We must identify patients at risk for pre-hospital sudden cardiac arrest at the early phase of myocardial infarction
Global coronary heart disease mortality has markedly decreased for the last 4 decades thanks to primary prevention. More than half of the total reduction has been achieved by controlling cardiovascular risk factors (1). Concurrently, effective therapeutic modalities have contributed to reducing further in-hospital fatal events, obtaining a 6–8% reduction (1,2). Meanwhile, out-of-hospital sudden cardiac arrest (SCA) secondary to myocardial infarction remains high, and still represents the majority of all fatal cardiac events (3). Although there is a large amount of literature regarding this sudden and unexpected complication, there is still need for a better understanding of associated risk factors and to identify patients at highest risk for SCA at the pre-hospital phase. Early recognition of the risk of this grim complication could permit a better triage of high-risk patients and consequently improve their outcome.
Concerned by the high pre-hospital mortality in ST-segment-elevation myocardial infarction (STEMI), Karam et al. have recently performed a landmark study aimed at identifying characteristics of STEMI patients presenting with out-of-hospital SCA (4). Using a prospective population-based design, they included patients from the e-MUST (Evaluation en Médecine d’Urgence des Stratégies Thérapeutiques des infarctus du myocarde) registry between 2006 and 2010, which includes all the out-of-hospital STEMI patients managed by the Emergency Medical Service (EMS) in Paris area. In short, it combines data collected by the EMS dispatch call center and the EMS physician in the field. They included patients that were primarily managed by the EMS, alive at EMS arrival, with typical angina and a STEMI-compatible electrocardiogram (ECG). Pre-hospital SCA was defined as a “sudden and unexpected pulseless event without obvious extracardiac cause occurring before hospital arrival and witnessed by the EMS”. Patients with SCA prior to EMS arrival were excluded because of ECG’s poor predictive value for STEMI diagnosis after resuscitation.
Eight thousand one hundred and twelve STEMI patients {median age [interquartile range]: 60 [51–73] years, 78% male} were managed by the EMS within 60 [26–165] minutes after pain onset. Four hundred and fifty-two patients (5.6%) presented EMS-witnessed out-of-hospital SCA, with ventricular tachycardia or ventricular fibrillation as the most frequent initial rhythms (348 patients, 76.9%). Survival in this population was 63.9%, which was significantly lower than reported in the non-SCA population (95.9%). SCA patients with complete data were randomly split into two cohorts, namely a derivation cohort (two thirds of the population) and a validation cohort (one third of the population). From the derivation cohort, pre-hospital risk factors of SCA were identified by multivariate analysis. The e-MUST score was then derived from estimation of the β parameters (regression coefficients) of categorical variables. Individual patient scores were generated. Score performance was then reassessed in the validation cohort to obtain internal validation. Lastly, an external validation was performed in a similar STEMI population from another French region (n=606 with 39 SCA during the study period). Model discrimination was assessed using the area under curve (AUC) the receiver operating characteristics (ROC) curve.
By multivariate analysis, younger age, absence of obesity, absence of diabetes, shortness of breath, and a short delay between pain onset and call to EMS were the main predictors of SCA. A score built from these variables (Table 1) predicted SCA, with the risk increasing 2-fold in patients with a score between 10 and 19, 4-fold with a score between 20 and 29, and more than 18-fold with a score ≥30, compared to those with scores <10. The SCA rate was 28.9% in patients with a score ≥30 compared to 1.6% in patients with a score ≤9. Four groups of score risk was created using 10 points of score {[0–9], [10–19], [20–29], [>30]}. In our opinion, these five simple clinical features, easily obtained by the EMS dispatcher, are of major importance to rapidly implement the means to prevent this fatal event.
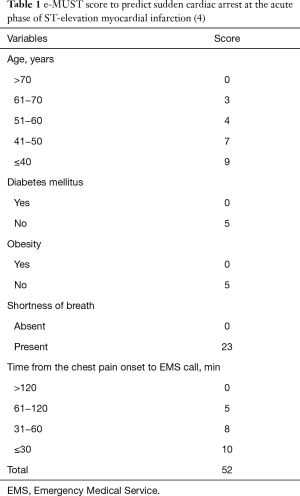
Full table
The main score obtained in the overall population was 18 [13–23], whereas it was only 5 points higher for those with SCA {23 [18–28]}. These slight differences between both groups could lead us to question the e-MUST score performance in intermediate risk populations. Indeed, internal validation and external validation of the e-MUST score demonstrated reasonable but not outstanding discrimination and calibration (c =0.72 and 0.60, respectively). Consequently, selecting a relevant threshold to identify high-risk patients may be complex. When the e-MUST score was ≥30, the specificity was excellent (97%) with, however, low sensitivity (18%). In other words, one out of four patients with an e-MUST score ≥30 will suffer a SCA. With the aim to improve the sensitivity of the score, the authors recommended an e-MUST score of >20 to better identify high-risk patients with a sensitivity and specificity of 65 and 62%, respectively. It is likely that the addition of clinical data easily obtained in the field by the EMS, such as STEMI location on a 12-lead ECG, family history of sudden death, atrial fibrillation, alcohol consumption and hemodynamic situation (5-7), could enhance the accuracy of the model. Because this information can only be obtained after EMS arrival on site, the initial purpose of this score (i.e., early identification of SCA-at-risk patients before EMS dispatching) would be slightly changed.
