Socioeconomic impact of asthma, chronic obstructive pulmonary disease and asthma-COPD overlap syndrome
Introduction
Chronic airway disease is one of the most common chronic diseases, which is responsible for current and future socioeconomic burden (1). Asthma and chronic obstructive pulmonary disease (COPD) are major airway diseases and have unique distinctive features (2). However, clinicians often encounter patients presenting overlapping symptoms of both diseases. Now asthma-COPD overlap syndrome (ACOS) is widely used to describe such a condition sharing both features of asthma and COPD (3-5). ACOS is simply defined as coexistence of incompletely reversible airway obstruction and airway hyper-responsiveness. Subjects with ACOS tend to have increased risk of exacerbation and poor quality of life (6-8). High economic burden of ACOS was demonstrated compared to those of asthma and COPD (9-13). This study was to measure impact of ACOS particularly on healthcare utilization and medical cost using data from the fourth South Korean National Health and Nutrition Examination Survey (KNHANES IV) (14) and National Health Insurance claims (15,16).
Methods
Data source and ethical considerations
This study examined data from KNHANES IV and National Health Insurance claims.
KNHANES is a national survey performed every three years, which began in 1998. The purpose of KNHANES is to assist the establishment of a national health policy and to develop a knowledge base for the evaluation of health risk factors and health indicators. The fourth survey was later converted into a year-round investigation to improve weaknesses in survey areas and the quality of results gained. The first round [2007], the second round [2008], and the last round [2009] of the KNHANES IV have been conducted (14). KNHANES IV used stratified, multi-stage, clustered probability design to select a representative sample of non-institutionalized citizens from the Korean population (14). KNHANES IV consisted of Health Interviews, Health Behavior Surveys, Health Examination Studies, and Nutrition Surveys. More details on the research methodology used to gather and analyze the KNHANES IV data are available on the National Health and Nutrition Examination Survey website (https://knhanes.cdc.go.kr/knhanes/index.do).
The National Health Insurance claims data was provided by the Korean Health Insurance Review and Assessment Service (HIRA), which was established to review claims data and assess healthcare in Korea; it is under the responsibility of a single agency independent from insurers, providers, and other interested parties. All Koreans are covered under the national health insurance system, and the HIRA database contains all information regarding submitted claims and prescriptions.
This study analyzed respondents over the age of nineteen who participated in the spirometry test of the KNHANES IV and who provided responses to questions on whether they had experienced wheezing in the past year. Subjects who did not have missing covariates were selected, and their claims data, collected from January 1 to December 31 of the years when KNHANES IV was conducted, was examined in conjunction with the KNHANES IV data.
The Public Institutional Review Board approved the present study (PIRB11-025-2).
Study population selection
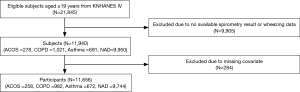
A total of 21,845 respondents, over the age of nineteen, participated in the KNHANES IV. This study examined a total of 11,940 subjects who had participated in the spirometry tests and had provided a response regarding experiences of wheezing during the one year prior to the survey. Two hundred-eighty four subjects with missing covariates were excluded from the final data set, and the remaining 11,656 respondents were analyzed for the study. Figure 1 shows the details on the selection of the study population.
Measures
Definition of airway diseases
Subjects were categorized into four groups: ACOS group, COPD group, asthma group, and group with no airway disease (NAD). ACOS was defined as having FEV1/FVC <0.7 and experiencing wheezing during the twelve months prior to the survey. COPD was defined as having FEV1/FVC <0.7 and no wheezing during the twelve months prior to the survey. Asthma was defined as having FEV1/FVC ≥0.7 and experiencing wheezing during the twelve months prior to the survey. NAD was defined as having FEV1/FVC ≥0.7 and no wheezing.
Subjects’ characteristics
The variables of the subjects’ characteristics were age, gender, body mass index (BMI), spirometry, presence or absence of chronic bronchitis, smoking status, education, and household income level. BMI is obtained by dividing a subject’s weight by the square of the subject’s height, and this study divided subjects into three BMI groups: underweight (<18.5 kg/m2), normal (≥18.5 and <25 kg/m2), and overweight (≥25 kg/m2). Chronic bronchitis was defined as having cough or sputum production for over three months during the twelve months prior to the survey and had a cough or sputum that lasted over two years. Subjects’ smoking status was divided into current smokers, former smokers, and never smokers. Subjects’ education level was categorized as <12, 12, and >12 years. Household income level was divided into four groups based on their average total household income: 1st, 2nd, 3rd and the 4th quartile; the 1st quartile consisted of the lowest income group, while the 4th quartile was composed of subjects with the highest income.
