Off-pump coronary artery bypass grafting in high-risk patients: a review
Introduction
The use of off-pump coronary artery bypass (OPCAB) for coronary revascularization remains controversial.
In an early meta-analysis by Cheng et al. OPCAB was reported to reduce perioperative complications such as stroke, acute kidney injury (AKI), respiratory complications and blood transfusions (1). These early positive results were however, questioned by the ROOBY trial which showed a higher rate of primary composite outcomes [death from any cause, repeat revascularization, or nonfatal myocardial infarction at 1 year in OPCAB compared to conventional on-pump coronary artery bypass (ONCAB)].
This study, was criticised because of the high variability of surgeon’s experience and the selection bias (2). A recent large expertise based randomised clinical study (RCT) the CORONARY trial (3), found no difference in the primary composite outcome of death, nonfatal stroke, myocardial infarction, or new renal failure requiring dialysis at 30 days, but found in favour of OPCAB in secondary outcomes of rates of transfusion, AKI, respiratory complications, reoperation for bleeding, operating time, and intensive care unit time. However, patients undergoing OPCAB, received fewer grafts.
The CORONARY trial latter published their 1-year results which found no significant difference between both groups in the rate of the composite outcome, nor in the rate of each component of the composite outcome separately; nor in the rate of repeat revascularization.
Neither of the aforementioned trials was designed to look at high risk patients, the ROOBY trial excluded those at high risk and the CORONARY trial had less than 18% of high risk patients in each arm.
In this review we discuss the role of OPCAB in a high risk population.
Methods
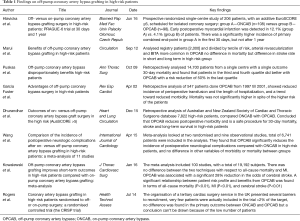
We conducted a literature search through PubMed, Embase, the Web of Science, the Cochrane Library, and Google Scholar, No language, publication date, or publication status restriction was imposed. Title and abstracts were first assessed, suitable papers were individually analysed, and results were tabulated in a spreadsheet to categorize and organize the information. The main articles are presented in a table (Table 1).
Full table
Results
In the most recent single centre RCT by Hlavicka et al. (PRAGUE-6) in high risk patients (EuroSCORE ≥6) comparing ONCAB with OPCAB the primary combined endpoint at 30 days occurred in 20.6% of ONCAB patients and in 9.2% of OPCAB (P=0.028; HR for off-pump, 0.42; 95% CI, 0.19–0.91). At 1 year the primary combined endpoint occurred in 33 (30.8%) and in 21 (21.4%) of ONCAB and OPCAB patients respectively (P=0.117; HR, 0.65; 95% CI, 0.37–1.12) (4).
Puskas et al. in a retrospectively analysed registry data from the Society of Thoracic Surgeons (STS) database, in all isolated CABG cases from 1997 until 2007 divided patients into quartiles based on the STS Predicted Risk of Mortality. A total of 14,766 consecutive patients were included. They showed no statistically significant difference in 30-day mortality between the groups in the two lower quartiles but a significant difference in favour of OPCAB was found in the two higher risk quartiles (odds ratio, 0.62 and 0.45) with an even greater benefit in the highest quartile (odds ratio, 0.45; 95% CI, 0.33–0.63; P<0.0001) (5). Similar results were also reported by other retrospective analyses.
Marui et al. analysed two thousand patients from a registry dividing the risk profile into terciles and found no difference in mortality but a significant difference in the rate of stroke favouring the OPCAB group. The operative characteristics were not similar, the OPCAB group receiving more bilateral internal thoracic arteries (BITAs), which could have contributed to the difference in postoperative stroke rate (6).
García Fuster et al. looked at 547 consecutive patients from a single centre of which 121 had OPCAB, with a higher EuroSCORE (5.4±4) compared to the ONCAB group (2.8±2.3) and despite this found no difference in mortality and a trend in reduction of morbidity and reduction in transfusion (1±1 vs. 1.9±2 blood units; P<0.0001) and postoperative hospital stay (8.9±5 vs. 11.3±7 days; P<0.001) in favour of OPCAB (7).
Dhurandhar et al. conducted a retrospective analysis of the Australian and New Zealand Society of Cardiac and Thoracic Surgeons database and identified 7,822 high-risk patients (based on a higher than 5 AusSCORE) that underwent isolated CABG, of which 545 were operated with OPCAB technique. They found a trend towards lower 30-day mortality and stroke rate in the OPCAB compared to the ONCAB (3.9% vs. 2.4%, P=0.067 and 2.4% vs. 1.3%, P=0.104 respectively). They also reported lower rates of postoperative atrial fibrillation (28.3% vs. 33.3%, P=0.017) and blood transfusion (52.1% vs. 59.5%, P=0.001) in the OPCAB group. This paper had a very low number of patients in the OPCAB group (7%) and similar to other studies these patients were more likely to receive BITAs than in the ONCAB (8).