Based on multivariate analysis results, discrepancies of the weight of each score component appear important. For instance, “shortness of breath” accounts for 23 points, whereas “absence of obesity” or “absence of diabetes” were weighted 5 points each. In other words, feeling “shortness of breath” in the pre-hospital stage during a STEMI would automatically classify the patient as high risk for SCA. Indeed, “shortness of breath” can be considered a surrogate for heart failure and/or myocardial infarct size. In fact, it has been demonstrated that increased Killip class was associated with poorer outcome (8,9). Jabbari et al. identified Killip class > 1 at admission as a predictive factor of ventricular fibrillation (VF) before primary percutaneous coronary intervention in patients with STEMI (7).
Paradoxically, young age, absence of obesity or diabetes, and a short delay between pain onset and call to EMS were the other major risk factors for SCA (Table 1). At first reading, these results might seem a bit surprising. However, previous coronary artery disease is often associated with well-developed collateral flow, which finally reduces myocardial infarct size and mitigates prognosis (10). In addition, better outcome in patients with pre-infarction angina has been reported, which acts as a protective factor against out-of-hospital VF (6,11). Consequently, we can hypothesize that a sudden and complete occlusion of a coronary artery without collateral flow supply may lead in healthy young patients to a proarrhythmic state, a bigger infarct size and a worse prognosis. The impact of “young age” on the risk of SCA in the context of STEMI is still a matter of debate however, with controversial results reported so far (5-7). In the present study, median ages in the SCA and in the non-SCA groups were 57 [48–68] and 60 [51–73] years, respectively. When transformed into categorical variables, patients younger than 40 years of age had the highest risk for SCA {OR 2.5 [1.5–4.4], P<0.0001} whereas the risk progressively decreases with older ages.
Timing is a well-known major determinant of outcome in STEMI patients. However, Karam et al. reported for the first-time short time delay between pain onset and EMS call to be independently associated with increased risk of SCA. This point reinforces the need to get early access to coronary revascularization. Alternative therapeutic implications could arise regarding this issue, such as hastening revascularization with thrombolysis in high-risk patients, even when the recommended time frame can be achieved by percutaneous coronary intervention. Although attractive, randomized trials will be needed in the future to further study this strategy. The e-MUST score might be useful to identify high-risk patients who will need such urgent strategies. Lastly, it should not be considered as a substitute for clinical judgment. ECG features or hemodynamic parameters obtained at EMS arrival may help to better stratify the risk of SCA and set adequate management. In addition, the poor discrimination of this score reported in the external validation (c =0.60) demands the need for further validation.
In conclusion, the e-MUST score offers, through five simple pre-EMS items, a relevant and validated tool for early prediction of SCA in patients with STEMI. Further international prospective studies aiming to evaluate the performance and the benefit of this score are now warranted.
Acknowledgements
S Montero is being funded by a 2016 ESC Clinical Training Grant awarded by the European Society of Cardiology.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Unal B, Critchley JA, Capewell S. Explaining the Decline in Coronary Heart Disease Mortality in England and Wales Between 1981 and 2000. Circulation 2004;109:1101-7. [Crossref] [PubMed]
- Ford ES, Ajani UA, Croft JB, et al. Explaining the Decrease in U.S. Deaths from Coronary Disease, 1980−2000. N Engl J Med 2007;356:2388-98. [Crossref] [PubMed]
- Dudas K, Lappas G, Stewart S, et al. Trends in out-of-hospital deaths due to coronary heart disease in Sweden (1991 to 2006). Circulation 2011;123:46-52. [Crossref] [PubMed]
- Karam N, Bataille S, Marijon E, et al. Identifying Patients at Risk for Prehospital Sudden Cardiac Arrest at the Early Phase of Myocardial Infarction: The e-MUST Study (Evaluation en Médecine d'Urgence des Stratégies Thérapeutiques des infarctus du myocarde). Circulation 2016;134:2074-83. [Crossref] [PubMed]
- Dekker LR, Bezzina CR, Henriques JP, et al. Familial Sudden Death Is an Important Risk Factor for Primary Ventricular Fibrillation. Circulation 2006;114:1140. [Crossref] [PubMed]
- Jabbari R, Engstrom T, Glinge C, et al. Incidence and risk factors of ventricular fibrillation before primary angioplasty in patients with first ST-elevation myocardial infarction: a nationwide study in Denmark. J Am Heart Assoc 2015;4:e001399. [Crossref] [PubMed]
- Jabbari R, Risgaard B, Fosbøl EL, et al. Factors Associated With and Outcomes After Ventricular Fibrillation Before and During Primary Angioplasty in Patients With ST-Segment Elevation Myocardial Infarction. Am J Cardiol 2015;116:678-85. [Crossref] [PubMed]
- Mercado-Martínez J, Rivera-Fernández R, Aguilar-Alonso E, et al. APACHE-II score and Killip class for patients with acute myocardial infarction. Intensive Care Med 2010;36:1579-86. [Crossref] [PubMed]
- Auffret V, Leurent G, Gilard M, et al. Incidence, timing, predictors and impact of acute heart failure complicating ST-segment elevation myocardial infarction in patients treated by primary percutaneous coronary intervention. Int J Cardiol 2016;221:433-42. [Crossref] [PubMed]
- Seiler C, Stoller M, Pitt B, et al. The human coronary collateral circulation: development and clinical importance. Eur Heart J 2013;34:2674-82. [Crossref] [PubMed]
- Gheeraert PJ, Henriques JP, De Buyzere ML, et al. Preinfarction angina protects against out-of-hospital ventricular fibrillation in patients with acute occlusion of the left coronary artery. J Am Coll Cardiol 2001;38:1369-74. [Crossref] [PubMed]


