Do low profile implants provide reliable stability in fixing the sternal fractures as a “fourth vertebral column” in sternovertebral injuries?
Introduction
The sternal fracture (SF) as a posttraumatic injury can be the result of different mechanical mechanism, usually due to direct impact force to the anterior chest wall most commonly related to road traffic accidents with 80% in the sense of a high-velocity trauma (1,2). Sternal fractures are described with a rare incidence of 3–8% out of the whole number of traumatic bone injuries with a mortality of 24–45% associated to concomitant injuries of thoracic organs and less caused by the sternal fracture itself (3-11). However, the most frequently seen concomitant injuries are fractures of the ribs and the vertebral column followed by pulmonary injuries (6).
The second mechanism for sternal fractures is described due to indirect forces to the sternum resulting from a flexion and compression movement of the trunk with a distinctive type of dislocation of the main sternal fragments. The upper part of the sternum is considered to be involved commonly with its typical dislocation posterior to the lower part of the sternum in contrast to direct force injuries which show a dislocation of the corpus sterni posteriorly in the most cases (12).
Meanwhile, the combination of a sternal fracture and the vertebral column, has been already described by several authors in literature (12-16) with the highest incidence in thoracic spine (21.6–38%), followed by the lumbar spine (16.9–27%) (14,17).
Operative stabilization of thoracic and lumbar spine injuries employ posterior instrumentation (51.8%), isolated anterior stabilization (4.6%) and combined posteroanterior procedures (43.5%) (18). This necessitates to be aware of the different types of instability in a vertebral fracture.
Moreover the so called sternum and the rib-complex is presumed to provide additional adjunctive stability in the sagittal biomechanic as the rib cage stiffens the thoracic spine (Table 1) (3). However there is no standardized treatment strategy for the combined injury of the sternum and the spine column (1). A wide range of therapy options for sternal fractures has been published in literature but the role of sternal fractures in the sagittal stability of the trunk has not been addressed well (15). Nevertheless case reports showed severe kyphotic deformities over the course in fatigue fractures of the sternum and its osseous collapsing concomitant to fractures of the thoracic spine column (18).

Full table
Possible options for the treatment of sternal fractures include intramedullary techniques such as Kirschner wires, elastic stable intramedullary nails (ESIN) and wire cerclages which are not supposed to restore the stability of the anterior chest wall from a biomechanical point of view in flexion and compression injuries. Moreover, complications such as an intrathoracic migration of the wires have been described (23). Since bulky implants may lead to discomfort due to sparely soft tissue in front of the sternum, the application of locked plates in a low profile design would be favourable because of an association to a high patient’s convenience (24) and should provide effectual stability as well (25).
From a biomechanic point of view the vertebral body fractures need to be stabilized in case of an involvement of the posterior column which is mostly accompanied by severe sagittal or even rotational instability which could be managed through an posterior approach and sufficient stabilization through an internal fixator (26,27). At the same time the reduction of the usually overlapped and shortened sternum will restore the sagittal alignment of the trunk and subsequently relieve the pressure of the anterior part of the vertebral body. Since the sternal fracture is supposed to be unstable, open reduction with internal fixation employing a locked plate should be the most effective procedure (28-30).
Methods
Study design and patients
A retrospective analysis was carried out on the patients taken to our level I trauma center in the period from November 2011 to October 2014. Included were the patients who had a fracture of the sternum. Two groups were built out of them—SF without a concomitant vertebral fracture and those with a combination of a SF and a vertebral fracture. Those are well known as a sternovertebral injury (SVV). At first the SVV had been divided into three subgroups: SVV with cervical, thoracic and lumbar spine fracture. At second four subgroups out of the SVV with the description of their treatment had been build: conservative treatment, only spine fixation, only sternal fixation and the patients who were stabilized at the sternum and the spine at the same time.
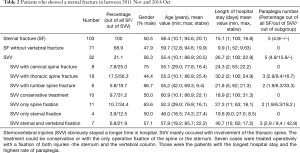
Each of the subgroups is described by their number of patients, their percentage compared to the main group as well as gender, age, length of hospital stay and the number of patients suffering from paraplegia due to the current injury (Table 2).
Full table
A special dedication had been given those with the need of an operative stabilization of the sternum and who were suffering from a vertebral spine injury at the same time.
