Peripheral venous catheter fracture with embolism into the pulmonary artery
Introduction
Peripheral vein catheterization is a very frequent medical or nursing maneuver all over the word; indeed, a peripheral venous catheter (PVC) is placed in almost every patient that is hospitalized. It is generally considered a harmless procedure. The most frequent complications related to this maneuver are vein rupture, paravenous subcutaneous infusion, phlebitis and thrombosis. PVC rupture associated with embolism is an unlikely complication. To our knowledge, this is the first reported case of a PVC fracture with pulmonary artery embolization.
Case presentation
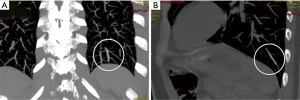
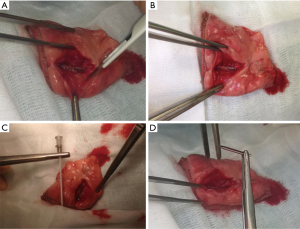
A 40-year-old Caucasian female was admitted to an emergency department because of prolonged abdominal pain with diarrhea. Before starting the intravenous supporting therapy, a PVC was placed, after a few attempts, in the medial antebrachial vein. At the time of discharge, the nurse reported some resistance to PVC retraction, and after complete removal the absence of its end portion it was observed. The patient was informed, and a vein ultrasound was immediately performed without demonstrating the presence of plastic fragment in the upper limb veins. The angio-computed-tomography-scan was performed, showing the presence of a hyperdense structure of elongated shape (18 mm-long) in the lumen of a terminal branch of the lower lobe pulmonary artery, suggesting a fragment of the device (Figure 1). Due to the small-size of the fragment and its peripheral location, in agreement with the patient, it was decided to wait and see. In the following weeks, the patient began to have mild fever with dry cough, unresponsive to prolonged medical therapy with antibiotics, antipyretics and corticosteroids. After 2 months, the patient underwent another angio-computed-tomography-scan which confirmed a small filling defect at the level of a branch of the sub-segmental pulmonary artery for the left lower lobe, so there was no change of position or migration of the device compared to the previous radiological control, and no signs of infections pulmonary embolism/thrombosis or pulmonary consolidation around the fragment. The patient became strongly motivated to undergo removal of the foreign body because of the persistence of symptoms that limited her normal daily life. She came to our attention for this purpose. The case was submitted to our interventional radiologist and cardiologist to evaluate the possibility of an endovascular procedure that was rejected due to the small size of the fragment and its peripheral position. Surgery was therefore planned. The operation was performed through a lateral-minithoracotomy (4 cm muscle-sparing) at the level of the sixth intercostal space that allowed the palpation of parenchyma including the PVC fragment, and we thus performed a wedge resection. The surgical specimen was opened on the operating field to detect the presence of the foreign body (Figure 2). The postoperative course was uneventful. After 6-month follow-up, she is in excellent medical condition without therapy and no limitation to her daily life.
Discussion
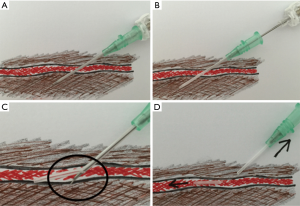
The first description of intravascular embolization of a catheter fragment was made in 1954 (1). In the literature, the incidence of this rare complication varies from 0.2% to 4.2% and this event mainly occurs with central venous catheter or totally implanted port devices (2). Fragmentation can occur during implantation, most frequently in the subclavian vein, or during catheter explantation. In the latter case, catheter fractures are generally the result of device damage during implantation, particularly during guide-wire removal and device manipulation (3) or the so called “pinch-off syndrome”, recurrent compression of the catheter between the clavicle and the first rib (2). Our case represents a different situation because it was a PVC positioned in the left cubital vein and it remained for in situ just a few hours. We hypothesize that the fracture mechanism occurred at the time of catheter placement, probably related to the retraction followed by the reinsertion of the needle in an attempt to correct a first malposition. In this way the needle could damage the plastic liner which was then broken during removal that in fact was reported as having been a little difficult (Figure 3). In the literature the most common site of embolization of such plastic fragments are the right cardiac chambers (49.6%) followed by pulmonary arteries (35%), depending on the size of the fragment (2,3). In our case, the catheter fragment embolized in a sub-segmental left lower lobe pulmonary artery. It is interesting that this position is the typical site in which materials inserted in the forearm, following the blood circulation through the basilic and cephalic veins embolize. Indeed, we found various reports in the literature regarding migration of subdermal contraceptive implants that were positioned in the forearms, with shape and dimension very similar to a fragment of PVC (4-6). In all these cases, the foreign body was found in a subsegmental branch of the left lower lobe artery as in our case. Perhaps this event was based on the anatomical and fluid dynamic features of the pulmonary circulation.
The indications for the removal of these foreign bodies are still debated. Some authors suggest that the long-term risk of pulmonary or septic complications is sufficient to justify extraction (2). The most used and least invasive technique is generally percutaneous retrieval (2,7). Only in 2.3% of cases was surgery required (2,4). In our case, the percutaneous approach was judged not feasible because of the too peripheral location of the foreign body. Video assisted thoracic resection was not attempted because of the very small dimensions of the plastic fragment with impossibility of visualization and correct identification. We preferred to perform a very small lateral-thoracotomy (4 cm) with minimal rib retraction just to be able to put two fingers inside the chest for lung parenchyma palpation. In this way we were able to safely identify the catheter and thus perform a limited atypical pulmonary resection with an endo-gia (Figure 2). This approach required three-day hospitalization without early or long-term complications with a full return to a normal daily life of the young patient.
Conclusions
The placement of a PVC is not always a harmless procedure, and fracture and thus embolism of the catheter can happen. Extraction followed by reinsertion of the wire after cutaneous puncture is not advisable. Every time there are difficulties in positioning or, in particular, in removal of a PVC the device should be carefully inspected to verify its integrity. The advisability of removal of these small foreign bodies is debated; percutaneous retrieval is preferred, while surgery should be discussed case by case.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Turner DD, Sommers SC. Accidental passage of a polyethylene catheter from cubital vein to right atrium; report of a fatal case. N Engl J Med 1954;251:744-5. [Crossref] [PubMed]
- Surov A, Wienke A, Carter JM, et al. Intravascular embolization of venous catheter--causes, clinical signs, and management: a systematic review. JPEN J Parenter Enteral Nutr 2009;33:677-85. [Crossref] [PubMed]
- Loughran SC, Borzatta M. Peripherally inserted central catheters: a report of 2506 catheter days. JPEN J Parenter Enteral Nutr 1995;19:133-6. [Crossref] [PubMed]
- D'Journo XB, Vidal V, Agostini A. Intravascular pulmonary migration of a subdermal contraceptive implant. Ann Thorac Surg 2015;99:1828. [Crossref] [PubMed]
- Patel A, Shetty D, Hollings N, et al. Contraceptive implant embolism into the pulmonary artery. Ann Thorac Surg 2014;97:1452. [Crossref] [PubMed]
- O' Brien A, O'Reilly MK, Sugrue G, et al. Subdermal Contraceptive Implant Embolism to a Pulmonary Artery. Ann Thorac Surg 2015;99:2254-5. [Crossref] [PubMed]
- Cekirge S, Weiss JP, Foster RG, et al. Percutaneous retrieval of foreign bodies: experience with the nitinol Goose Neck snare. J Vasc Interv Radiol 1993;4:805-10. [Crossref] [PubMed]


