Association between post-sternotomy tracheostomy and deep sternal wound infection: a retrospective analysis
Introduction
Tracheostomy has traditionally been used as a means of facilitated mechanical ventilation in patients requiring respiratory management following cardiac surgery. Long-term ventilator dependency in this population occurs in up to 20% of patients (1). Tracheostomy offers several potential benefits including reduced sedation requirements (2), reduction in incidence of pneumonia (3), reduction in work of breathing (4), and more rapid weaning from mechanical ventilation. For patient comfort and to facilitate ease of mechanical ventilation, tracheostomy is commonly performed on ventilator-dependent patients (5).
However in the clinical setting, the advantages of tracheostomy has been questioned by concerns surrounding evidence of its association with increased risk of deep sternal wound infections (DSWI). Several studies have suggested that microbial contamination and consecutive infection of the sternal wound with microbes from tracheostomy may increase the risk of DSWI and mediastinitis (5,6). It could be argued that in principle, delaying the tracheostomy could interfere less with early phase of sternal and incisional healing. However, this has not be uniformly supported by clinical data, with reports refuting the association between tracheostomy and DSWI (5,7,8).
At our institution, tracheostomy has been performed for cardiac surgery patients requiring prolonged mechanical ventilation over the past decade. The present study sought to evaluate retrospectively our experience with post-sternotomy tracheostomy among cardiac surgery patients, by investigating predictors of DSWI in this population.
Methods
Study population
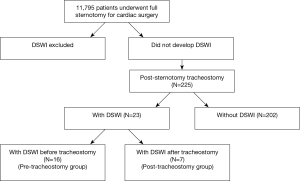
Between July 2003 and June 2013, 11,795 patients underwent open cardiac surgery via sternotomy in our department. Among these, 225 underwent post-sternotomy tracheostomy. Data were obtained by reviewing the Cardiac Surgical and Cardiac Intensive Care Unit (ICU) databases for adult cardiac patients. The inclusion criteria were patients greater than 14 years of age who underwent cardiac surgery via full median sternotomy at the Prince Charles Hospital, Brisbane, Australia. Patients who developed DSWI prior to tracheostomy were excluded from analysis (Figure 1).
Outcomes
Cardiac surgery operations with full sternotomy were classified as coronary artery bypass grafting (CABG), aortic valve (AV), mitral valve (MV), tricuspid valve (TV), pulmonary valve (PV), aortic wall, and congenital procedures. Patients were classified into tracheostomy vs. no tracheostomy post-sternotomy. Tracheostomy patients were further classified into DSWI vs. no-DSWI patients. These subgroups were used to assess risk factors for DSWI following tracheostomy. All sternotomy patients were also grouped into patients who developed DSWI vs. no-DSWI, to assess risk factors for DSWI following sternotomy regardless of tracheostomy.
Further outcome measures for this study included mortality (death by causes: cardiac, neurological, renal, vascular, infection, pulmonary, gastrointestinal, haemorrhagic), operative parameters [cross-clamp duration, cardiopulmonary bypass (CPB) duration, ICU stay and ICU re-admission], major postoperative complications [septicemia, ventilation, pneumonia, pulmonary embolism, red blood cell (RBC) transfusions, readmission for bleeding or tamponade, readmission for DSWI]. The study was approved by our local ethics committee.
Statistical analysis
Continuous variables were given as a median and standard deviation, whereas categorical variables were given as a number and percentage proportion. Univariate analysis was carried out using Wilcoxon rank sum test for continuous variables and 2-sided Fischer’s exact test for categorical variables. These variables were then entered into a stepwise multivariate regression model to identify independent predictors of DSWI. P value less than 0.05 was considered as significant. The statistical analysis was conducted using SAS.