Healthcare utilization
Healthcare utilization was measured by the medical cost and the duration (days) of medical service utilized per person. The medical cost was calculated as medical expenses (including insurance benefits and patients’ copayments), including outpatient and hospitalization fees. The duration of medical service use included the hospitalization period (including intensive care unit hospitalization days and emergency room days) and number of outpatient visits.
Statistical analyses
Data was analyzed using the SAS statistical program [ver. 9.2 (SAS Institute)]; details of the analytical methods are listed below.
First, frequencies, percentages, and mean ± standard deviation (SD) were calculated to enable comparison of subjects’ baseline characteristics among four groups; the chi-squared test was used for categorical (discrete) variables and ANOVA was used for continuous variables.
Second, Chi-squared test was applied to assess differences in utilization or non-utilization of healthcare services among four groups; ANOVA was used to analyze differences in length of healthcare utilization (number of days) and medical costs.
Lastly, linear regression analysis was applied to assess the impact of airway diseases and subjects’ characteristics on length of healthcare utilization and medical costs.
Results
Among a total of 11,656 subjects, ACOS comprise 2.2% [258]; COPD, 8.4% [982]; asthma, 5.8% [672] and NAD, 83.6% [9,744].
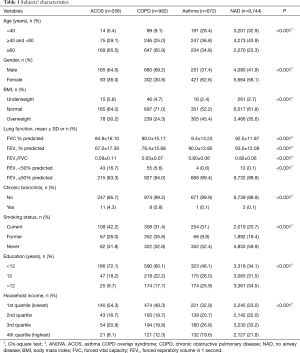
Four groups showed differences in age, gender, BMI, lung function, the presence or absence of chronic bronchitis, smoking status, education and household income level (P<0.001 respectively, Table 1). In terms of age, both ACOS and COPD groups were most common among those above sixty, while both asthma and NAD groups were most common among subjects between 40 and 60 (P<0.001). There were more males than females within both ACOS and COPD groups, and it was the opposite in both asthma and NAD groups (P<0.001). With regards to BMI, underweight is relatively common in both ACOS and COPD groups, and overweight is common in asthma group. Among four groups, ACOS group showed the worst lung function parameters as well as the highest smoking rate (68.2%). Moreover, current smoking rate was the highest. Although only 25 subjects had chronic bronchitis based on responses to questionnaires, most of them (n=19) belonged to both ACOS and COPD groups. ACOS group showed the lowest education levels, the next was COPD group and the third was asthma group (P<0.001). Household income showed similar trend to education level.
Full table
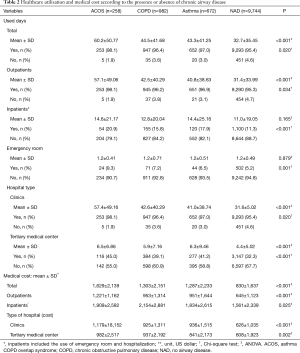
There were statistically significant differences among four groups in terms of the total number of days per person in healthcare utilization, outpatient care utilization, utilization of clinics, and utilization of tertiary medical centers from January 1 to December 31 of the year KNHANES IV was conducted (P<0.001, respectively, Table 2). While ACOS group recorded the top in both of total used days and total medical costs (P<0.001), inpatient medical cost was the highest in COPD group compared to the others (P=0.025).
Full table
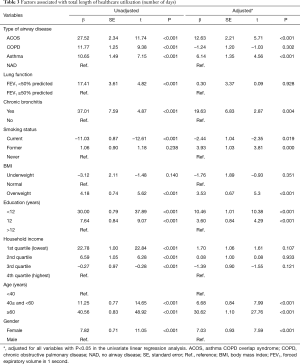
When a univariate regression analysis was applied to know factors affecting the length of healthcare utilization, it revealed that the presence of airway disease, FEV1 <50% predicted, the presence of chronic bronchitis, current smoking, overweight, lower education levels, lower household income levels, old age, and female gender are significantly associated with longer duration of health hare utilization (Table 3). To observe whether the type of airway disease had a specific impact on the length of healthcare utilization, all factors influencing the length of healthcare utilization from the univariate regression analysis were included in the multiple regression analysis; results showed that ACOS group (β=12.63, SE =2.21, P<0.001) and asthma group (β=6.14, SE =1.35, P<0.001) were significantly associated with higher number of days in healthcare utilization.
Full table
When the same approach was applied to the medical costs, univariate analyses showed that the type of airway disease, FEV1 <50% predicted, the presence of chronic bronchitis, current and former smokers, overweight, lower education levels, lower household income levels, and old age were associated with higher medical costs (Table 4). To observe whether the type of airway disease had a specific impact on medical costs, all factors influencing medical costs from the univariate regression analysis were included in the multiple regression analysis; results showed that ACOS group (β=350,475.88, SE =131,289.38, P=0.008) and asthma group (β=386,876.81, SE =80,026.83, P<0.001) were associated with higher medical costs.
