Perfusing chemotherapy by percutaneous lung puncture “holing” for pulmonary tuberculoma—a ten-year single center experience
Introduction
Tuberculoma is a single caseous tuberculosis lesion surrounded by fibrous tissue or spherical lesion formed from obstructed cavity filling with caseous substance, more than 2 cm in diameter. It is round, oval or lobulated, mostly located in the upper lobe of the lung; In imaging, it generally presents spherical massive shadow, clear outline, density inhomogeneity, may contain calcified lesions or photic zone and scattered fibrous proliferative lesions around, which are often called “satellite lesions”. They are relatively stable and can keep a stationary state, but once the body resistance is lowered, the lesions may be worsen, disseminated to form disseminated tuberculosis or liquefied and expectorated to form cavitary tuberculosis (1).
Most drug treatment effects on tuberculoma are relatively poor. After the whole drug treatment, the reduction of lesions is often not obvious, and the possibility of complete drug absorption is even smaller. From January 1999 to December 2009, we treated 54 patients with tuberculoma using the method of drug administration via percutaneous lung puncture-local holing.
Patients and methods
Subjects
Patients who have treated in the Tuberculous Department of Nanjing Chest Hospital from January 1999 to December 2009 were enrolled in this study. Inclusion criteria were as follows: (I) Patients who were diagnosed with tuberculoma, and the diameter was greater than or equal to 2 cm; (II) After 3-6 months of regular anti-TB treatment, tuberculoma size was unchanged; (III) Aged from 18 to 60 years old; (IV) Without serious organic (heart, lung, liver, kidney) diseases.
A total of 54 patients met the above conditions, including 26 males and 28 females, aged from 20 to 60 years (mean age: 33 years). 11 patients with tuberculoma were primarily detected. 35 patients were the disease course form 1 to 5 years, which of 8 patients was more than 5 years; main symptoms were manifested by fever (11 patients), cough (44 patients), expectoration (40 patients) and hemoptysis (10 patients); The concentrated sputum tubercle bacillus smear test indicated positive results in 15 patients, while tuberculosis bacillus culture indicated positive results in 7 patients and drug-resistant tubercle bacillus in 3 patients. The diameter of tuberculoma was from 1.1 cm × 1.2 cm to 6.5 cm × 1.5 cm (mean, 3.6 cm × 2.8 cm). After being treated by lung puncture, the follow-up was 4 to 9 years (mean, 66 months). All patients were informed the risks of lung puncture, such as pneumothorax and bleeding, and they all have signed written informed consent.
In addition, 9 patients with pulmonary tuberculoma were followed up according to conventional medical therapy due to fear of lung puncture risks or improvement in the general situation, including 7 males and 2 females. Their average age was 32 years old.
Treatment
Patients themselves were considered as the control group. Conventional treatment was conducted for 3 to 6 months firstly. Patients who had no changes in the size of tuberculoma underwent drug administration via percutaneous lung puncture. Firstly, percutaneous lung puncture was conducted, and the center of the tuberculoma was pugged and poked up and down for several times. Lesion contents were drawn out for pathological examination and acid-fast staining, known as “holing”. Then, drug injection via percutaneous lung puncture in tuberculoma was conducted, 1 or 2 times every week, 10 times as a course. In 54 patients, there were 26 in the prone position, 20 in the supine position and 8 in the lateral position. They were punctured for a total of 468 times. Specific operations included the treatment position, inserting depth and angle of the needle were determined according to CT. It was followed by routine skin disinfection and hole towel spreading. 2% lidocaine 5 mL was injected for local anesthesia to the pleura. After a 21-23 G puncture needle was inserted into the tuberculoma, INH 0.1 g and AMK 0.2 g were smoothly injected, and the needle was quickly pulled out. After pneumothorax was excluded by CT, patients came back to the ward for two-hour repose. After the course of treatment, they were continued to be treated for 3 to 6 months according to the original plan.
Efficacy determination
A comprehensive analysis was conducted including sputum examination for tubercle bacillus, clinical manifestations and changes in chest imaging to determine the therapeutic effect. If results of three consecutive months of sputum smear and tuberculosis bacillus culture were negative, it was defined as negative conversion. While the disappearance or relief of symptoms indicated an effective treatment, in contrast, no changes or worsening of symptoms suggested an ineffective treatment. Plain CT scan results of the tuberculoma diameter was treated as significantly reduced if it narrowed over 1/2 but as unchanged if no change in the tuberculoma diameter as increased if the diameter increased; and as disappearing if the tuberculoma disappeared.