Results
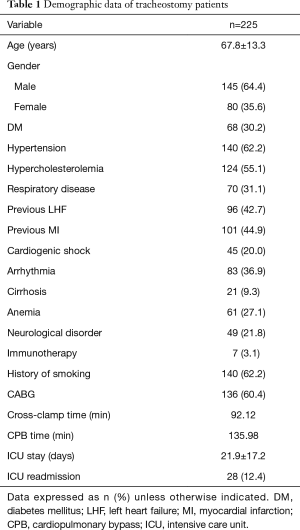
Out of the 11,795 sternotomy patients analyzed, 225 (1.9%) underwent tracheostomy. The majority of tracheostomy patients were male, with males (64.6%) and females (35.6%). The mean age was 68±13 years. Patient comorbidities included diabetes (30.2%), hypertension (62.2%), respiratory disease (31.1%), previous heart failure (42.7%), previous infarction (44.9%), cirrhosis (9.3%), anemia (27.1%) and neurological disorders (21.8%) (Table 1). The mean cross-clamp time and CPB time were 92.12 and 135.98 minutes, respectively. The mean length of ICU stay was 22±17 days, and 12.4% of tracheostomy patients were readmitted into ICU.
Full table
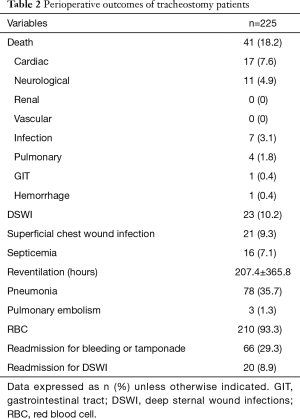
The overall mortality rate for post-sternotomy tracheostomy patients was 21.3%. The major causes of death included cardiac (7.6%), neurological (4.9%), infection (3.1%) and pulmonary (1.8%). DSWI developed in 23 patients (10.2%) of the tracheostomy group, of which seven patients developed the DSWI post-tracheostomy (3.1%). Other perioperative outcomes including septicemia, pneumonia, pulmonary embolism and readmissions are summarized in Table 2.
Full table
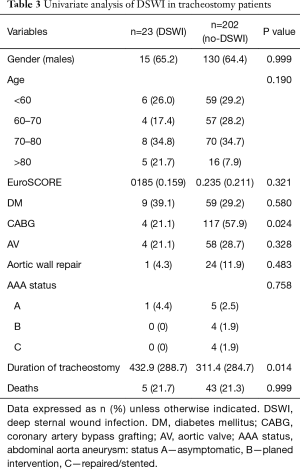
Table 3 demonstrates the univariate analysis assessment to identify risk factors for DSWI in post-sternotomy tracheostomy patients. Significant risk factors include CABG (P=0.024) and duration of tracheostomy (P=0.014). Demographic properties including gender, age, EuroSCORE, diabetes, AV surgery, aortic wall repair, abdominal aorta aneurysm (AAA) status were not predictive of DSWI in tracheostomy patients. There was also no significant association between DSWI in tracheostomy patients and mortality.
Full table
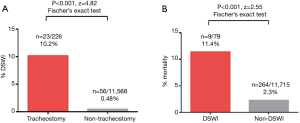
The incidence of DSWI across all sternotomy patients was also assessed. DSWI was significantly higher in tracheostomy versus no-tracheostomy patients (10.2% vs. 0.48%; P<0.001). Twenty three patients had DSWI in tracheostomy group (10.2%), of which seven patients developed the DSWI post-tracheostomy (3.1%). DSWI was also associated with higher mortality rates compared to non-DSWI patients (11.4% vs. 2.3%; P<0.001) (Figure 2).
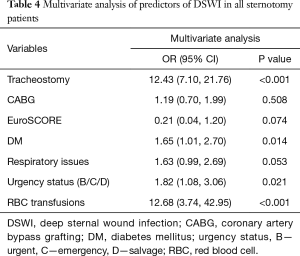
Multivariate logistic regression analysis identified tracheostomy (OR, 12.43; 95% CI, 7.10, 21.76; P<0.001), diabetes (OR, 1.65; 95% CI, 1.01, 2.70; P=0.014), urgency status (OR, 1.82; 95% CI, 1.08, 3.06; P=0.021) and RBC transfusions (OR, 12.68; 95% CI, 3.74, 42.95; P<0.001) as determinants of DSWI across all sternotomy patients (Table 4).
