Magmaris: a new generation metallic sirolimus-eluting fully bioresorbable scaffold: present status and future perspectives
Introduction
Permanent metallic drug-eluting stents (DES) are the current gold standard in percutaneous myocardial revascularization, as they have clearly demonstrated to warrant easy deliverability, good scaffolding, low neointimal hyperplasia, low restenosis rate, and low incidence of major cardiac adverse events (MACE) at long term follow up (1,2).
Nevertheless, despite their good results, a few concerns regarding their use are still there, mainly about negative consequences of permanent caging of the vessel. Analyzing in detail, a few shortcomings can be noticed (3-5).
Reduction or turbulence of side-branch flow is frequent, hindrance of positive vascular remodeling and prevention of significant vasomotion restoration are inevitable.
Interference with future surgical revascularization can be an issue.
Hypersensitivity reactions to polymers are possible (though they can now be prevented by polymer-free DES).
A low rate of late or very late stent thrombosis (ST) and stent fracture is still detectable.
Impaired lesion imaging in magnetic resonance and computed tomography limit the quality of non-invasive assessments.
Bioresorbable scaffolds (BRS), developed to theoretically overcome most of such limitations, are the so-called 4th revolution in interventional cardiology and have the potential to significantly improve coronary artery disease treatment (6-11).
First generation BRS Absorb (Abbott Vascular, Santa Clara, CA, USA) and DESolve (Elixir Medical Corporation, Milpitas, CA, USA) backbones are poly-L-lactic acid (PLLA)-based and limus-eluting.
Randomized controlled trials (RCT) comparing a PLLA-BRS Absorb versus a cobalt chromium everolimus-eluting stent have shown slightly but non significantly worse outcomes of PLLA-BRS at 1 year, but progressively unfavorable outcomes have surfaced up to 3 years (12-24).
It is likely, and it must be remarked, that, according to experts’ current opinion, an inadequate implantation technique has been widely employed in many RCT affecting at least the early years’ outcome.
Device characteristics
Magmaris BRS, formerly known as DREAMS 2G, is the first bio-corrodible metallic BRS available on the market, having received CE approval in Europe in June 2016. It is a balloon-expandable, sirolimus-eluting, bioresorbable metallic scaffold, mounted on a rapid-exchange delivery system. It was developed to improve the previous paclitaxel-eluting DREAMS platform tested in BIOSOLVE-I trial.
The backbone is made of a proprietary absorbable Mg alloy, is completely radiolucent and has permanent tantalum radiopaque double markers at the distal and proximal end. The markers are shifted by 90° to improve radiological visibility from every point of view. They are silicon-covered to avoid interactions with the Mg alloy, because Mg has great chemical and galvanic sensitivity to direct proximity to different metals.
The backbone surface is fully coated with 7 µm of the same biodegradable PLLA polymer BIOlute used in the Orsiro stent (Biotronik AG, Bülach, Switzerland), and is similarly loaded with sirolimus, at a dose of 1.4 µg/mm2 of scaffold surface. The controlled drug release is calibrated for a 90-day completion.
This new generation BRS has an open cell design with 6 crown and 2 links in the axial direction. The square-shaped struts are 150 µm × 140 µm in thickness and width respectively, and are electro-polished. Nominal pressure is 10 atm while rated burst pressure is 16 atm, and the diameter can be safely expanded up to a maximum of 0.6 mm above the nominal diameter.
The system has a rapid exchange balloon-expandable delivery, adapted from the Orsiro platform, and has a crossing profile of 1.5 mm, which enables a 6 Fr compatibility.
Currently available scaffold sizes are 3.0 and 3.5 mm diameter and 15, 20 and 25 mm lengths; a 2.5 mm diameter scaffold used in trials is currently unavailable and it will be released on the market probably not before the beginning of 2018.
A bench test (25) compared Abbott Absorb GT1 and Elixir DESolve to Magmaris (6 vs. 3 vs. 6 scaffolds); this last showed improved trackability, with a 29% reduction in the peak force needed to track through a tortuous vessel (Absorb GT1 2.40±0.21 N vs. DESolve 1.76±0.24 N vs. Magmaris 1.70±0.21 N, P<0.001 for Magmaris vs. Absorb GT1). It also showed slightly improved pushability, with a 34% increase in the force transmitted from the hub to the tip (Absorb GT1 33.77%±1.22% vs. DESolve 36.27%±1.30% vs. Magmaris 45.41%±2.03%, P=NS).
Other interesting results from the bench came from recoil tests in a mock vessel. When compared to PLLA-based competitors, Magmaris showed lesser acute recoil (Absorb GT1 5.22%±0.38% vs. DESolve 9.42%±0.21% vs. Magmaris 4.94%±0.31%) and almost no 1-hour post-expansion recoil (Absorb GT1 7.82%±0.47% vs. DESolve 11.41%±0.08% vs. Magmaris 4.85%±0.41%).
Resorption process
Mg alloy resorption is a two-stage process starting at the backbone surface, and continuing inward until only an amorphous footprint of hydroxyapatite is left instead of the struts. Corrosion progresses equally from every side in vitro but not in vivo, where the lateral sides of the struts are preferentially and intensely attacked by cells, macrophages in particular, with their digestion enzymes. About 95% of the Mg is resorbed within 12 months.
In the first stage water and ions like calcium and phosphate of the surrounding tissues pass the BIOlute coating and reach the backbone, then the alloy reacts with water to create Mg hydroxide and corrosion begins. In the second stage, Mg hydroxide is slowly converted to an amorphous calcium phosphate phase, which has a high water content. Cracks infiltrated by cells appear in the core and material is getting reabsorbed.
