A segmental labeling technique for non-intubated thoracoscopic anatomical segmentectomy
Introduction
Precise pulmonary segmentectomy as lung sparing surgery has been recognized as an alternative of lobectomy for early-stage lung cancer or undiagnosed small nodules in selected patients. Besides, uniportal and non-intubated/ tubeless thoracoscopic segmentectomy are less invasive with prompt recovery, comparing with intubated general anesthesia, which contributes significantly to precision medicine (1-3). The chance of segmentectomy is minimal if a segment is too small, or it is located between neighboring segments (4). One of the major challenges of complete segmentectomy is the identification of the intersegmental plane. Transbronchial indocyanine green injection allows identification of the intersegmental lines and planes (5), which consists of ligation of the segmental vein and injection of indocyanine green through the segmental bronchus (6). Then both the surface and parenchyma of the lung are stained with easily recognized segmental borderlines.
However, the previously reported methods for the identification of intersegmental plane are not that easy to master, therefore, a reliable segmental labeling method is truly needed for young surgeons. Herein, we offer a hypothetical segmental labeling procedure for non-intubated segmentectomy to solicit feedback from colleagues.
Technique
Firstly, preoperative three-dimensional computed tomography (3D-CT) angiography/bronchography or a 3D printing model using rapid prototyping could be done to distinguish anomalous branches of pulmonary vessels and to simulate the surgery prior to the actual resection (7).
In addition, the peripheral small nodule in the target segment is located by CT-guided coil or patent blue vital dye labeling for confirmation of its complete resection, while the deeply located nodules could be labeled by the vital dye (8). However, the preoperative location of the lesions should be avoided if related side effects such as bleeding and pneumothorax are evaluated to be significant.
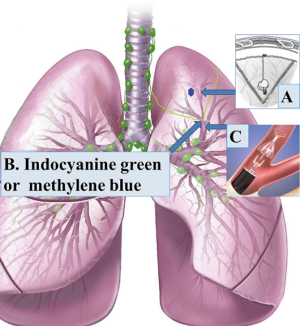
Next, the indocyanine green or methylene blue is sprayed into the bronchus of target segment as reported (6).
Subsequently, an one-way endobronchial valve is delivered by ultrathin bronchoscope to block the outlet of this bronchus for patients without interlobar collateral ventilation (9), which is aimed to achieve a complete atelectasis of the target segment, meanwhile, the remaining colored gas is extracted to avoid staining of the other lobes, and then the collapsed segment is confirmed under real-time CT monitoring (Figure 1).
As a result, a colored inflation-deflation line is created as the labeled segment is collapsed along the intersegmental plane, facilitating non-intubated segmentectomy assisted with artificial pneumothorax by carbon dioxide insufflation, using infrared thoracoscopy after indocyanine green injection or normal thoracoscopy after methylene blue staining, instead of conventionally repetitive inflation of the residual segments. The collapsed target segments are usually cone-shaped, therefore, the single surgical incision should be adjusted accordingly, which could be confirmed via simulation before surgery.
Lastly, the cutting edge is closed by fibrin glue and even composite mesh to diminish air leakage especially for emphysema patients. Intraoperative frozen-section sampling of the mediastinal lymph nodes is necessary, and lobectomy should be performed if possible when a lymph node is tumor-positive.
Discussion
This technique might deliver a colored and morphologically distinct line along the target segment, which is easy to be recognized for resection, and it is permitted by Ethic Committee of Xuzhou Central Hospital. However, there are several issues need to be elucidated before its clinical application.
The first issue is the establishment of strict selection criteria of lung cancer candidates suitable for segmentectomy, in addition to peripheral small-sized lung nodules and isolated metastatic tumors, because the data of long-term oncological outcomes is truly insufficient so far. It is noteworthy that, in most cases, segmentectomy is just a compromised choice for selected lung cancer patients with poor cardiopulmonary function.
The second issue is to distinguish patients with interlobar collateral ventilation, which could be measured and excluded by computed tomography-fissure analysis and the Chartis measurement as reported (10). The presenting method is seemingly not useful for patients with intersegmental collateral ventilation, because the target pulmonary segment could not be collapsed enough for resection after insertion of one-way endobronchial valve, especially for inexperienced clinicians.
Thirdly, the major dilemma in precise segmentectomy for young doctors is lacking of a definite intersegmental plane, which is essential to avoid or diminish the unnecessary resection of the adjacent normal tissues. Therefore, this presenting procedure, which is really expensive, is needless for experienced thoracic surgeons, meanwhile, initial data of this procedure could be available by experienced surgeons.
