy
Case introduction:
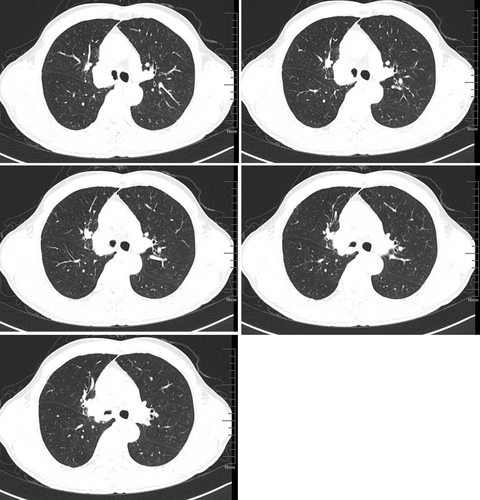
A 56-year-old male patient complained of recurrent cough and expectoration with blood-stained sputum for more than six months.
Tracheoscopic biopsy and pathology: Moderately differentiated squamous cell carcinoma
Chest CT: A mass at the opening of the bronchus in right upper lung complicated with right upper lobe atelectasis.
Previous history: Non-specific
Diagnosis: Squamous cell carcinoma of the right upper lung