Side effects of a minimum amount of degradation products are not expected since Mg has a key role in many biological systems. On the other hand, for instance, Mg antiarrhythmic properties are well known (26), and reduction in ischemia-reperfusion injury using Mg was experimentally documented (27). An Mg-mediated inhibition of the endotelin-1 production is also known, and prevents endothelin-induced vasoconstriction (28,29).
Due to its electronegative charge during degradation, potential antithrombotic properties of Mg have been reported in animal models (30-32). In vitro tests of Mg based BRS showed a decreased smooth muscle cell proliferation and an increased endothelial cell proliferation (33).
Dissimilarly, the BIOlute coating degradation process instead is longer than 24 months. PLLA is a semi-crystalline polymer (a mixture of amorphous and crystalline phase) that undergoes self-catalysed, inside-out, 3-step hydrolytic degeneration to lactic acid.
The first step is polymer hydration, which develops while water diffuses into the less dense amorphous regions and hydrolyzes ester bonds, thus causing random chain scissions and reduction of polymer molecular weight.
The second step is the scission of amorphous phase ties which connect the crystalline phase, leading to structural discontinuities and radial strength decrease.
During the third step hydrolyzed short polymer chains increase their hydrophilic and soluble properties, and diffuse out of the coating, leading to mass loss.
These small particles are phagocytosed by macrophages; at this stage lactic acid monomers loose a proton and become lactates. Lactates are subsequently converted into pyruvates and enter Kreb’s cycle, where they are metabolized to CO2 and H2O.
Magmaris clinical program and current status
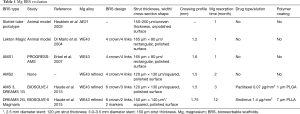
The first report of a biodegradable Mg alloy biocompatibility with vasculature came in 2003 from Heublein et al.’s pioneering work in an animal model using stents made of AE21 Mg alloy (containing 2% aluminium and 1% rare earths) showing negligible inflammatory response up to 56 days (30,34).
In 2004 Di Mario et al. (35) tested the Lekton Magic stent (Biotronik AG, Bülach, Switzerland), made of WE43, a different Mg alloy containing also <5% Zirconium, <5% Yttrium and <5% rare earths, demonstrating a positive remodelling, and a fast endothelialization process in an animal model.
The Lekton Magic was further improved and became the first version of the absorbable metallic stent (AMS1) (Biotronik, Berlin, Germany). It was substantially a slotted-tube stent made of WE43 Mg alloy. There was neither polymer coating nor drug elution. The thick backbone had a rectangular cross-section profile of the struts (80 µm × 165 µm width and thickness), and because of its radiolucency the positioning was guided by the two markers of the balloon.
From 2005 to 2007 AMS1 was tested in humans treating lower limb arteries in adults (36-38) as well as aorta and pulmonary arteries in pediatric patients (39-41).
AMS1 clinical safety and efficacy assessment started in 2007 with the first-in-man (FIM) prospective, non-randomized multicenter PROGRESS-AMS clinical trial (Clinical Performance and Angiographic Results of Coronary Stenting with Absorbable Metal Stents; ClinicalTrials.gov Identifier: NCT01610102) (42). Sixty-three patients with simple lesions (single stenosis, lesion length ≤15 mm) received 71 AMS1 (10 to 15 mm in length, 3.0 to 3.5 mm in diameter). Small vessels were excluded [reference vessel diameters (RVD) range, 3.0–3.5 mm]. Pre-dilatation was mandatory while post-dilatation was at discretion and was performed in 66.7% of cases.
The patients received a post-procedural intravascular ultrasound (IVUS) evaluation, an angiographic and IVUS follow up at 4 months plus a planned clinical assessment at 6 and 12 months. Nine patients underwent a later IVUS follow-up as well (range, 12–28 months).
Primary endpoints of the study were cardiac death (CD), non-fatal MI and target lesion revascularization (TLR) at 4 months.
Results at 4 months showed vasoreactivity at acetylcholine (ACH) test (43) and no CD, MI or scaffold thrombosis (ScT) where observed, but a high rate of MACE (23.8%), TLR (39,7%), and angiographic in-stent late lumen loss (LLL) (1.08±0.49 mm) were seen. One-year TLR (45%) and MACE (26.7%) were unacceptably high.
The main IVUS findings (44) were an almost complete resorption of the struts at 4 months, and a significant vessel recoil caused by early radial strength loss. Intra- and extra-scaffold neointima proliferation was evident, due mainly to the absence of antiproliferative drug elution.
In order to overcome the radial strength issue the AMS2 was developed, with two different main features. In fact a square-shaped cross section profile of the struts and a refined WE43 Mg alloy were made. The absorption was delayed at 9–12 months, and a higher collapse pressure (1.5 bar AMS2 vs. 0.8 bar AMS1) was achieved. Furthermore, during anisotropic scaffold degradation (corrosion being preferential at lateral sides of the struts) the adopted square-shaped struts increased scaffold integrity, thereby allowing a reduced strut thickness of 130 µm × 120 µm.
The further evolution, called AMS3, was aimed to address the neointimal hyperplasia issue. Previous AMS2 was used as stent platform, but it was coated with a 1 µm paclitaxel-eluting, bioresorbable polymer matrix made of poly lactic-co-glycolic acid (PLGA).