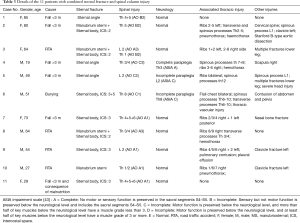
The defined exclusion criteria in these two subgroups (SVV only sternal fixation (n=4; 2 female) and SVV sternal and vertebral fixation (n=7; 3 female)) were patients where the follow-up examinations were not executed (Tables 2,3). SF without concomitant vertebral fracture were not followed up in this study.
Full table
Investigations
All of the patients in the SVV group received a whole-body computed tomography in multisliced technique (“Trauma-Scan”) (Somatom definition AS+, 128 slice, Siemens, Munich, Germany) with a slice thickness of 1.5 mm and multiplanar reconstruction not to miss any concomitant injury. The fractures of the sternum and the vertebral body were precisely checked for instability and they were subsequently typified following the AO spine classification.
The angulation of ground plate to cover plate of all fractured vertebrae identified in initial CT-scan were determined. The patients were in a supine position during the CT scan.
Furthermore the patients were examined for neurological deficits.
Management of the vertebral spine
The vertebral spine injuries had been treated following the recommendations of the AO foundation (31,32). Either conservatively, only dorsal instrumentation or in a dorsal and additional ventral procedure.
Simple wedge or impaction fractures (AO subtype A1) were treated either conservatively or by kyphoplasty.
Fixation of the sternum
Along the lines of the vertebral fractures, the sternal fractures were checked for any displacement and instability as well. After a precise clinical examination, the morphology of the sternal fracture and their exact localization were determined in the CT Scans following a standard algorithm (9).
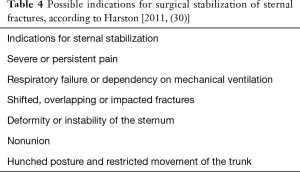
The indication for an operative procedure was set by a senior surgeon following the suggestions from Harston (Table 4) and had been approved by the head of the department in each case (30).
Full table
The procedure was carried out under general anesthesia while the patient was in a supine position. The procedure has been performed as soon as possible after the trauma in patients under stable conditions whereas a stabilization of the trunk was carried out after the recovering from life threat in the patients who were suffering from a polytrauma.
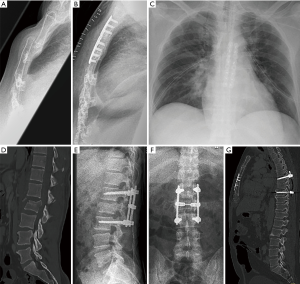
The sternum was stabilized through an open median approach and an anterior locked plate osteosynthesis in a low profile design (Matrix Rib® 1.5 mm thickness, 2.9 mm diameter of screws; DePuy Synthes CMF, Switzerland) following a standard protocol of our department (9). After the elevation of the posterior depressed fragment, the fracture could be reduced exact and subsequently the plate has been fixed with at least three screws to each fragment in order to fix it properly. The screws were fixed in a depth limited drilling technique to avoid mediastinal injuries (29) (Figure 1).

Follow up
All out of the SVV patients were followed up immediately postoperative as well as after one, two, six and twelve weeks. Furthermore the patients were followed up after one and two years additionally. At each time, a clinical examination was carried out including a neurological follow up as well as an X-ray of the spinal column and of the thorax in two planes with a focused look to the consolidation of the fractures and the alignment of the spine column in the sagittal plane while the patient was in standing or in a sitting position.
Statistics
Descriptive statistical analysis was performed by means of Excel® (version 2013, Microsoft Corp., Redmond, USA).
Results
Patients
103 patients showed a fracture of the sternum in the observation period (Table 2). Out of them 32 suffered a combined injury of the sternum and the spinal column. Table 2 shows the main collective in detail as well as the SVV group and its different subgroups. Total of 11 Patients were fixed at their SF—4 in an isolated procedure and 7 in a combined fixation of the SF and the spine injury.
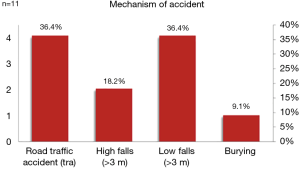
The different trauma mechanisms of the SVV with any sternal fixation were road traffic accidents, high falls (>3 m), low falls (<3 m) and burying by debris avalanche in one case (Case number 6) (Table 3,Figures 2,3).
All of those patients survived until now.
