Difficult intubation due to unknown congenital tracheal stenosis in the adult: a case report and literature review
Introduction
Congenital tracheal stenosis (CTS) is a rare disorder. It is almost always diagnosed in infancy due to respiratory distress (1). Often complicated with other cardiopulmonary abnormalities, most patients require immediate surgical intervention (2). It is extremely rare that patients survive undiagnosed. We experienced an adult case of CTS who remained undiagnosed until routine intubation procedures for surgery was unsuccessful. Difficult airway management is a potentially lethal airway emergency. This life-threatening situation is preventable with the appropriate awareness. We report this clinically valuable case for the safety of future patient care. The patient gave informed consent for publication.
Case presentation
A 42-year-old female presented with dyspnea from four days before. Chest X-ray showed right-sided pneumothorax. She had three right-sided pneumothoraces in the past year, all found asymptomatically on regular check-ups and all improving with rest. Past medical history included bronchial asthma (diagnosed from history and symptoms without spirometry) and atopic dermatitis. She had no smoking history. Family history was unremarkable.
She was 151.1-cm tall and weighed 38.8 kg. Oxygen saturation was 95% on room air. Other vital signs were stable. Right lung sounds were diminished. Chest CT showed a possible bulla on the right upper lobe. No other possible causes of pneumothorax were found. Four recurrent episodes of right-sided pneumothorax, at least two of which occurred in association with menstruation, indicated the possibility of catamenial pneumothorax. Therefore, thoracoscopy was performed for definitive diagnosis.
On induction of general anesthesia, attempts at conventional intubation procedures failed. Additional attempts with a 32 French double lumen tube, single lumen tube (with cuff) with an inner diameter of 6.5, 6.0, 5.5, and 5.0 mm all failed. After various trials, intubation finally succeeded with a 5.0-mm pediatric tube (without cuff). During surgery, airway pressure elevated, complicating the course of mechanical ventilation. Intermittent manual ventilation was necessary for safe ventilation. There were no visible blebs or ectopic endometrium on the pleura, and the etiology of the recurrent pneumothorax was unclear. Residual scarring and localized pleural thickening were found on the right lung apex. A sealing test was performed and there was no air leakage. Sheet-type collagen was applied to the lung apex in attempt to prevent the recurrence of pneumothorax. The surgery was otherwise uneventful, and the patient was safely extubated immediately after the surgery. The postoperative course was also uneventful.
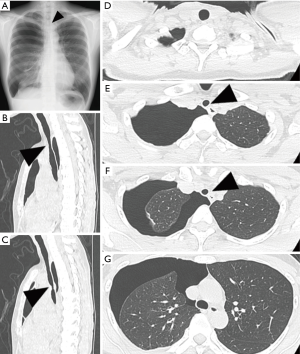
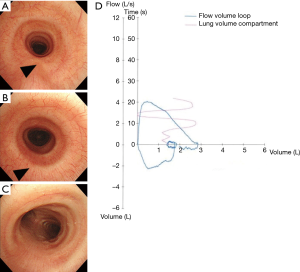
After the surgery, pre-surgical X-ray and CT were rechecked. They had both shown bronchial narrowing but was left unnoticed prior to surgery (Figure 1). Postsurgical bronchoscopy revealed partial tracheal stenosis due to complete tracheal rings (Figure 2A-C). There were no findings suggestive of an underlying acquired disease such as benign or malignant tumor, tuberculosis, sarcoidosis, polychondritis, amyloidosis, or inflammatory granulomas. She had no history of intubation, trauma, infection, or other systemic disease. There were no findings suggestive of idiopathic tracheal stenosis, such as progressive dyspnea, wheezing, or tracheal inflammation. Therefore, we diagnosed her as CTS. Spirometry showed a characteristic trapezoid flow volume loop, consistent with airway stenosis (Figure 2D). Spirometry had not been performed prior to surgery due to the risk of pneumothorax recurrence.