As paclitaxel release rate depends on PLGA degradation, which in turn depends on its lactide-co-glycolide ratio, Wittchow et al. (45) tested AMS3 scaffolds with different PLGA formulations and different paclitaxel loading in pigs. The 85:15 H (high molecular weight) version with 8 µg paclitaxel showed the best results and this final iteration of the AMS3 scaffold was renamed DRug-Eluting AMS 1.0 DRug-Eluting Absorbable Metal Scaffold (DREAMS) (Biotronik AG, Bülach, Switzerland). Its safety and efficacy were tested in the FIM prospective, non-randomized multicenter BIOSOLVE-I clinical trial (Safety and Performance of the DREAMS, in Patients with de-novo Coronary Lesions; ClinicalTrials.gov Identifier: NCT01168830) (46-48).
Forty-seven first-generation DREAMS (1G) were implanted in 46 patients with 47 single de novo lesions. Silent ischemia, stable or unstable angina were the indication to percutaneous coronary intervention (PCI). A 3-year clinical follow-up and an angiographic and IVUS follow-up at 6 and 12 months were planned. Pre-dilatation was mandatory, post-dilatation was at discretion and was performed only in 14.9% of cases. Double anti-platelet therapy (DAPT) was recommended for at least 12 months.
Primary endpoint was target lesion failure (TLF), a composite of CD, target vessel myocardial infarction (TV-MI) and ischemia-driven (ID) TLR, at 6- and 12-month follow-up. At 6 months a 4% TLF (2/46 patients) was observed, with a subsequent increase at 6.6% (3/43 patients) at 12 months. At 3 years follow-up TLF remains unchanged, while a 4.3% ID-TLR (2/43 patients) and 2.2% TV-MI (1/43 patients) were reported. The single MI occurred during the scheduled 12-month angiographic follow-up as a complication of a PCI of the target vessel but not of the target segment. No CD or ScT was observed.
Quantitative coronary angiography (QCA) assessment showed 0.51±0.46 mm in-scaffold LLL and 0.28±0.34 mm in-segment LLL at 12 months, respectively decreased at 0.32±0.32 and 0.11±0.18 mm at 3 years. These data represented a drastic 61% reduction in comparison to 4-month PROGRESS-AMS data. Anyway, the new, higher level of performance wasn’t still good enough to compare well with traditional DES.
A further scaffold evolution was the second-generation DREAMS (DREAMS 2G), whose modified DREAMS 1G backbone became a 6-crown 2-link design with strut thickness of 150 µm × 140 µm. The coating shifted from 1 µm PLGA to 7 µm PLLA, this time sirolimus-eluting at a dose of 1.4 µg/mm2 (the same as for the Orsiro stent). Tantalum markers were added at the edges to provide the scaffold with some radiological visibility.
A brief synthesis of the various Mg BRS iterations is depicted in Table 1.
Full table
DREAMS 2G was tested in the FIM prospective, multi-centric, non-randomized BIOSOLVE-II study (Safety and Performance of the Second-generation Drug-Eluting Absorbable Metal Scaffold in Patients with de novo Coronary Artery Lesions; ClinicalTrials.gov Identifier: NCT01960504) (49).
A total of 123 patients (123 single de novo lesions) were enrolled and 121 patients with stable or unstable angina or silent ischemia were treated with 125 DREAMS 2G (4 patients received 2 BRS).
The target lesions were longer than in the two previous studies (length ≤21 mm) while the vessel were smaller in diameter (RVD range, 2.2–3.7 mm). Device sizes were 2.5×20, 3.0×20 and 3.5×25 mm2. Pre-dilatation was mandatory, post-dilatation was at operator’s discretion. DAPT was recommended for at least 6 months.
Angiographic follow-up was scheduled at 6 months for all patients while 42 patients agreed to an additional angiographic follow-up at 12 months. A subgroup of 30 patients underwent IVUS and optical coherence tomography (OCT) evaluation as well. A total of 25 patients had a vasomotion test at 6 months, 11 patients IVUS plus OCT and 14 patients had vasomotion tests repeated at 12 months.
Primary endpoint was in-segment LLL at 6 months. Secondary endpoints were set at 12 months: TLF [a composite of CD, TV-MI, coronary artery bypass grafting (CABG) and ID-TLR], ScT, in-scaffold and in-segment binary restenosis, diameter stenosis and in-scaffold LLL.
The 6-month follow-up obtained in 120 patients showed in-scaffold LLL of 0.44±0.36 mm and in-segment LLL of 0.27±0.37 mm. In-scaffold and in-segment binary restenosis were both 5% (6/120). A 3.3% TLF (4/120) was reported: 1 death for unknown causes classified as CD and possible ScT (0.8%), 1 TV-MI (0.8%) due to peri-procedural temporary no-reflow, and 2 ID-TLR (1.7%) for restenosis. No definite or probable ScT was recorded. One patient died because of cancer.
In the IVUS arm 30 patients showed a preservation of the scaffold area and a mean neointimal hyperplasia area of only 0.08 mm2. Moreover, malapposition area was 0.02 mm2 and incomplete strut apposition was 37% (11/30), but at OCT evaluation no malapposed or uncovered struts was detected.
Vasomotricity test with intracoronary ACH and nitrates (NTG) injection showed a certain amount of vasomotion recovery at 6 months (threshold of ≥3.0% change in mean lumen diameter) in 20 out of 25 patients (80%).
