Clinical outcomes for multi- and extensively drug resistant tuberculosis patients with adjunctive resectional lung surgery in Beijing, China
Introduction
Tuberculosis (TB) is still a major global public health concern, with 9.6 million new cases and 1.5 million deaths in 2014 (1). Due to the successful implementation of directly observed therapy short-course (DOTS) strategy, the incidence and mortality of TB have decreased in many high-burden countries (1). Unfortunately, the burgeoning multidrug-resistant tuberculosis (MDR-TB) and extensively drug resistant tuberculosis (XDR-TB) epidemic is a more serious problem and becomes a threat to global TB control efforts (2-4).
Compared with drug-susceptible TB, the treatment of MDR-TB patients requires prolonged medication with second-line drugs, which are more toxic and expensive (5,6). However, the medical treatment for MDR-TB with second-line drugs does not usually achieve satisfactory outcomes, with an estimated cure or treatment completion rate of 50% (7). The resectional lung surgery to remove a destroyed lung affected by MDR-TB provides an alternative for MDR-TB patients that do not response to chemotherapy (8,9). Previous studies have reported that the successful rates for pulmonary resection combined with anti-TB chemotherapy for MDR-TB ranged from 5% to 96%, indicating the role of surgery in the treatment of MDR-TB remains controversial (10,11).
China has a serious epidemic of MDR-TB, associated with inadequate antibiotic treatment (12). According to the estimation by World Health Organization (WHO), there were 52,000 incident cases of MDR-TB per year in China, accounting for approximate 18% of global burden (1). In China, doctors are preferred to use anti-TB drugs treatment rather than surgery for MDR/XDR-TB patients in process of clinical practice. Hence, there are currently limited data regarding the surgical treatment for MDR- and XDR-TB in China. In this study, we retrospectively analyzed the outcomes of MDR- and XDR-TB patients who received surgical pulmonary resection combined with anti-TB regimens to evaluate the performance of adjective resectional lung surgery for these patients in China.
Methods
Patients
Between October 1992 and October 2012, 21 MDR/XDR patients undergoing pulmonary resection at Beijing Chest Hospital were enrolled in this study. The general criteria for surgical intervention included MDR/XDR-TB, poor response to medical therapy, large cavity in lung, and sufficient pulmonary function to tolerate surgery.
Data collection
After resectional lung surgery, the patients received at least 12 months of anti-TB treatment according to the drug susceptibility profiles. Surgical follow-up was continued for a period of 3 years. The medical records of these patients were retrospectively reviewed to obtain the demographic and clinical characteristics, including age, sex, treatment history, drug susceptibility profiles, chest radiography results, treatment regimens after surgery, and final treatment outcomes. Clinical outcome was classified as cure if the patients completed at least 12 months of treatment with five consecutive monthly negative cultures, while clinical outcome was classified as relapse if the patients exhibited as recurrent disease with a positive sputum culture that matched the drug susceptibility profile of initial Mycobacterium tuberculosis (MTB) isolate and/or the radiographic results revealed that new lesions were appearing at the same side of which pulmonary lobe was resected during the follow-up period.
Microbiological examination
Two sputum samples were collected from each TB patient, and then digested in N-acetyl-L-cysteine-NaOH-Na citrate (1.5% final concentration). After incubation for 15 min at room temperature, the treated samples were neutralized with phosphate buffer (PBS, 0.067 mol/L, pH =7.4), with subsequent centrifugation at 4,000 g for 15 mins. The resuspended sediments were inoculated directly onto Löwenstein-Jensen (L-J) medium. The culture was then incubated at 37 °C for 8 weeks. The MTB positive cultures were used to perform drug susceptibility testing (DST) with the critical concentration method as previously described (6).
Statistical analysis
Chi-squared test and Fisher’s exact test were used to investigate demographic and clinical factors associated with treatment outcome. All statistical analysis was performed with SPSS version 15.0 software (SPSS Inc., Chicago, IL, USA).
Results
A total of 21 patients with pulmonary MDR/XDR-TB undergoing surgical resection were enrolled in this study, including 14 MDR- and 7 XDR-TB. As shown in Table 1, the patients, 15 males and 6 females, had a mean age of 37.2 years (range, 17–44 years). 57.1% (12/21) of these patients were retreated TB cases who had been previously treated with either first- (100.0%, 12/12) or second-line drugs (50.0%, 6/12). Prior to surgery, the median duration of anti-TB treatment was 11.3 months (range, 6–24 months). We further analyzed the pulmonary radiographic presentation. Twenty patients (95.2%) had unilateral cavitary disease, and one patient (4.8%) exhibited bilateral cavitary disease. The most frequent cavitation was located in the left upper lung (38.1%, 8/21). In addition, destroyed lung with reduced lung volume was observed in one patient (4.8%).