Procedure
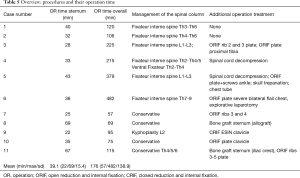
Stabilizing combined injuries of the sternum and the spine column took 39.1 min for the sternal fixation itself and 176 min for combined procedure including the operative treatment which was needed to all concomitant injuries. The spinal injury has been treated first in all cases, followed by the sternal stabilization and stabilization of concomitant rib fractures in 3 cases (pat. 3, 6, 7) (Table 5).
Full table
The patients could be mobilized the day after the operation except those showing paraplegia (pat. nr. 4, 5, 6). The duration of hospitalization ranged from 10 to 59 days with a mean hospitalization time of 31 days (SD =17.1 days) which emphasizes the severity of the combined injuries.
Vertebral injuries und neurologic status
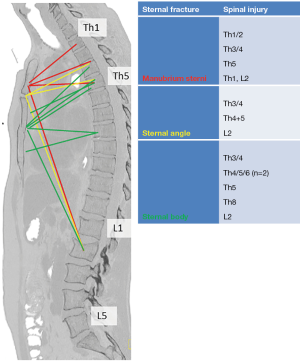
The thoracic spine was involved in 9 cases, the thoracolumbar spine (each involving L2) in three cases whereas 7 out of these patients showed multiple fractures at multiple levels, which were adjacent to each other involving the thoracic spine. There was no fracture with involvement of the lumbar region seen as well as none with involvement of multiple regions of the spinal column (Table 3,Figure 3).
Three out of the patients showed paraplegia below the fractured vertebra (pat. No. 4, 5, 6), two of them incomplete (Case number 5, 6), whereas the other patients remained neurologically intact. All of these three patients were followed at least 24 months up to now. Patient nr. 6 improved to normal neurologic status (ASIA E) in between 6 weeks after operative stabilization whereas patient nr. 5 improved from ASIA B to ASIA D at the time of 12 months after the accident with only minor residual sensory deficit of the lower legs. Patient 4 remained paraplegic but he became able to move to a wheel chair and to drive it independently.
The patients without any neurologic deficit returned to normal life without any limitation in their mobilization. None of them complained about any pain during the follow up.
Any patient showed an anatomic alignment of the vertebral column without secondary dislocation or acquired sagittal deformity caused by further vertebral compression (Figure 4).
All out of the vertebral fractures showed a satisfactory consolidation after 6 weeks and a completely consolidation after 12 weeks. The sagittal profile was examined from a clinical point of view since an X-ray of the whole spine column was not included in the local standards.
Sternal injury
The sternal fractures were located at the manubrium in 4 cases, at the angulus sterni in 3 cases and at the corpus sterni in 7 cases (Table 3,Figure 3). Four out of these patients (Case number 2, 3, 6, 8) showed fractures at two levels of the sternum. Injuries involving the angulus sterni were caused by a downfall in all cases (Case number 1, 4, 5) and showed severe dislocation in each case.
Anterior sternal plating as well as the stabilization of the spine was uneventful in all cases without any implant failures. All of the sternal fractures showed sufficient consolidation without any sign of secondary dislocation or spontaneous collapse of the anterior chest wall following the osteosynthesis. The follow up after 6 weeks showed callus formation at the sternum in all cases and a complete consolidation of the fracture after 12 weeks in all cases.
Concomitant injuries
Concomitant injuries involving the thoracic cage as well as any others are shown in Table 3. Multiple rib fractures were commonly seen (n=9) accompanying the sternovertebral injury, 5 patients suffered from them bilaterally, one of them (Case number 6) showed a severe bilateral flail chest injury due to a crush in conjunction with burying. One patient (Case number 2) sustained a Stanford B-type aortic dissection with an intramural hematoma, which was followed up and treated conservatively.
Discussion
Almost one third out of the patients with SF showed a combined SVV which involved the thoracic spine in more than the half of those patients. Approximately one third out of the SVV were treated conservatively, one third received an exclusive fixation of the vertebral injury whereas a fixation of the sternal fracture had been carried out in another third of the patients with SVV. Those patients with the combined fixation of the sternum and the spine had an exceedingly longer stay in hospital which is accompanied by their higher number and severity of the concomitant injuries (Tables 2,3,5).
Combined SVV injuries mostly result from a flexion-compression mechanism which induced tremendous force impact to the trunk (2,15).