At 1-year follow-up (50) paired data obtained for 42 patients showed a 6 and 12-month in-segment LLL of 0.20±0.21 and 0.25±0.22 mm, and a 6 and 12-month in-scaffold LLL of 0.37±0.25 and 0.39±0.27 mm respectively. There were no statistically significant differences between paired data and between this subgroup and the overall patients population baseline characteristics. TLF at 1-year was 3.4% (4/118). No further events, notably ScT, occurred beyond 6-month follow-up.
Paired data of the 11 patients in imaging group showed no differences in 6- and 12-month IVUS parameters, except for zeroing the number of patients with incomplete strut apposition, but 6- and 12-month OCT data showed a disturbing significant decrease in mean minimal lumen area from 4.58 to 4.19 mm2 (P=0.032).
Serial vasomotion assessment on 14 patients showed a detectable response in 79% (11/14); the percentage change in 6- and 12-month mean lumen diameter between post-ACH and NTG was 3.4% and 6.7% respectively.
In early 2017 Waksman et al. (51) published a preclinical study where 90 (3.0 mm × 20 mm) Magmaris were implanted in porcine and rabbit models. Control devices were 3.0 mm × 18 mm Absorb GT1 BRS for sub-acute safety and endothelialization studies, and 3.0 mm × 18 mm Xience Xpedition for long term safety assessment.
Sub-acute safety study in pigs at 3 days showed a higher degree of endothelialization in Magmaris struts (overall endothelialization: Magmaris 47.0%±4.1% vs. Absorb GT1 31.4%±9.2%, P=0.0093) and fewer non-occlusive thrombi on struts in comparison to Absorb. Neither showed occlusive thrombi.
Endothelialization evaluation at 28 days in rabbit iliac arteries was in favor of Magmaris again (overall endothelialization: Magmaris 73.8%±10.5% vs. Absorb GT1 59.2%±8.0%, P=0.0073), this time both competitors displaying no significant thrombus deposition on struts.
In long-term follow-up QCA unveiled initial greater LLL for Magmaris compared to Xience, which became almost equal at 1 year. The results turned in Magmaris greater late lumen gain after 2 years, due to positive remodelling after BRS resorption (LLL at 90 days: Magmaris 0.49±0.20 mm vs. Xience 0.30±0.13 mm, P=0.02; at 1 year: Magmaris 0.10±0.16 mm vs. Xience 0.05±0.15 mm, P=0.67; at 2 years: Magmaris −0.32±0.19 mm vs. Xience −0.18±0.14 mm, P=0.12).
Histopathological investigation at early follow-up and at 2 years showed greater neointimal area for Magmaris compared to Xience (median neointimal area at 2 years: Magmaris 2.25 mm2vs. Xience 1.45 mm2, P=0.0009). Inflammatory response was initially worse in Magmaris with peak at 90 days and progressive decrease up to 2 years. On the contrary Xience showed minimal inflammation up to 90 days and subsequent increased, reaching a peak at 1 year (Inflammation score at 90 days: Magmaris 1.67 vs. Xience 0.0, P=0.04; at 1 year: Magmaris 1.67 vs. Xience 1.83, P=0.71; at 2 years: Magmaris 1.00 vs. Xience 1.67, P=0.04). Fibrin deposition was moderate for both stents at 28 days and very low thereafter.
OCT evaluation of mean lumen area at 2 years showed a significantly lesser decrease in Magmaris compared to Xience (baseline: Magmaris 7.76±0.60 mm2vs. Xience 8.87±0.35 mm2; at 2 years: Magmaris 7.14±0.48 mm2vs. Xience 7.16±0.42 mm2, P=0.03).
On the whole these results underscored Magmaris’ low acute thrombogenicity, advanced healing properties, good vascular compatibility and absence of excessive LLL up to 2 years, supporting its safety in human use.
A synopsis of Mg BRS clinical trials main results is displayed in Tables S1-S3.

Full table

Full table

Full table
As for next expected results, there are four currently ongoing studies.
The first one, sponsored by Biotronik, is BIOSOLVE-III Study [Acute Performance Of a Drug Eluting Absorbable Metal Scaffold (DREAMS 2G) in Patients With de Novo Lesions in NatiVE Coronary Arteries; ClinicalTrials.gov Identifier: NCT02716220] (52). It is a pre-market, prospective, multi-centric, pivotal trial, aimed to assess the acute clinical performance of the DREAMS 2G in de novo coronary artery simple lesions Inclusion criteria are maximum of two single stenoses in two different vessels, mean lesion length <21 mm, RVD between 2.7–3.8 mm, target lesion stenosis >50% and <100%. It has an estimate enrollment of 61 subjects with stable or unstable angina pectoris or documented silent ischemia in 8 centers in Belgium, Germany, the Netherlands and Switzerland.
The primary endpoint is procedural success, defined as achievement of a final diameter stenosis of <30% without occurrence of death, Q-wave or non-Q-wave MI, or TLR during a hospital stay of max 7 days. Secondary endpoints are TLF (a composite of CD, TV-MI, CABG, ID-TLR) and ScT rate up to 36 months post procedure, plus binary restenosis rate (%) in-scaffold and in-segment diameter stenosis, in-segment and in-scaffold LLL at 12-months.
Final data collection for primary outcome measure is expected in April 2017.