Two recent meta-analyses of RCTs looked at high risk patients. Kowalewski et al. included several studies that investigated all risk patients and used special statistic methods to compare them by risk profile. They concluded that in high risk patients there is a linear correlation between the risk profile and the increase of the benefit of OPCAB in: all-cause mortality (P<0.01), myocardial infarction (P<0.01), and stroke (P<0.01) (9).
Wang et al. meta-analysed exclusively papers focused on high risk patients and found a difference in neurological complications in favour of OPCAB. However, the total number of patients analysed was too small to conclude on other aspects such as stroke rate and myocardial infarction (10).
Recently a trial was designed by Rogers et al., specifically to address this group of patients the coronary artery bypass grafting in high-risk patients randomised to OPCAB or ONCAB surgery: a randomised controlled trial (the CRISP trial). The study had to be stopped due to logistic reasons with respect to patient recruitment and the availability of data for the inclusion criteria. The report provided from the trial can serve as a canvas for the design of future trials, which are necessary to accurately assess the benefits or disadvantages of OPCAB in high risk patients (11).
Discussion
The evidence in the literature seems to support the benefit of OPCAB in high risk patients. Several studies, RCTs and meta-analyses have shown improved outcomes in this patient group. We found no studies that showed adverse outcomes when looking specifically at high risk patients. The reason for the good results of OPCAB in high risk patients is not clear. Early studies demonstrated that cardiopulmonary by-pass produces an increase of the inflammatory response, oxidative stress and myocardial reperfusion injury; it is possible that these negative effects are better tolerated by intermediate or low risk patients but not in high risk group.
It is important to mention however, that most studies suffer from a selection bias that is very difficult to overcome, as only specialised OPCAB centres and surgeons would embark in research involving high risk patients operated using this technique.
It is well known that surgeon and centre experience in OPCAB or rather the lack of it can severely influence outcome, more so than in ONCAB revascularisation.
Another weakness in our review, and a general weakness of any analysis that investigates categorizing groups of patients based on their risk profiles, is the difference in the several risk scores available and their use in the papers analysed. A single risk score must be used in large randomised controlled multi-centre trials to be able to overcome the mentioned bias.
Thus this review may leave us with a conclusion not be applicable to all cardiac surgery centres. This correlates with the current 2014 guidelines of the European Society of Cardiology on myocardial revascularization that state that off-pump CABG should be considered for subgroups of high-risk patients in high-volume off-pump centres, a class IIa recommendation with a level B of evidence.
Acknowledgements
This study was supported by the British Heart Foundation and the NIHR Bristol Cardiovascular Biomedical Research Unit.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cheng DC, Bainbridge D, Martin JE, et al. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology 2005;102:188-203. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]
- Hlavicka J, Straka Z, Jelinek S, et al. Off-pump versus on-pump coronary artery bypass grafting surgery in high-risk patients: PRAGUE-6 trial at 30 days and 1 year. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016;160:263-70. [Crossref] [PubMed]
- Puskas JD, Thourani VH, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg 2009;88:1142-7. [Crossref] [PubMed]
- Marui A, Okabayashi H, Komiya T, et al. Benefits of off-pump coronary artery bypass grafting in high-risk patients. Circulation 2012;126:S151-7. [Crossref] [PubMed]
- García Fuster R, Montero JA, Gil O, et al. Advantages of off-pump coronary bypass surgery in high-risk patients. Rev Esp Cardiol 2002;55:383-90. [PubMed]
- Dhurandhar V, Saxena A, Parikh R, et al. Outcomes of On-Pump versus Off-Pump Coronary Artery Bypass Graft Surgery in the High Risk (AusSCORE > 5). Heart Lung Circ 2015;24:1216-24. [Crossref] [PubMed]
- Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: Meta-analysis. J Thorac Cardiovasc Surg 2016;151:60-77.e1-58.
- Wang J, Gu C, Gao M, et al. Comparison of the incidence of postoperative neurologic complications after on-pump versus off-pump coronary artery bypass grafting in high-risk patients: A meta-analysis of 11 studies. Int J Cardiol 2015;185:195-7. [Crossref] [PubMed]
- Rogers CA, Pike K, Campbell H, et al. Coronary artery bypass grafting in high-RISk patients randomised to off- or on-Pump surgery: a randomised controlled trial (the CRISP trial). Health Technol Assess 2014;18:v-xx, 1-157. [Crossref] [PubMed]