Whilst in 1905 no procedures of sternal stabilization were known yet, Fowler fixed the reduced sternum with a K-wire which was placed transcutaneously (12,33). Meanwhile anterior sternal plating has been described as the most reliable procedure since it can be performed following a standard sequence with high safety and dangerous dislocations of wires intrathoracally are eliminated. At the same time the method of depth limited drilling minimizes the risk of intrathoracal or mediastinal lesions and appropriate plates can be chosen through preoperative planning by computed tomography (9) (Figure 1). Once the sternal fragments have been reduced anatomically the plates provided enough stability at the anterior chest wall, even though they were manufactured in a low profile design (Figures 1,4B,4G). Bottlang focussed on this issue and described the low profile plates to be stable enough while providing some elasticity which induces callus formation and thus accelerates the bone healing (25). Furthermore locked plates with the principle of an internal fixator show the advantage of minimized plate-bone contact and thus they preserve the periostal blood supply (34). In contrast, other reconstruction plates such as pelvic recon one for example provide more stability but they don’t provide any elasticity.
Our experience illustrates the efficacy of the low profile plates without any material failure whereas all out of the patients showed full consolidation of the sternal fracture in between 12 weeks. Moreover the procedure of the sternal fixation could be carried out in a pretty short time (39.1 min; 22–69 min) compared to the overall operation time (176 min; 57–482 min; Table 5) which includes the treatment of all of the concomitant injuries.
Surgical fixation of sternal fractures has a very low number of complications intraoperative as well as postoperative (29,35). Raman et al. investigated proportion of patients with nonunion of the sternum. They saw significant lower non union of the sternum with rigid plate fixation than with wire cerclage. The hypothesis is that a higher biomechanical stability leads to a better bone healing (36). It is obvious that a conservative treatment of sternum fractures has the lowest mechanical stability of all.
All out of the sternal fractures in SVV showed the typical type of dislocation with an override of the corpus atop the manubrium which is consistent to the ones Tarnowsky [1905] and Fowler [1957] reported yet (12,33) (Figure 4A). In consequence the trunk lost its stability in the sagittal plane due to a destruction of the anterior chest wall what subsequently frequently cause concomitant injuries of the vertebral spine in strong impacts to the trunk (12). Current trails show an incidence of 21.6–38% (14,17) as shown introductorily.
Fowler described the types of sternal fractures depending to the force the thoracal complex is exposed to. In opposition to a direct trauma against the anterior chest wall an indirect force is transmitted there through a flexion and compression mechanism of the trunk. Falling on the back and high speed motor vehicle crashes with the passenger’s ejection out of the vehicle are described as the main common reasons for indirect sternal fractures alongside an impact to the neck caused by falling down objects such as hay bales (12,19,33). Our study presents homogeneous causes with falls and high velocity injuries involving motor vehicles (Table 3,Figure 2). Likewise, patient 6 was buried from debris avalanche and subsequently his trunk was strongly hyperextended and distracted which has been survived in rare cases.
The significance of the stability of the anterior chest wall was recognized by several authors before as it stiffens the thoracic cage and the thoracic spine indirectly (2,3,15) (Table 1). Hence the anterior chest wall, inparticular the sternum and rib complex were considered to act like a fourth vertebral column in the stability of the trunk (3). Once it lost its stability the vertebral spine might be affected from significant more pressure and the subsequent risk of kyphotic deformation due to vertebral fractures.
In the case of a burst fracture of the vertebra from a biomechanical point of view the center of rotation at the vertebral spine are the facet joints (37). Once the vertebral body suffers from a burst fracture a ventral stabilization is strongly recommended, such as performing vertebral body replacement through an anterior approach and usually employing a cage system.
All patients in our study who were fixed at the sternum, except one, showed a decrease of kyphotic angulation of the fractured vertebra after operative treatment in the control scan 6 weeks later. One patient (nr. 7) with the increase of angulation underwent no dorsal or ventral stabilization of the injured vertebra because he was suspected not to be suitable for a prone position due to a severe pulmonary disease. Furthermore he suffered from a barrel chest which may lead to an increase of kyphosis in standing or sitting position in comparison to the posttraumatic x-ray which were taken in a supine position.