The second one is BIOSOLVE-IV (Safety and Performance in de NOvo Lesion of NatiVE Coronary Arteries With Magmaris-Registry; ClinicalTrials.gov Identifier: NCT02817802) (53), It is a post-market surveillance, prospective, single-arm, multi-centric registry aimed to test the clinical performance and long-term safety of Magmaris in patients with symptomatic coronary artery disease and single de novo native coronary artery lesions. This study targets a real-world population with few exclusion criteria (pregnancy, allergy and dialysis) and includes also complex lesions with the exception of occlusions. Inclusion criteria are target lesion stenosis >50% and <100% and TIMI flow ≥1. It is currently enrolling patients in two centers in Germany and Latvia, with a later estimate enrollment of 1,065 patients in Asia, Australia and Europe. Primary endpoint is TLF at 12 months. Final data collection for primary outcome measure is expected by October 2018.
The third one is BIOSOLVE-India (Safety and Clinical Performance Of the Magmaris Drug Eluting Absorbable Metal Scaffold in a Cohort of Patients in India With de Novo Lesions in NatiVE Coronary Arteries; ClinicalTrials.gov Identifier: NCT02916485) (54). It is a prospective, multi-centric, single-arm, open-label trial assessing the safety and clinical performance of Magmaris in de novo simple lesions. Inclusion criteria are: maximum of two single stenoses in two different vessels, mean lesion length ≤21 mm, RVD between 2.7–3.8 mm, target lesion stenosis >50% and <100% and TIMI flow ≥1). A total of 110 patients with de novo lesions in native coronary arteries will be enrolled at 8 investigational sites in India. In-hospital clinical follow-up is planned at 1 and 6 months post procedure.
Primary endpoint is TLF (a composite of CD, TV-MI, CABG, clinically driven TLR) at 1 month. Secondary endpoints are: TLF at 6 months post-procedure, target vessel failure (TVF), TLR, CD, MI, ScT at 1 and 6 months post-procedure, procedure success (defined as achievement of a final diameter stenosis of <30% without the occurrence of death, Q-wave or non-Q-wave MI, or TLR during the hospital stay of 3±2 days), device success (a composite of final diameter stenosis of <30%, successful delivery of the scaffold to the target lesion site in the coronary artery, appropriate scaffold deployment, successful removal of the device, safe removal of the device in case of deployment failure). Final data collection for primary outcome assessment is expected by June 2017.
The last one is the Magnesium 1,000 Program (55), recording worldwide the acute performances of the first 1,000 Magmaris BRS implantation outside the trials. The registry has reached 1,000 implants performed in 25 countries to date, and results are expected soon.
Patient and lesion selection
A panel of the experts involved in the FIM studies with AMS-DREAMS scaffolds produced a consensus document just before Magmaris European market launch in June 2016 (56).
It recognized that this technology was—and still is—in its infancy, and kept in mind the experience gained with Absorb, whose unrestricted use at launch allowed some implantation pitfalls, which in turn probably led, for instance, to a higher than expected ScT rate.
The panel stated that, at least initially, Magmaris implantation should be limited to patients with long life expectancy, and with stable, short de novo lesions which have good likelihood to regain vasomotion.
So, according to the experts’ opinion, Magmaris implantation must be avoided if returning vasomotion cannot be expected (e.g., saphenous grafts, in-stent restenoses, previous stents in the same vessel, heavy calcification), if the sizing is uncertain, if there is remaining thrombus at the lesion site, and if adequate pre-dilatation cannot be obtained (please see below, Implantation technique).
Furthermore, for the time being Magmaris must be avoided in left main lesions, in ostial lesions, and in lesions with complex anatomy (heavy calcification; challenging tortuosity or angulation; diffuse, long disease).
ST-elevation myocardial infarction (STEMI) patients must not be implanted due to lack of data and to concern about further platelets activation from thick struts.
Finally, patients who cannot comply with current ESC/EAPCI DAPT recommendations for stable lesions must not be implanted.
A summary of indications and contraindications is displayed in Table 2.

Full table
Implantation technique
Imaging-guided implantation is highly recommended, in order to asses precisely the vessel size, to detect possible calcification to the best (keeping in mind that significant calcification is currently still an unfavorable subset for any BRS, and to decide whether post-dilatation is required.
The Magmaris IFU recommend a vessel diameter between 2.7 and 3.2 mm for a scaffold diameter of 3.0 mm and a vessel diameter between 3.2 and 3.7 mm for a scaffold diameter of 3.5 mm.
A careful vessel preparation is necessary, so an effective pre-dilatation is mandatory. If a complete expansion of the pre-dilatation balloon or if a <30% post pre-dilatation residual stenosis are not achieved, a Magmaris must not be implanted.
The inflation is single-step, completely DES-like.
According to experts’ opinion, decision to perform or not post-dilatation should be imaging-guided. If imaging is not available post-dilatation is mandatory, with the goal of best strut apposition and <20% final residual stenosis. Anyway, borrowing the experience recently gained with PLLA-BRS, maybe post-dilatation could be the standard for the time being. Post-dilatation must be done with a non-compliant balloon inflated to a pressure greater than 16 atmospheres and of the same nominal size as the scaffold or up to 0.5 mm larger. If needed, upsizing of the device should be limited to 0.6 mm beyond the nominal size.
A planned overlap should be avoided. Just in case, a second Magmaris can be implanted and juxtaposed scaffold-to-scaffold avoiding gap and supraposition. If a DES is preferred for the overlap, a second generation DES is better employed. However, in the absence of significant data, the manufacturer and a consensus document from an expert panel (56) suggest the use of an Orsiro stent due to its ProBIO passive coating which, they state, does not interfere with the contiguous Mg alloy.
The anticoagulation regimen during the procedure and the DAPT are the same than for PCI with DES. A minimum of 6 months is required for stable patients.