Results
Effect evaluation
In 54 patients, 15 patients showed positive smears, after 2 months of treatment, 13 showed negative conversion; 3 of 39 patients with negative smears showed positive conversion; in tubercle bacillus culture, all 7 patients with positive results showed negative conversion. They were reexamined after one year, 4 of 5 tubercle bacillus-positive patients showed negative conversion, and two consecutive tubercle bacillus cultures showed one tubercle bacillus-positive patient were negative, and patients were generally well, with so-called dead tubercle bacillus. Tuberculoma of 21 patients disappeared, which was significantly in 12 patients. After drug administration via lung puncture, the density of tuberculoma increased in varying degrees, even calcified in 5 patients. All 10 patients with hemoptysis were cured. The diameter of the tuberculoma was at the fleck of calcification (about 5.0 cm × 1.9 cm), with an average of 1.7 cm × 1.1 cm. A total of 34 patients were followed up for 5 years or more, the disappearance rate of tuberculoma was 47% (16/34). No recurrence appeared. Nine patients with tuberculoma who have undergone routine treatment were followed up for 2 to 7 years, one with tuberculoma reduction, five ones with no changes in tuberculoma, and one with increased tuberculoma, two ones with cavity formed and positive for sputum tubercle bacillus smear).
The effective treatment for tuberculoma was defined as negative conversion of tubercle bacillus, disappearance or calcification of tuberculoma. After the treatment course in the group, the negative conversion rate of tubercle bacillus was 87% (13/15), and tubercle bacillus culture- negative conversion rate was 100% (7/7). After one year, the negative conversion rate of tubercle bacillus was 100%, and 61% (33/54) of tuberculoma significantly reduced, of which, the disappearance rate of tuberculoma was 40% (21/54).
Side effects
In 54 patients, five cases had pneumothorax with lung compression rate less than 20%, which didn’t affect the continued treatment. Four patients had slight hemoptysis, and were cured without special treatment. The body temperature of six patients increased, in whom three ones were transient without treatment, three ones had high fever over 38.5 °C, and increased white blood cells. Their temperature dropped to normal within 3 days after the anti-inflammatory symptomatic treatment.
Typical cases
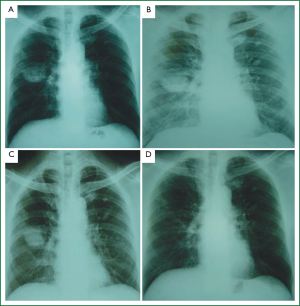
The first case, male, 45 years old, who had a 5-year history of TB was hospitalized because of massive hemoptysis. After the anti-tuberculosis symptomatic treatment by HERV, his hemoptysis was ceased gradually. Triple concentrated sputum tubercle bacillus smear tests all showed negative results. He was treated 9 times by drug administration via percutaneous lung puncture. The tuberculoma diameter was 6 cm × 4.2 cm (Figure 1A) and decreased to 6 cm × 3.8 cm (Figure 1B) after injection and was 4.6 cm × 3.1 cm (Figure 1C) one year later, two years later, they were reexamined and was found no tuberculoma (Figure 1D) and negative concentrated sputum tubercle bacillus smear test as well as the sputum mycobacterium tuberculosis culture. He was followed up for 10 years and was in good condition.
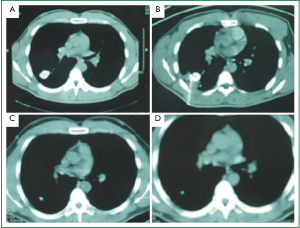
The second case, male, 31 years old, who had a one-year history of pulmonary tuberculosis was hospitalized due to drug-induced hepatitis. ALT was 295 U/L, AST was 79 U/L, and three times of concentrated sputum tubercle bacillus smear tests showed negative results. He was treated 10 times by drug administration via percutaneous lung puncture. Before injection, the tuberculoma diameter was 2.5 cm × 2 cm (Figure 2A), after 6 times of injection, it was 2.5 cm × 2 cm (Figure 2B), but crevasse appeared at the punctured site. Five months after injection, tuberculoma disappeared and became edge-blurred flecks of calcifications (Figure 2C), with normal liver function. One year later, it became flecks of calcifications (Figure 2D). The concentrated sputum tubercle bacillus smear test always showed negative results. They were followed up for 9 years and in good condition.