However, all of these patients showed adequate restoration of their shape of the trunk without any hunched posture. None of them showed any deformity of the anterior chest wall due to a displaced sternum or even a restriction of respiratory chest wall movements. For this reason none of the patients complained about any pain during the follow up. While the patients without any neurologic deficit returned to normal life without any limitation in their mobilization the two patients who showed incomplete paraplegia improved their neurologic status after the procedure. The one patient who showed complete paraplegia could be rehabilitated to a self-determined in independent mobilization in a wheel chair. Driving this wheel chair it might be important to perform powerful movements with the arms which became possible under the basic condition of a stable thoracic cage without any pain or even hunched posture from a dislocated fracture of the sternum and the vertebral column.
This study was carried out with the objective to discuss a possible treatment strategy for patients suffering from a combined sternovertebral injury with the focus on the role of the sternal stability and its management through low profile locked plate osteosynthesis in case of unstable fractures.
Conclusions
Potential complications associated to a sternovertebral injury in patients after blunt thorax trauma are reduced to a minimum through this algorithm. Once the thoracic vertebral column had been involved to an injury concomitant to a sternal fracture the combination of fractures had been evaluated for possible instability. Any instable sternal fractures had been stabilized through two locking plates in parallel and the vertebral column had been stabilized at the same time following the AO rules.
Acknowledgements
None.
Footnote
Conflicts of Interest: Stefan Schulz-Drost has a consultant agreement with DePuy Synthes CMF. Furthermore he is a member of the thoracic expert group of the AO Foundation. No funds were received in connection to the presented study. Sebastian Krinner, Sina Grupp, Pascal Oppel, Andreas Langenbach and Friedrich F. Hennig declare that they have no competing interests.
Ethical Statement: This study does not include research involving human participants or animals. All data has been collected retrospectively.
References
- Homagk L, Siekmann H, Schmidt I, et al. The sterno-vertebral instability - a new classification and therapeutic options. Z Orthop Unfall 2014;152:343-50. [PubMed]
- Gopalakrishnan KC, el Masri WS. Fractures of the sternum associated with spinal injury. J Bone Joint Surg Br 1986;68:178-81. [PubMed]
- Berg EE. The sternal-rib complex. A possible fourth column in thoracic spine fractures. Spine (Phila Pa 1976) 1993;18:1916-9. [Crossref] [PubMed]
- Brookes JG, Dunn RJ, Rogers IR. Sternal fractures: a retrospective analysis of 272 cases. J Trauma 1993;35:46-54. [Crossref] [PubMed]
- Maxwell WA. Sternal fracture: a benign injury? J R Coll Surg Edinb 1988;33:267-9. [PubMed]
- Athanassiadi K, Gerazounis M, Moustardas M, et al. Sternal fractures: retrospective analysis of 100 cases. World J Surg 2002;26:1243-6. [Crossref] [PubMed]
- Yeh DD, Hwabejire JO, DeMoya MA, et al. Sternal fracture--an analysis of the National Trauma Data Bank. J Surg Res 2014;186:39-43. [Crossref] [PubMed]
- Schulz-Drost S, Oppel P, Grupp S, et al. Bony injuries of the thoracic cage in multiple trauma: Incidence, concomitant injuries, course and outcome. Unfallchirurg 2016;119:1023-30. [Crossref] [PubMed]
- Schulz-Drost S, Oppel P, Grupp S, et al. Surgical fixation of sternal fractures: preoperative planning and a safe surgical technique using locked titanium plates and depth limited drilling. J Vis Exp 2015.e52124. [PubMed]
- Trinca GW, Dooley BJ. The effects of mandatory seat belt wearing on the mortality and pattern of injury of car occupants involved in motor vehicle crashes in Victoria. Med J Aust 1975;1:675-8. [PubMed]
- Celik B, Sahin E, Nadir A, et al. Sternum fractures and effects of associated injuries. Thorac Cardiovasc Surg 2009;57:468-71. [Crossref] [PubMed]
- Fowler AW. Flexion-compression injury of the sternum. J Bone Joint Surg Br 1957;39-B:487-97. [PubMed]
- Park WM, McCall IW, McSweeney T, et al. Cervicodorsal injury presenting as sternal fracture. Clin Radiol 1980;31:49-53. [Crossref] [PubMed]
- Oyetunji TA, Jackson HT, Obirieze AC, et al. Associated injuries in traumatic sternal fractures: a review of the National Trauma Data Bank. Am Surg 2013;79:702-5. [PubMed]
- Vioreanu MH, Quinlan JF, Robertson I, et al. Vertebral fractures and concomitant fractures of the sternum. Int Orthop 2005;29:339-42. [Crossref] [PubMed]
- Labbe JL, Peres O, Leclair O, et al. Fractures of the upper transthoracic cage. J Bone Joint Surg Br 2009;91:91-6. [Crossref] [PubMed]
- Scheyerer MJ, Zimmermann SM, Bouaicha S, et al. Location of sternal fractures as a possible marker for associated injuries. Emerg Med Int 2013;2013:407589.