Magmaris’ current and future perspectives
The current Magmaris instrumental and clinical data are good. However these data are still sparse, based on a small number of non-RCT studies and on a small number of patients.
The overall follow-up is still short.
It must be also absolutely kept in mind that to date the only reliable study available for Magmaris validation is BIOSOLVE II, where only 123 patients were treated and any kind of complex lesion was excluded. Previous studies, however important for the development, tested different iterations of the device and provide little information about the current one.
In comparison to the leading PLLA BRS, Magmaris shows better radial force, pushability and trackability, this last partly due to the technical possibility of polishing the strut edges.
Precise positioning is made easier by the possibility of a rapid, single-step inflation, which also contributes to limit the procedural ischemia time.
Conversely, fine tuning of the BRS (expecially post-dilatation and overlap) are rather difficult due to absolute lack of radiological visibility of the scaffold itself, which is little compensated by scarce visibility of the markers as well.
A few imaging and histopathological data seem to demonstrate good struts embedment and rapid endothelialization, which could correlate with the finding of a zero definite/probable ScT rate to date, but a confirmation by dedicated and systematic imaging studies is needed.
A fast reabsorption allows a short vascular irritation time, which might be useful for limiting ScT and irritation-related restenosis. On the contrary, the same fast reabsorption—with consequent very fast loss of radial strength and scaffolding—might oppose too feebly to late recoil, which seems possibly related to some kind of well-known stent and scaffold restenosis and thrombosis. Anyway, the best duration of reabsorption balance has not been clearly established yet.
Similarly, no data are available about possible consequences of spasm. Actually it might affect—about rheology and apposition—a degradating BRS which is still physically present, but lacks very early any residual radial strength.
Little clinical data are available about vasomotion recovery.
The biocompatibility properties are very good, and are testified by Mg-alloy devices already employed in non-cardiac fields.
The evaluation of real future perspectives requires first a clear evidence of good long-term outcomes in less simple, more clinically common lesions, to be obtained in RCT with adequate statistical power to analyze hard clinical endpoints and relatively rare events such as ST. Should this happen, a rapid reabsorption time coupled to a good albeit temporary scaffolding will prove an advantage.
Furthermore, speaking of hypothetical future perspectives, as Mg alloys features are known to be quite easily modified, it is possible that different varieties of the alloy can coexist and be adapted, in terms of radial strength and reabsorption, to the requirements of different kind of lesions.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014;35:2541-619. [Crossref] [PubMed]
- Iqbal J, Serruys PW, Silber S, et al. Comparison of zotarolimus- and everolimus-eluting coronary stents: final 5-year report of the RESOLUTE all-comers trial. Circ Cardiovasc Interv 2015;8:e002230. [Crossref] [PubMed]
- Finn AV, Joner M, Nakazawa G, et al. Pathological correlates of late drug-eluting stent thrombosis: strut coverage as a marker of endothelialization. Circulation 2007;115:2435-41. [Crossref] [PubMed]
- Cook S, Ladich E, Nakazawa G, et al. Correlation of intravascular ultrasound findings with histopathological analysis of thrombus aspirates in patients with very late drug-eluting stent thrombosis. Circulation 2009;120:391-9. [Crossref] [PubMed]
- Joner M, Finn AV, Farb A, et al. Pathology of drug-eluting stents in humans: delayed healing and late thrombotic risk. J Am Coll Cardiol 2006;48:193-202. [Crossref] [PubMed]
- Iqbal J, Onuma Y, Ormiston J, et al. Bioresorbable scaffolds: rationale, current status, challenges, and future. Eur Heart J 2014;35:765-76. [Crossref] [PubMed]
- Wiebe J, Nef HM, Hamm CW. Current status of bioresorbable scaffolds in the treatment of coronary artery disease. J Am Coll Cardiol 2014;64:2541-51. [Crossref] [PubMed]
- Garg S, Serruys P. Biodegradable and non-biodegradable stents. Minerva Cardioangiol 2009;57:537-65. [PubMed]
- Onuma Y, Serruys PW. Bioresorbable scaffold: the advent of a new era in percutaneous coronary and peripheral revascularization? Circulation 2011;123:779-97. [Crossref] [PubMed]
- Ormiston JA, Webster MWI, Armstrong G. First-in-human implantation of a fully bioabsorbable drug-eluting stent: The BVS poly-L-lactic acid everolimus-eluting coronary stent. Catheter Cardiovasc Interv 2007;69:128-31. [Crossref] [PubMed]
- Serruys PW, Garcia-Garcia HM, Onuma Y. From metallic cages to transient bioresorbable scaffolds: change in paradigm of coronary revascularization in the upcoming decade? Eur Heart J 2012;33:16-25b. [Crossref] [PubMed]