The third case, female, 47 years old, who had a half-year history of pulmonary tuberculosis with tuberculosis pleurisy of the left side and a history of hepatitis B and hepatitis C was hospitalized due to liver function abnormalities. The patient was allergic to rifampicin, ALT was 81 U/L, and the concentrated sputum tubercle bacillus smear test showed negative results. Pasiniazide, ethambutol and levofloxacin were administered to her for anti-tuberculosis treatment. And she was treated 10 times by drug administration via percutaneous lung puncture. Before injection, the tuberculoma diameter was 3.2 cm × 3.2 cm (Figure 3A). After 10 times of injection, it was 2.3 cm × 1.8 cm (Figure 3B). After half a year, it was 1.5 cm× 1.5 cm (Figure 3C), after 1 year, tuberculoma completely disappeared (Figure 3D), and liver functions were normal.

Discussion
Spherical tuberculose lesions in the lungs are called pulmonary tuberculoma. Spherical tuberculose lesions occur in the visceral and parietal pleura are called pleural tuberculoma. In different types of spherical tuberculose lesions, the tubercle bacillus-positive rate can be up to 10-64%. Clinical experience has shown that: most medical treatment effects on tuberculoma are relatively poor, after the whole anti-tuberculosis treatment, lesions are often not obviously reduced. The possibility of complete drug absorption is even smaller. So these patients should also be regularly reexamined though the treatment has been finished, especially those with tuberculoma. Because the immunity will be weakened or allergic reaction increased once the body is affected by certain factors, tubercle bacillus in tuberculoma can be re-active and multiply, tuberculoma capsule is damaged. The lesion extends to the surrounding lung tissue or is caseated liquefied, dissolved and penetrates the bronchia to discharge, thus forming a cavity. Tubercle bacillus can also spread to the lung or pleura via lymph or bronchia, causing new lesions, worsening tuberculosis. Therefore, the way to control and treat tuberculoma becomes another anti-tuberculosis problem.
Porkhanov et al. diagnosed and treated 98 patients with single or multiple tuberculoma using thoracoscope, in whom 14 patients underwent lobectomy and 23 patients had incomplete pneumonectomy. As a result, the rate of postoperative complications was 7.5%, and three patients had thoracotomy (2). Some recent studies showed that (3) surgical resection of tuberculoma by video-assisted thoracoscopic surgery (VATS) could effectively cure tuberculoma with 6-12 months anti-tuberculosis treatment after surgery. Thus, thoracoscopic surgical resection was a good way for the diagnosis and treatment of tuberculoma. But the surgery is a major trauma for patients.
Dai et al. (4) reported the method and effect of fibre bronchoscope on the treatment of tuberculoma, that is, under direct X-ray vision, after the fibre bronchoscope was inserted into the lobe and segmental bronchi where the tuberculoma located, an biopsy forceps was put in to probe the tuberculoma, loosed necrotic tissue in it, abstracted with an aspirator under negative pressure and the inner necrotic tissue was clipped out. In that way, the clinical efficacy could reach 48%, tuberculoma completely disappears (5/30) within 1-3 months, in whom one reduced, eight ones had cavities but three ones had closed cavities after the treatment course. Tuberculoma mostly present in the periphery of the lung so that fibre bronchoscope is hard to be inserted deeply, thus limiting the application of this method.