Full table
Discussion
The association between post-sternotomy tracheostomy and mediastinitis following median sternotomy is a concern that has not been well addressed by conflicting data in the literature. The proposed mechanism involves the spread of bacteria from the tracheostoma to the wound site (9,10). Sternal wound infections have been associated with life-threatening complications, responsible for up to high mortality rates of 29% in adult cardiac surgical patients (11). In our present study, DSWI was indeed associated with significantly higher mortality compared to no-DSWI patients (11.4% vs. 2.3%, P<0.001). However, for high risk surgical patients with a complicated post-operative recovery, it is not clearly established whether the potential benefits of tracheostomy would be outweighed by the risk of surgical site infections.
Over the past decade, tracheostomy was performed in 1.9% of cardiac surgery patients at our institution for airway and ventilation management post-sternotomy. The present study showed a strong association between post-sternotomy tracheostomy and DSWI, with OR of 12.4 in a multivariate risk model. Our multivariate analysis also identified diabetes, urgency status and RBC transfusions as predictors of DSWI. These trends are well supported by prior studies (5,6), who identified tracheostomy as a risk factor for DSWI and operative mortality. Curtis et al. (6) reported 8.6% incidence of DSWI in tracheostomy patients compared to 0.7% in the non-tracheostomy patients. In their study of 6,057 patients, mortality in the tracheostomy group was 24.7% compared with 5.2% in the non-tracheostomy cohort, consistent with the trends observed in the present study. Force et al. (5) identified 291 patients out of 16,277 cardiac procedures who had post-sternotomy tracheostomy. DSWI occurred in 0.8% of all patients, and 3.4% of tracheostomy patients. Their multivariate model also identified diabetes, age and BMI as predictors of DSWI, but tracheostomy with the greatest odds ratio of 5.7. For the percutaneous tracheostomy approach, which would be expected to provide an improved tube seal and reduce contamination of the sternal wound, Ngaage et al. (12) showed that the risk of DSWI was similar compared to open surgical tracheostomy.
Given that tracheostomy is often performed in high-risk patients with complicated postoperative recovery, it is difficult to define whether these patient profiles or the tracheostomy procedure itself is responsible for mediastinitis. In order to address this, the present study performed univariate analysis within the tracheostomy cohort only, and identified that CABG procedures and long durations of tracheostomy were predictive risk factors for DSWI. In contrast, other factors such as age, gender, EuroSCORE, diabetes, and AAA status were not predictive of DSWI in this population. The elevated infection risk with CABG is likely due to devascularization of sternum, prolonged operative durations and longer CPB time (13), given that length of operative procedures have been previously associated with prolonged postoperative mechanical ventilation. Longer durations of tracheostomy also put the patients in a window of greater exposure to infection, thus increasing the risk of superficial sternal wound infections and DSWI (14,15).
Limitations
Our study is limited by several constraints. Firstly, the retrospective nature of the current study means that there is some inherent baseline bias and variation which may undermine the validity of the results presented. Ideally, large prospective studies that are adequately powered are needed to confirm these findings. However, given the low frequency of DSWI and tracheostomy patients, an adequately powered, randomized trial will be difficult to design. Secondly, there was a lack of information on the causative organisms of the DSWI, and whether or not this coincided with any baseline comorbidities including respiratory tract infections. Given the infrequent use of tracheostomy and relative rare DSWI complications, there was also difficulty in obtaining adequately powered, matched patient cohorts for comparison.
Conclusions
Overall, the present study demonstrated that tracheostomy was an independent risk factor for post-sternotomy DSWI, and that DSWI was a predictor of mortality. For tracheostomy patients, CABG procedures and longer durations of tracheostomy were strong predictors of DSWI. Across all sternotomy patients, tracheostomy, diabetes, urgency status and transfusions were significant risk factors for DSWI. For very sick patients with no alternatives of ventilation, they most likely need a tracheostomy and might be at higher risk of DSWI. As such, the decision for tracheostomy post-sternotomy is considered on a case by case basis.