- Reinhold M, Knop C, Beisse R, Audigé L, et al. Operative treatment of traumatic fractures of the thorax and lumbar spine. Part II: surgical treatment and radiological findings. Unfallchirurg 2009;112:149-67. [Crossref] [PubMed]
- Mayba II. Hay balers' fractures. J Trauma 1984;24:271-3. [Crossref] [PubMed]
- Jones HK, McBride GG, Mumby RC. Sternal fractures associated with spinal injury. J Trauma 1989;29:360-4. [Crossref] [PubMed]
- Lund JM, Chojnowski A, Crawford R. Multiple thoracic spine wedge fractures with associated sternal fracture; an unstable combination. Injury 2001;32:254-5. [Crossref] [PubMed]
- Regauer M, Huber-Wagner S, Oedekoven T, et al. Flexible intramedullary nailing of a displaced transverse sternal fracture associated with a flexion-compression injury of the thoracic spine. Spine (Phila Pa 1976) 2010;35:E553-8. [Crossref] [PubMed]
- Chou NS, Wu MH, Chan CS, et al. Intrathoracic migration of Kirschner wires. J Formos Med Assoc 1994;93:974-6. [PubMed]
- Schulz-Drost S, Syed J, Besendoerfer M, et al. Elastic Stable Chest Repair as a Means of Stabilizing the Anterior Chest Wall in Recurrent Pectus Excavatum with Sternocostal Pseudarthrosis: An Innovative Fixation Device. Thorac Cardiovasc Surg 2015;63:419-26. [PubMed]
- Bottlang M, Doornink J, Lujan TJ, et al. Effects of construct stiffness on healing of fractures stabilized with locking plates. J Bone Joint Surg Am 2010;92 Suppl 2:12-22. [Crossref] [PubMed]
- Wang F, He XJ. Long-term effects on health-related quality of life after short-segment pedicle fixation of thoracolumbar fractures without neurologic injury. Zhongguo Gu Shang 2015;28:12-6. [PubMed]
- Kanna RM, Shetty AP, Rajasekaran S. Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J 2015;15:256-64. [Crossref] [PubMed]
- Gloyer MA, Frei HC, Hotz TK, et al. Osteosynthesis of traumatic manubriosternal dislocations and sternal fractures with a 3.5/4.0 mm fixed-angle plate (LCP). Arch Orthop Trauma Surg 2011;131:1261-6. [Crossref] [PubMed]
- Schulz-Drost S, Mauerer A, Grupp S, et al. Surgical fixation of sternal fractures: locked plate fixation by low-profile titanium plates--surgical safety through depth limited drilling. Int Orthop 2014;38:133-9. [Crossref] [PubMed]
- Harston A, Roberts C. Fixation of sternal fractures: a systematic review. J Trauma 2011;71:1875-9. [Crossref] [PubMed]
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013;38:2028-37. [Crossref] [PubMed]
- Vaccaro AR, Schroeder GD, Kepler CK, et al. The surgical algorithm for the AOSpine thoracolumbar spine injury classification system. Eur Spine J 2016;25:1087-94. [Crossref] [PubMed]
- De Tarnowsky G. VII. Contrecoup Fracture of the Sternum. Ann Surg 1905;41:252-64. [Crossref] [PubMed]
- Murphy WM. AO Principles of Fracture Management. 2000;165:25.
- Song DH, Lohman RF, Renucci JD, et al. Primary sternal plating in high-risk patients prevents mediastinitis. Eur J Cardiothorac Surg 2004;26:367-72. [Crossref] [PubMed]
- Raman J, Lehmann S, Zehr K, et al. Sternal closure with rigid plate fixation versus wire closure: a randomized controlled multicenter trial. Ann Thorac Surg 2012;94:1854-61. [Crossref] [PubMed]
- Neumann P, Nordwall A, Osvalder AL. Traumatic instability of the lumbar spine. A dynamic in vitro study of flexion-distraction injury. Spine (Phila Pa 1976) 1995;20:1111-21. [Crossref] [PubMed]