Drug administration via percutaneous lung puncture for tuberculoma is a new therapy we have created over more than 10 years. The underlying mechanism might be that tuberculoma is coagulated caseous necrotic and is covered with a layer of fibrous capsule. Because of the lack of blood supply and hypoxia in the tuberculoma, remnant tubercle bacillus relies on lipid metabolism by surrounding lipids and breathing by nitrogen to survive, in a stationary or sleeping state (5). Drugs are difficult to enter the tuberculoma to kill it. Holing administration refers to percutaneous lung puncture was conducted firstly to mash central lesions in the tuberculoma, contents were extracted from lesions, so a tiny space was formed in the tuberculoma, thus being conducive to the infiltration of blood and oxygen supply, thereby activating stationary tubercle bacillus. After the re-injection of anti-tuberculosis drugs by percutaneous lung puncture, high concentrations of anti-tuberculosis drugs can kill tubercle bacillus in tuberculoma, including multidrug-resistant tubercle bacilli (6), tuberculoma was completely cured. We have cured a patient with extensively drug-resistant tuberculosis using this method successfully (7). In the group, after one year of treatment of tuberculoma, the negative conversion rate of tubercle bacillus is up to 100%, the disappearance rate of tuberculoma was 40%. In whom, 34 patients were followed up for 5 years. The disappearance rate of tuberculoma is up to 47%, with no recurrence. After another nine patients with tuberculoma were treated by conventional medical anti-tuberculosis and were followed up for 2-7 years, with 33% recurrence rate of tuberculosis.
Isoniazid is a complete bactericidal drug, easy to penetrate phagocytic cells and can kill intracellular or extracellular Mycobacterium tuberculosis with fast or slow growth and reproduction in acidic or alkaline environment. It is the first choice for the treatment of tuberculosis (8). Amikacin has a strong anti-mycobacterium tuberculosis effect. It is mainly used for streptomycin-resistant patients. Its mechanism of action is similar to that of kanamycin, with higher bactericidal activity against mycobacterium tuberculosis and less side effects.
Because tuberculoma is solid, drugs penetrate in the tuberculoma wrapped by fibrous tissue after injection. High concentrations of drugs could achieve a good bactericidal effect. Hemoptysis and pneumothorax are sporadic, and the symptoms are very mild, and they are significantly reduced compared to complications such as pneumothorax caused by percutaneous puncture of small pulmonary nodules (9). And fever is rare, this maybe because the reaction in the whole body of toxins generated by drugs killing tubercule bacillus. We found that all patients who had postoperative fever were easier to had rupture and disappear tuberculoma. For patients with hepatitis and abnormal liver function, little or no anti-tuberculosis drugs can be used, and the effect is also very good.
In conclusion, the treatment of administration via percutaneous lung puncture in tuberculoma works effectively, with less side effects, which could be a noval, safer therapy with better short- and long-term effects for tuberculoma.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Meng LL. eds. Self-control for tuberculosis. Beijing: Golden Shield Press, 2003:166-7.
- Porkhanov VA, Poliakov IS, Kononenko VB, et al. Videothoracosopy in diagnosis and surgical treatment of tuberculosis. Khirurgiia (Mosk) 2002;6:14-6. [PubMed]
- Hsu KY, Lee HC, Ou CC, et al. Value of video-assisted thoracoscopic surgery in the diagnosis and treatment of pulmonary tuberculoma: 53 cases analysis and review of literature. J Zhejiang Univ Sci B 2009;10:375-9. [PubMed]
- Dai XY, Cao XY, Wu MR, et al. Treatment effects of tuberculosis ball 30 patients with tuberculoma observed using fiber bronchoscope. Journal of Wuhan Professional Medical College 2000;3:18-9.
- Wu SZ, Song JF. Pathogenesis of Mycobacterium tuberculosis and immunity against it. Chinese Journal of Tuberculosis and Respiratory Diseases 2003;26:101-3.
- Yang SH, Mao HJ, Shi XD, et al. Treatment of drug administration via percutaneous lung puncture for multidrug-resistant cavitary tuberculosis. Chinese Journal of Tuberculosis and Respiratory Diseases 2006;29:131-2.
- Yang SH, Zhan P, Sun M, et al. Perfusing chemotherapy by percutaneous lung puncture in the treatment of extensive drug resistant pulmonary tuberculosis. J Thorac Dis 2012;4:624-8. [PubMed]
- Zhang DR. eds. Diagnosis and treatment of tuberculosis. Beijing: People’s Medical Publishing House, 2003:72-3.
- Gu JH, Sun WG, Lu DY. CT-guided percutaneous needle biopsy of small pulmonary nodules in 48 patients. Jiangsu Medical Journal 2001;27:878-9.