Acknowledgements
None.
Footnote
Conflicts of Interest: This article was presented in Royal Australasian College of Surgeons, 2014 Annual Scientific Congress, Singapore, May 7, 2014.
Ethical Statement: The study was approved by their local ethics committee (HREC/13/QPCH/282).
References
- Murthy SC, Arroliga AC, Walts PA, et al. Ventilatory dependency after cardiovascular surgery. J Thorac Cardiovasc Surg 2007;134:484-90. [Crossref] [PubMed]
- Nieszkowska A, Combes A, Luyt CE, et al. Impact of tracheotomy on sedative administration, sedation level, and comfort of mechanically ventilated intensive care unit patients. Crit Care Med 2005;33:2527-33. [Crossref] [PubMed]
- Rumbak MJ, Newton M, Truncale T, et al. A prospective, randomized, study comparing early percutaneous dilational tracheotomy to prolonged translaryngeal intubation (delayed tracheotomy) in critically ill medical patients. Crit Care Med 2004;32:1689-94. [Crossref] [PubMed]
- Diehl JL, El Atrous S, Touchard D, et al. Changes in the work of breathing induced by tracheotomy in ventilator-dependent patients. Am J Respir Crit Care Med 1999;159:383-8. [Crossref] [PubMed]
- Force SD, Miller DL, Petersen R, et al. Incidence of deep sternal wound infections after tracheostomy in cardiac surgery patients. Ann Thorac Surg 2005;80:618-21; discussion 621-2. [Crossref] [PubMed]
- Curtis JJ, Clark NC, McKenney CA, et al. Tracheostomy: a risk factor for mediastinitis after cardiac operation. Ann Thorac Surg 2001;72:731-4. [Crossref] [PubMed]
- Byhahn C, Rinne T, Halbig S, et al. Early percutaneous tracheostomy after median sternotomy. J Thorac Cardiovasc Surg 2000;120:329-34. [Crossref] [PubMed]
- Gaudino M, Losasso G, Anselmi A, et al. Is early tracheostomy a risk factor for mediastinitis after median sternotomy? J Card Surg 2009;24:632-6. [Crossref] [PubMed]
- Fariñas MC, Gald Peralta F, Bernal JM, et al. Suppurative mediastinitis after open-heart surgery: a case-control study covering a seven-year period in Santander, Spain. Clin Infect Dis 1995;20:272-9. [Crossref] [PubMed]
- Bacchetta MD, Girardi LN, Southard EJ, et al. Comparison of open versus bedside percutaneous dilatational tracheostomy in the cardiothoracic surgical patient: outcomes and financial analysis. Ann Thorac Surg 2005;79:1879-85. [Crossref] [PubMed]
- Colombier S, Kessler U, Ferrari E, et al. Influence of deep sternal wound infection on long-term survival after cardiac surgery. Med Sci Monit 2013;19:668-73. [Crossref] [PubMed]
- Ngaage DL, Cale AR, Griffin S, et al. Is post-sternotomy percutaneous dilatational tracheostomy a predictor for sternal wound infections? Eur J Cardiothorac Surg 2008;33:1076-9; discussion 1080-1. [Crossref] [PubMed]
- Kubota H, Miyata H, Motomura N, et al. Deep sternal wound infection after cardiac surgery. J Cardiothorac Surg 2013;8:132. [Crossref] [PubMed]
- Ladowski JM, Downey HE, Ladowski BJ, et al. Early versus Late Tracheostomy for Ventilator Dependence after Cardiovascular Surgery: Long-Term Results. World J Cardiovasc Surg 2013;3:114-8. [Crossref]
- Trouillet JL, Luyt CE, Guiguet M, et al. Early percutaneous tracheotomy versus prolonged intubation of mechanically ventilated patients after cardiac surgery: a randomized trial. Ann Intern Med 2011;154:373-83. [Crossref] [PubMed]