Of the 21 total patients, 19 (90.5%) underwent lobectomy, and the other two (9.5%) underwent pneumonectomy due to obvious cavitation in both upper and lower fields of unilateral lung. Medical treatment for TB was performed following surgery, and several drugs, against which some MDR/XDR-TB patients exhibited in vitro resistance, were still been used because of few available treatment options. The treatment outcomes after 3-year follow-up were summarized in Table 1. Overall, 8 patients (38.1%) were cured and 13 patients (61.9%) suffered from unfavorable outcomes. Of 13 patients with unfavorable outcomes, 5 patients (38.5%) died of further progression of TB disease, and 8 patients (61.5%) relapsed who were still receiving anti-TB medical treatment or had treatment failure. We compared the proportions of different clinical outcomes according to various characteristics. As summarized in Table 1, 7 patients (33.3%) experienced the complication, including 5 (23.8%) experiencing lung infection and 2 (6.4%) experiencing bronchial stump fistula. The surgical complication seemed to be more frequently observed among patients with unfavorable outcome (46.2%) versus those with favorable outcome (12.5%), while the statistical analysis revealed no significant different (P=0.17). For patients with different drug susceptibility profiles, only 1 (14.3%) out of 7 XDR-TB patients was cured, compared with 7 (50.0%) out of 14 MDR-TB patients, while the difference was not statistically significant (P=0.17). The proportion of favorable outcome for patients with resistance to any fluoroquinolone (FQ) was 20.0% (2/10), whereas that for patients with susceptibility to FQs was 54.5% (6/11). In addition, the patients with resistance to any second-line injectable drugs (SLID) were more likely to have a poor clinical outcome than those susceptible to SLID (14.3% vs. 50.0%). However, statistical analysis revealed that the differences for these two comparisons were both non-significant (P=0.18 for FQ; P=0.17 for SLID), which may be associated with the small sample size in the present study.
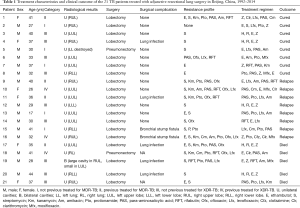
Full table
Discussion
Surgery provides an alternative adjunctive therapeutic approach with a high rate of successful clinical outcome for MDR/XDR-TB patients (10). In the present study, our data demonstrated that the overall cure rate was 38.1% for MDR/XDR patients, which was similar to that from Latvia (47%) (13), while lower than most studies from Peru (63%) (14), South Korea (72%) (15), Japan (89%) (16), and USA (90%) (17). There were several potential reasons responsible for the low cure rate of adjunctive pulmonary surgery for MDR/XDR-TB patients. First, a recent review of 18 case series revealed that the pooled rate of favorable outcome was 89.5% for MDR/XDR-TB patients undergoing adjunctive surgical therapy. However, the median proportion of XDR-TB patient in this review was only 8.8% (85/964) (18), which was lower than that from our report (33.3%). Considering the additional resistance to FQ and SLID, XDR-TB is considered as more dangerous than MDR-TB, thereby determining poor treatment outcomes. Hence, the high rate of XDR-TB may be the major contributor to the low cure rate in our study. Second, due to avoiding the damage of pulmonary surgery, clinicians prefer individualized anti-TB treatment rather than adjunctive resectional lung surgery to treat MDR/XDR-TB patients in Beijing Chest Hospital. The surgical therapy therefore becomes the last choice for MDR/XDR-TB unless treatment failure is observed in response to all potential aggressive chemotherapy. In view of this fact, the patients may suffer from more severe clinical symptoms prior to the delay of surgical treatment, which may be associated with poor cure rate from our observation. Third, most of second-line anti-TB drugs were routinely used for the treatment of MDR-TB patients after 2000 in China (12). Hence, some patients in this study who were enrolled before 2000 could not access the second-line anti-TB regimens, and lack of high quality treatment thus leads to the unfavorable outcome. Fourth, we performed 3-year follow-up for determining the clinical outcome, and the long follow-up period may allow us to monitor more relapse cases.
Due to poor penetration of the TB cavity, it provides an ideal growth niche for TB bacilli from sterilization of anti-TB drugs and host immunity (19). Resectional lung surgery is thus more likely to be an available solution to remove the lung tissue with a large, focal burden of bacilli (19). However, due to the dispersed distribution of TB lesion in the lung, the surgical therapy could not resect all the lung lesions of patients. Therefore, the subsequent treatment with second-line drugs may play the most important role in determining the final clinical outcome for MDR/XDR-TB patients. Several previous literatures have demonstrated that XDR-TB is an indicator for a poor treatment outcome for adjunctive pulmonary surgery (20). In consistent to this finding, we also found that the cure rate of XDR-TB undergoing surgery was not as satisfactory as that of MDR-TB. In view of extensive drug resistance to most antimicrobial agents of XDR-TB, there is an urgent need to improve the availability of new anti-TB drugs, which will offer new opportunities for defeating XDR-TB.
We also realized that there were several limitations in this study. First, the sample size of this study was too small to make conclusions regarding factors associated with clinical outcome. Second, due to the long period of patients’ enrollment, the heterogeneous clinical practice may interfere with the analysis result. In spite of these limitations, this study enhances our understanding on the benefit of surgical resection for MDR/XDR-TB patients.