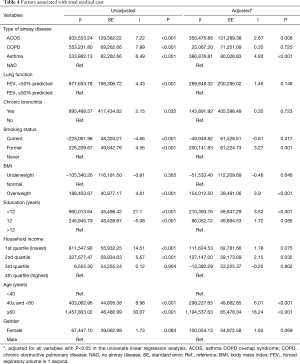
Full table
Discussion
This study clearly showed large impact of ACOS on healthcare utilization, which existed independently after multiple adjustments with possible confounding factors. Although Rhee et al. (11) reported high medical utilization of ACOS in Korea, they used only the National Health Insurance claim data, which did not include spirometry data and history of smoking and chronic bronchitis. Therefore, their definitions of COPD and ACOS were not based on spirometry, but on diagnosis codes and medication records. Additionally Rhee et al. compared healthcare utilization of ACOS only with that of COPD, not with that of asthma. In contrast, our study applied spirometric criteria to define airway disease and used data from a representative sample of non-institutionalized citizens from the Korean population by stratified, multi-stage, clustered probability design. These support that our results could have representativeness.
ACOS is known to encompass severe asthma with airway remodeling and COPD with bronchial hyper-responsiveness. Naturally healthcare utilization and medical cost of ACOS group are expected to be higher than those of asthma and COPD. Accordingly, our study showed that all the medical cost and total length of healthcare utilization were the highest in ACOS group except inpatient medical cost, which was the highest in COPD group. Healthcare utilization and cost of COPD group were higher than those of asthma group, which is consistent with previous studies conducted in the other countries (9,10,17). However, our multiple regression analyses failed to show significant impact of COPD on health care utilization and medical cost though impacts of both ACOS and asthma kept significance. There were several possible reasons. Our definitions of ACOS, COPD, and asthma are not the same as those of previous studies. Bronchial hyper-responsiveness was based on self-reported wheezing and spirometry was not performed after bronchodilation, which made some heterogeneity even in the same group. Our definition of asthma might exclude subjects with recently well-controlled asthma, who were probably allocated to NAD group. Our asthma group presented wheezing in a previous year, which might make them to need healthcare utilization. Another reason is that these data were from national survey through representative sampling, which included subjects with relatively mild disease. Subjects with severe disease hardly participate survey. In our COPD group, only 5.6% had severe airflow limitation, defined as FEV1 <50% predicted. In clinical practice, patients with FEV1 ≥50% predicted rarely complain shortness of breath particularly if they are old and do not need physical activity. Maybe our asthma group represent recently poorly controlled asthma, and our COPD group mainly consists of subjects with mild to moderate airflow limitation and no symptoms. Furthermore, considering several features such as old age, high smoking rate, poor lung function, low education levels and low household income of ACOS group, most of them are likely to have severe COPD with frequent exacerbations or longstanding poorly-controlled asthma. Combination of low FEV1 and airway hyper-responsiveness is likely to need medical attention. A previous study using the same definitions as those in our study also demonstrated that ACOS group reported the worst self-rated health status, but COPD group showed better than asthma group (8).
This study has several limitations. First, KNHANES was not exclusively intended to investigate chronic airway disease. Lung function was not measured in all participants, which contributes to selection bias. Total participation rate was not so high, and only participants with eligible spirometry results were included. Severely ill case could not be enrolled due to unsuitable data, though different sampling weights provided by KNHANES IV were applied to minimize the healthy worker effect (18). Second, bronchial hyper-responsiveness was defined only based on responses to questionnaires. This may result in misdiagnosis of an individual case and heterogeneity of subjects in the same group. Subjects with recent COPD exacerbations could have been misdiagnosed as having ACOS. Some asthmatics with poor compliance might have been misclassified to ACOS. Subjects with well-controlled mild asthma could have been considered to have NAD. COPD group may include subjects with well controlled ACOS. This sample bias might contribute to higher medical costs for the ACOS and asthma groups than those for the COPD. Nevertheless, self-assessment methods have been widely used in previous general population-based studies because of their feasibility (8,19,20). Although the definition of ACOS has been widely variable, the prevalence of ACOS in the current study is similar to that in previous studies (3,5), which estimated 15% to 45% of the population with obstructive airway disease. Our prevalence of ACOS was 21% [258/1,240] of subjects with airflow limitation. Additionally characteristics of our three groups are very consistent with previously described those of ACOS, asthma, and COPD. Third, only direct medical cost and length of healthcare utilization were shown, though indirect cost, loss of working days and mortality are very important to evaluate socioeconomic burden of disease.