- Serruys PW, Chevalier B, Dudek D, et al. A bioresorbable everolimus-eluting scaffold versus a metallic everolimus-eluting stent for ischaemic heart disease caused by de-novo native coronary artery lesions (ABSORB II): an interim 1-year analysis of clinical and procedural secondary outcomes from a randomised controlled trial. Lancet 2015;385:43-54. [Crossref] [PubMed]
- Capodanno D, Gori T, Nef H, et al. Percutaneous coronary intervention with everolimus-eluting bioresorbable vascular scaffolds in routine clinical practice: early and midterm outcomes from the European multicentre GHOST-EU registry. EuroIntervention 2015;10:1144-53. [Crossref] [PubMed]
- Ishibashi Y, Onuma Y, Muramatsu T, et al. ABSORB EXTEND Investigators. Lesson learned from acute and late scaffold failures in the ABSORB EXTEND trial. EuroIntervention 2014;10:449-57. [Crossref] [PubMed]
- Serruys PW, Ormiston JA, Onuma Y, et al. A bioabsorbable everolimus-eluting coronary stent system (ABSORB): 2-year outcomes and results from multiple imaging methods. Lancet 2009;373:897-910. [Crossref] [PubMed]
- Puricel S, Arroyo D, Corpataux N, et al. Comparison of everolimus- and biolimus-eluting coronary stents with everolimus-eluting bioresorbable vascular scaffolds. J Am Coll Cardiol 2015;65:791-801. [Crossref] [PubMed]
- Ellis SG, Kereiakes DJ, Metzger DC, et al. Absorb III Investigators. Everolimus-eluting bioresorbable scaffolds for coronary artery disease. N Engl J Med 2015;373:1905-15. [Crossref] [PubMed]
- Stone GW, Gao R, Kimura T, et al. 1-year outcomes with the Absorb bioresorbable scaffold in patients with coronary artery disease: a patient-level, pooled meta-analysis. Lancet 2016;387:1277-89. [Crossref] [PubMed]
- Cassese S, Byrne RA, Ndrepepa G, et al. Everolimus-eluting bioresorbable vascular scaffolds versus everolimus-eluting metallic stents: a meta-analysis of randomised controlled trials. Lancet 2016;387:537-44. [Crossref] [PubMed]
- Serruys PW, Chevalier B, Sotomi Y, et al. Comparison of an everolimus-eluting bioresorbable scaffold with an everolimus-eluting metallic stent for the treatment of coronary artery stenosis (ABSORB II): a 3 year, randomised, controlled, single-blind, multicentre clinical trial. Lancet 2016;388:2479-91. [Crossref] [PubMed]
- Lipinski MJ, Escarcega RO, Baker NC, et al. Scaffold thrombosis after percutaneous coronary intervention with ABSORB bioresorbable vascular scaffold: a systematic review and meta-analysis. JACC Cardiovasc Interv 2016;9:12-24. [Crossref] [PubMed]
- Puricel S, Cuculi F, Weissner M, et al. Bioresorbable Coronary Scaffold Thrombosis: Multicenter Comprehensive Analysis of Clinical Presentation, Mechanisms, and Predictors. J Am Coll Cardiol 2016;67:921-31. [Crossref] [PubMed]
- Räber L, Brugaletta S, Yamaji K, et al. Very Late Scaffold Thrombosis: Intracoronary Imaging and Histopathological and Spectroscopic Findings. J Am Coll Cardiol 2015;66:1901-14. [Crossref] [PubMed]
- Sotomi Y, Suwannasom P, Serruys PW, et al. Possible mechanical causes of scaffold thrombosis: insights from case reports with intracoronary imaging. EuroIntervention 2017;12:1747-56. [Crossref] [PubMed]
- Schmidt W, Behrens P, Brandt-Wunderlich C, et al. In vitro performance investigation of bioresorbable scaffolds - Standard tests for vascular stents and beyond. Cardiovasc Revasc Med 2016;17:375-83. [Crossref] [PubMed]
- Smith LF, Heagerty AM, Bing RF, et al. Intravenous infusion of magnesium sulphate after acute myocardial infarction: Effects on arrhytmias and mortality. Int J Cardiol 1986;12:175-83. [Crossref] [PubMed]
- Christensen CW, Rieder MA, Silverstein EL, et al. Magnesium sulfate reduces myocardial infarct size when administered before but not after coronary reperfusion in a canine model. Circulation 1995;92:2617-21. [Crossref] [PubMed]
- Kemp PA, Gardiner SM, March JE, et al. Assessment of the effects of endothelin-1 and magnesium sulphate on regional blood flows in conscious rats, by the coloured microsphere reference technique. Br J Pharmacol 1999;126:621-6. [Crossref] [PubMed]
- Berthon N, Laurant P, Fellmann D, et al. Effect of magnesium on mRNA expression and production of endothelin-1 in DOCA-salt hypertensive rats. J Cardiovasc Pharmacol 2003;42:24-31. [Crossref] [PubMed]
- Heublein B, Rohde R, Kaese V, et al. Biocorrosion of magnesium alloys: a new principle in cardiovascular implant technology? Heart 2003;89:651-6. [Crossref] [PubMed]
- Rukshin V, Azarbal B, Shah PK, et al. Intravenous magnesium in experimental stent thrombosis in swine. Arterioscler Thromb Vasc Biol 2001;21:1544-9. [Crossref] [PubMed]
- Rukshin V, Shah PK, Cercek B. Comparative antithrombotic effects of magnesium sulfate and the platelet glycoprotein IIb/IIIa inhibitors tirofiban and eptifibatide in a canine model of stent thrombosis. Circulation 2002;105:1970-5. [Crossref] [PubMed]
- Sternberg K, Gratz M, Koeck K, et al. Magnesium used in bioabsorbable stents controls smooth muscle cell proliferation and stimulates endothelial cells in vitro. J Biomed Mater Res B Appl Biomater 2012;100:41-50. [Crossref] [PubMed]
- Heublein B, Rohde R, Niemeye M, et al. Degradation of metallic alloys - A new principle in stent technology? J Am Coll Cardiol 2000;35:14A-5A.