On the other hand, it is reported that contraindications of transbronchial injection of indocyanine green include allergy to indocyanine green or iodine, hyperthyroidism, thyroid neoplasm, and poor hepatic or renal function (11). Another LigaSure technique using intravenous indocyanine green fluorescence may be utilized to extend its indications (12).
Fourthly, the appropriate intrathoracic pressure needs to be controlled at a relatively low level after carbon dioxide insufflation, because the residual lung tissues should not be compressed excessively, so that an inflation-deflation line along the diseased segment remains for identification and resection.
Fifthly, the presented method with intrinsic drawbacks and limitations is merely a hypothesis, and it seems really costly, meanwhile, radiologist, pneumologist and surgeons are involved with tremendous personal and technical investment. Furthermore, a multi-functional operating room might need to be established for convenience, which is probably unrealistic. Therefore, in vivo experiment using animal models is necessary for experience before its validation, regarding feasibility and technical details of this method. Specifically, proper modifications such as time interval between each step might be settled via animal experiments, which is helpful to diminish both the evitable risks and misleading information for patients as well as young surgeons.
Last but not least, this procedure might not be considered without favorable results from the preliminary data. After all, it could be merely a reference for the evolution of other simple, practical methods for precise thoracic surgery.
Acknowledgements
Funding: This study is supported by Jiangsu Province Innovative and Entrepreneurial Talent Introduction Plan (Wenbin Wu, 2016), and Xuzhou City Science and Technology Project (No. KC16SH102).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Guo Z, Yin W, Pan H, et al. Video-assisted thoracoscopic surgery segmentectomy by non-intubated or intubated anesthesia: a comparative analysis of short-term outcome. J Thorac Dis 2016;8:359-68. [Crossref] [PubMed]
- Cui F, Liu J, Li S, et al. Tubeless video-assisted thoracoscopic surgery (VATS) under non-intubated, intravenous anesthesia with spontaneous ventilation and no placement of chest tube postoperatively. J Thorac Dis 2016;8:2226-32. [Crossref] [PubMed]
- Chow SC, Ng CS. Recent developments in video-assisted thoracoscopic surgery for pulmonary nodule management. J Thorac Dis 2016;8:S509-16. [Crossref] [PubMed]
- Ueda K, Tanaka T, Hayashi M, et al. What proportion of lung cancers can be operated by segmentectomy? A computed-tomography-based simulation. Eur J Cardiothorac Surg 2012;41:341-5. [Crossref] [PubMed]
- Sekine Y, Ko E, Oishi H, et al. A simple and effective technique for identification of intersegmental planes by infrared thoracoscopy after transbronchial injection of indocyanine green. J Thorac Cardiovasc Surg 2012;143:1330-5. [Crossref] [PubMed]
- Oh S, Suzuki K, Miyasaka Y, et al. New technique for lung segmentectomy using indocyanine green injection. Ann Thorac Surg 2013;95:2188-90. [Crossref] [PubMed]
- Oizumi H, Kanauchi N, Kato H, et al. Anatomic thoracoscopic pulmonary segmentectomy under 3-dimensional multidetector computed tomography simulation: a report of 52 consecutive cases. J Thorac Cardiovasc Surg 2011;141:678-82. [Crossref] [PubMed]
- Lin MW, Tseng YH, Lee YF, et al. Computed tomography-guided patent blue vital dye localization of pulmonary nodules in uniportal thoracoscopy. J Thorac Cardiovasc Surg 2016;152:535-44.e2. [Crossref] [PubMed]
- Klooster K, ten Hacken NH, Hartman JE, et al. Endobronchial Valves for Emphysema without Interlobar Collateral Ventilation. N Engl J Med 2015;373:2325-35. [Crossref] [PubMed]
- Koster TD, Slebos DJ. The fissure: interlobar collateral ventilation and implications for endoscopic therapy in emphysema. Int J Chron Obstruct Pulmon Dis 2016;11:765-73. [Crossref] [PubMed]
- Pardolesi A, Veronesi G, Solli P, et al. Use of indocyanine green to facilitate intersegmental plane identification during robotic anatomic segmentectomy. J Thorac Cardiovasc Surg 2014;148:737-8. [Crossref] [PubMed]
- Kuroda H, Dejima H, Mizumo T, et al. A new LigaSure technique for the formation of segmental plane by intravenous indocyanine green fluorescence during thoracoscopic anatomical segmentectomy. J Thorac Dis 2016;8:1210-6. [Crossref] [PubMed]