Despite these limitations mentioned, this study clearly showed high impact of ACOS on healthcare utilization after multiple adjustments. Although our analysis was not complete, several important confounding factors such as age and socioeconomic factors were adjusted. These socioeconomic factors cannot be easily obtained in gathering clinical data, which was one of our strengths.
The current study highlights that the impact of ACOS on socioeconomic burden independently exists under multiple adjustments with other confounding factors. ACOS group needs appropriate socioeconomic supports as well as careful management by respiratory experts until evidence-based guidelines for management of ACOS will be developed.
Acknowledgements
Funding: This work supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2010-0027945).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The Public Institutional Review Board approved the present study (PIRB11-025-2).
References
- Sullivan SD, Ramsey SD, Lee TA. The economic burden of COPD. Chest 2000;117:5S-9S. [Crossref] [PubMed]
- Barker BL, Brightling CE. Phenotyping the heterogeneity of chronic obstructive pulmonary disease. Clin Sci (Lond) 2013;124:371-87. [Crossref] [PubMed]
- Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax 2009;64:728-35. [Crossref] [PubMed]
- Postma DS, Rabe KF. The Asthma-COPD Overlap Syndrome. N Engl J Med 2015;373:1241-9. [Crossref] [PubMed]
- de Marco R, Pesce G, Marcon A, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One 2013;8:e62985. [Crossref] [PubMed]
- Hardin M, Silverman EK, Barr RG, et al. The clinical features of the overlap between COPD and asthma. Respir Res 2011;12:127. [Crossref] [PubMed]
- Kim MA, Noh CS, Chang YJ, et al. Asthma and COPD overlap syndrome is associated with increased risk of hospitalisation. Int J Tuberc Lung Dis 2015;19:864-9. [Crossref] [PubMed]
- Chung JW, Kong KA, Lee JH, et al. Characteristics and self-rated health of overlap syndrome. Int J Chron Obstruct Pulmon Dis 2014;9:795-804. [PubMed]
- Shaya FT, Dongyi D, Akazawa MO, et al. Burden of concomitant asthma and COPD in a Medicaid population. Chest 2008;134:14-9. [Crossref] [PubMed]
- Jacobson L, Hertzman P, Lofdahl CG, et al. The economic impact of asthma and chronic obstructive pulmonary disease (COPD) in Sweden in 1980 and 1991. Respir Med 2000;94:247-55. [Crossref] [PubMed]
- Rhee CK, Yoon HK, Yoo KH, et al. Medical utilization and cost in patients with overlap syndrome of chronic obstructive pulmonary disease and asthma. COPD 2014;11:163-70. [Crossref] [PubMed]
- Andersén H, Lampela P, Nevanlinna A, et al. High hospital burden in overlap syndrome of asthma and COPD. Clin Respir J 2013;7:342-6. [Crossref] [PubMed]
- Gerhardsson de Verdier M, Andersson M, Kern DM, et al. Asthma and Chronic Obstructive Pulmonary Disease Overlap Syndrome: Doubled Costs Compared with Patients with Asthma Alone. Value Health 2015;18:759-66. [Crossref] [PubMed]
- Kweon S, Kim Y, Jang MJ, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014;43:69-77. [Crossref] [PubMed]
- Lim SJ, Kim HJ, Nam CM, et al. Socioeconomic costs of stroke in Korea: estimated from the Korea national health insurance claims database. J Prev Med Public Health 2009;42:251-60. [Crossref] [PubMed]
- Lee YH, Yoon SJ, Kim EJ, et al. Economic burden of asthma in Korea. Allergy Asthma Proc 2011;32:35-40. [Crossref] [PubMed]
- Blanchette CM, Gutierrez B, Ory C, et al. Economic burden in direct costs of concomitant chronic obstructive pulmonary disease and asthma in a Medicare Advantage population. J Manag Care Pharm 2008;14:176-85. [Crossref] [PubMed]
- Yoo KH, Kim YS, Sheen SS, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology 2011;16:659-65. [Crossref] [PubMed]
- Xuan W, Peat JK, Toelle BG, et al. Lung function growth and its relation to airway hyperresponsiveness and recent wheeze. Results from a longitudinal population study. Am J Respir Crit Care Med 2000;161:1820-4. [Crossref] [PubMed]
- Arif AA, Delclos GL, Lee ES, et al. Prevalence and risk factors of asthma and wheezing among US adults: an analysis of the NHANES III data. Eur Respir J 2003;21:827-33. [Crossref] [PubMed]