- Di Mario C, Griffiths H, Goktekin O, et al. Drug-eluting bioabsorbable magnesium stent. J Interv Cardiol 2004;17:391-5. [Crossref] [PubMed]
- Peeters P, Bosiers M, Verbist J, et al. Preliminary results after application of absorbable metal stents in patients with critical limb ischemia. J Endovasc Ther 2005;12:1-5. [Crossref] [PubMed]
- Bosiers M, Deloose K, Verbist J, et al. First clinical application of absorbable metal stents in the treatment of critical limb ischemia: 12-month results. Vascular Disease Management 2005;2:86-91.
- Bosiers M, Peeters P, D'Archambeau O, et al. AMS INSIGHT--absorbable metal stent implantation for treatment of below-the-knee critical limb ischemia: 6-month analysis. Cardiovasc Intervent Radiol 2009;32:424-35. [Crossref] [PubMed]
- Zartner P, Cesnjevar R, Singer H, et al. First successful implantation of a biodegradable metal stent into the left pulmonary artery of a preterm baby. Catheter Cardiovasc Interv 2005;66:590-4. [Crossref] [PubMed]
- Schranz D, Zartner P, Michel-Behnke I, et al. Bioabsorbable metal stents for percutaneous treatment of critical recoarctation of the aorta in a newborn. Catheter Cardiovasc Interv 2006;67:671-3. [Crossref] [PubMed]
- McMahon CJ, Oslizlok P, Walsh KP. Early restenosis following biodegradable stent implantation in an aortopulmonary collateral of a patient with pulmonary atresia and hypoplastic pulmonary arteries. Catheter Cardiovasc Interv 2007;69:735-8. [Crossref] [PubMed]
- Erbel R, Di Mario C, Bartunek J, et al. PROGRESS-AMS (Clinical Performance and Angiographic Results of Coronary Stenting with Absorbable Metal Stents) investigators. Temporary scaffolding of coronary arteries with bioabsorbable magnesium stents: A prospective, non-randomised multicentre trial. Lancet 2007;369:1869-75. [Crossref] [PubMed]
- Ghimire G, Spiro J, Kharbanda R, et al. Initial evidence for the return of coronary vasoreactivity following the absorption of bioabsorbable magnesium alloy coronary stents. EuroIntervention 2009;4:481-4. [Crossref] [PubMed]
- Waksman R, Erbel R, Di Mario C, et al. Early and long-term intravascular ultrasound and angiographic findings after bioabsorbable magnesium stent implantation in human coronary arteries. JACC Cardiovasc Interv 2009;2:312-20. [Crossref] [PubMed]
- Wittchow E, Adden N, Riedmüller J, et al. Bioresorbable drug-eluting magnesium-alloy scaffold: design and feasibility in a porcine coronary model. EuroIntervention 2013;8:1441-50. [Crossref] [PubMed]
- Haude M, Erbel R, Erne P, et al. Safety and performance of the drug-eluting absorbable metal scaffold (DREAMS) in patients with de-novo coronary lesions: 12 month results of the prospective, multicentre, first-in-man BIOSOLVE-I trial. Lancet 2013;381:836-44. [Crossref] [PubMed]
- Haude M, Erbel R, Erne P, et al. Safety and performance of the DRug-Eluting Absorbable Metal Scaffold (DREAMS) in patients with de novo coronary lesions: 3-year results of the prospective, multicentre, first-in-man BIOSOLVE-I trial. EuroIntervention 2016;12:e160-6. [Crossref] [PubMed]
- Waksman R, Prati F, Bruining N, et al. Serial observation of drug-eluting absorbable metal scaffold: multi-imaging modality assessment. Circ Cardiovasc Interv 2013;6:644-53. [Crossref] [PubMed]
- Haude M, Ince H, Abizaid A, et al. Safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de-novo coronary artery lesions (BIOSOLVE-II): 6 month results of a prospective, multicentre, non-randomised, first-in-man trial. Lancet 2016;387:31-9. [Crossref] [PubMed]
- Haude M, Ince H, Abizaid A, et al. Sustained safety and performance of the second-generation drug-eluting absorbable metal scaffold in patients with de novo coronary lesions: 12-month clinical results and angiographic findings of the BIOSOLVE-II first-in-man trial. Eur Heart J 2016;37:2701-9. [Crossref] [PubMed]
- Waksman R, Zumstein P, Pritsch M, et al. Second-generation Magnesium Scaffold Magmaris, Device Design, and Preclinical Evaluation in a Porcine Coronary Artery Model. EuroIntervention 2017;13:440-449. [Crossref] [PubMed]
- Acute Performance Of a Drug Eluting Absorbable Metal Scaffold (DREAMS 2G) in Patients With de Novo Lesions in NatiVE Coronary Arteries: BIOSOLVE-III. Accessed March 21, 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT02716220
- Safety and Performance in de NOvo Lesion of NatiVE Coronary Arteries With Magmaris Registry: BIOSOLVE-IV. Accessed March 21, 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT02817802
- Safety and Clinical Performance Of the Magmaris Drug Eluting Absorbable Metal Scaffold in a Cohort of Patients in India With de Novo Lesions in NatiVE Coronary Arteries. BIOSOLVE-India. Accessed March 21, 2017. Available online: https://clinicaltrials.gov/ct2/show/NCT02916485
- Waksman R. Magmaris a Magnesium Based Bioresorbable Scaffold. Presented at Joint Interventional Meeting; February 8, 2017. Milan, Italy.
- Fajadet J, Haude M, Joner M, et al. Magmaris preliminary recommendation upon commercial launch: a consensus from the expert panel on 14 April 2016. EuroIntervention 2016;12:828-33. [Crossref] [PubMed]