In conclusion, our data demonstrate that if available, surgical treatment should be considered in MDR/XDR-TB patients in China. The subsequent treatment with second-line drugs may play the most important role in determining the final clinical outcome for MDR/XDR-TB patients.
Acknowledgements
We would like to thank the staffs from Beijing Chest Hospital for their assistance in the patients’ follow-up.
Funding: The study was supported by National Key Project (2008ZX1003015).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Ethical approval was obtained from Beijing Chest Hospital affiliated to Capital Medical University, Beijing, China (ethical approval number: BJXK-2009-13). The study has been registered on the Research Registry (Research Registry UIN: researchregistry1685).
References
- World Health Organization. Global Tuberculosis Report 2015. Available online: http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf
- Calligaro GL, Moodley L, Symons G, et al. The medical and surgical treatment of drug-resistant tuberculosis. J Thorac Dis 2014;6:186-95. [PubMed]
- Lalloo UG, Naidoo R, Ambaram A. Recent advances in the medical and surgical treatment of multi-drug resistant tuberculosis. Curr Opin Pulm Med 2006;12:179-85. [Crossref] [PubMed]
- Dara M, Sotgiu G, Zaleskis R, et al. Untreatable tuberculosis: is surgery the answer? Eur Respir J 2015;45:577-82. [Crossref] [PubMed]
- Caminero JA, Sotgiu G, Zumla A, et al. Best drug treatment for multidrug-resistant and extensively drug-resistant tuberculosis. Lancet Infect Dis 2010;10:621-9. [Crossref] [PubMed]
- Zhang L, Pang Y, Yu X, et al. Linezolid in the treatment of extensively drug-resistant tuberculosis. Infection 2014;42:705-11. [Crossref] [PubMed]
- Papiashvili M, Barmd I, Sasson L, et al. Pulmonary resection for multidrug-resistant tuberculosis: the Israeli experience (1998-2011). Isr Med Assoc J 2012;14:733-6. [PubMed]
- Vashakidze S, Gogishvili S, Nikolaishvili K, et al. Favorable outcomes for multidrug and extensively drug resistant tuberculosis patients undergoing surgery. Ann Thorac Surg 2013;95:1892-8. [Crossref] [PubMed]
- Kang MW, Kim HK, Choi YS, et al. Surgical treatment for multidrug-resistant and extensive drug-resistant tuberculosis. Ann Thorac Surg 2010;89:1597-602. [Crossref] [PubMed]
- Xu HB, Jiang RH, Li L. Pulmonary resection for patients with multidrug-resistant tuberculosis: systematic review and meta-analysis. J Antimicrob Chemother 2011;66:1687-95. [Crossref] [PubMed]
- Madansein R, Parida S, Padayatchi N, et al. Surgical treatment of complications of pulmonary tuberculosis, including drug-resistant tuberculosis. Int J Infect Dis 2015;32:61-7. [Crossref] [PubMed]
- Zhao Y, Xu S, Wang L, et al. National survey of drug-resistant tuberculosis in China. N Engl J Med 2012;366:2161-70. [Crossref] [PubMed]
- Dravniece G, Cain KP, Holtz TH, et al. Adjunctive resectional lung surgery for extensively drug-resistant tuberculosis. Eur Respir J 2009;34:180-3. [Crossref] [PubMed]
- Somocurcio JG, Sotomayor A, Shin S, et al. Surgery for patients with drug-resistant tuberculosis: report of 121 cases receiving community-based treatment in Lima, Peru. Thorax 2007;62:416-21. [Crossref] [PubMed]
- Kim HJ, Kang CH, Kim YT, et al. Prognostic factors for surgical resection in patients with multidrug-resistant tuberculosis. Eur Respir J 2006;28:576-80. [Crossref] [PubMed]
- Takeda S, Maeda H, Hayakawa M, et al. Current surgical intervention for pulmonary tuberculosis. Ann Thorac Surg 2005;79:959-63. [Crossref] [PubMed]
- Pomerantz BJ, Cleveland JC Jr, Olson HK, et al. Pulmonary resection for multi-drug resistant tuberculosis. J Thorac Cardiovasc Surg 2001;121:448-53. [Crossref] [PubMed]
- Kempker RR, Vashakidze S, Solomonia N, et al. Surgical treatment of drug-resistant tuberculosis. Lancet Infect Dis 2012;12:157-66. [Crossref] [PubMed]
- Kaplan G, Post FA, Moreira AL, et al. Mycobacterium tuberculosis growth at the cavity surface: a microenvironment with failed immunity. Infect Immun 2003;71:7099-108. [Crossref] [PubMed]
- Gegia M, Kalandadze I, Kempker RR, et al. Adjunctive surgery improves treatment outcomes among patients with multidrug-resistant and extensively drug-resistant tuberculosis. Int J Infect Dis 2012;16:e391-6. [Crossref] [PubMed]