We explained the condition thoroughly to the patient and family, with emphasis on the importance of preventing respiratory infection. We made sure they would inform medical staff in advance should she ever need intubation. Right-sided pneumothorax continued to recur. A diary of her menstrual cycle and pneumothorax revealed an apparent relation between the two, leading to the diagnosis of catamenial pneumothorax. Her irregular menstrual cycle had made it difficult to identify the correlation. Hormonal therapy was initiated, decreasing the frequency of pneumothorax. There have been no episodes of respiratory distress or asthmatic attacks.
Discussion
We experienced an extremely rare case of adult CTS. CTS is a rare condition almost always diagnosed in infancy due to stridor, wheezing, and various degrees of respiratory distress (1). More than 75% are complicated with other anomalies, leading to the necessity of early surgical intervention (2). In particular, cardiopulmonary abnormalities such as pulmonary artery sling, cardiac defects, and lung hypoplasia or agenesis are seen most commonly. In mild stenosis, careful observation without surgery may be an adequate option. A small percentage may not present until childhood. However, it is extremely rare that patients survive undiagnosed. To the best of our knowledge, in English and Japanese literature, there have been only twelve reported cases of CTS discovered in adults, or those 18 years or older (Table 1) (3-14).
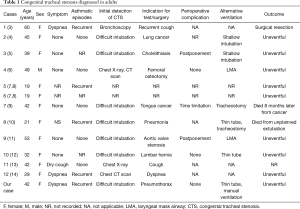
Full table
Of these 12 cases, three were diagnosed on images prior to intubation (6,13,14). Our case and six others were found only when intubation failed (4,5,9-12). All cases required adjustment of intubation procedures. Some cases required surgery postponement (5,11), surgery duration shortening (9) or additional invasive methods such as tracheostomy (9,10). Difficult intubation is a potentially lethal airway emergency. Moreover, multiple attempts at intubation through a narrowed trachea may cause tracheal mucosal edema and worsening of the airway narrowing. These are all preventable with the adequate awareness of the clinician. In all cases, the tracheal stenosis was already shown on X-ray and CT images prior to intubation. This highlights the importance of observing the bronchus carefully on images prior to intubation. The frequency of CTS may be underestimated (13).
Among the adult CTS cases, four had recurrent asthmatic episodes (3,8,10,14). When CTS is complicated with respiratory infection, patients are prone to asthma-like episodes of wheezing and dyspnea. This is attributed to increased airway secretion and edematous changes of the airway mucosa. In patients with recurrent wheezing resistant to asthma treatment, CTS should be kept in mind. Our case had asthma attacks and refractory atopic dermatitis since childhood. The following findings suggests the patient’s allergic tendency: fractioned exhaled nitric oxide level 45 ppb, thymus and activation-regulated chemokine 62,660 pg/mL, immunoglobulin E 14,200 IU/mL. Therefore, we assume our case actually had bronchial asthma. CTS complicated with asthma may cause more severe respiratory distress during an asthma attack. These patients may be at higher risk of intubation. In treatment resistant asthma, chest images should be revisited to rule out CTS (10,14).
Various airway management techniques have been reported for adult CTS cases. For example, shallow intubation stationed proximal to the tracheal narrowing (4,5), and utilization of a thin tube without cuff (10,12) or laryngeal mask (6,11). Laryngeal mask may have been an adequate alternative method of ventilation in our case. However, all of the above is limited to case reports. There are no established airway management techniques yet. Elevated airway pressure may necessitate manual ventilation. Utmost care is also required in selecting the optimal site and tubing for tracheostomy (10).
There is no sufficient data on the treatment and long-term prognosis of adult CTS. The few reports so far have focused on its diagnosis and surgical management. Asymptomatic adult CTS patients may eventually develop respiratory symptoms with recurrent infection or aging. Is surgical treatment recommended in these cases, or should preventative methods such as airway stenting or other bronchoscopic measures be taken? Further studies and accumulation of cases are awaited. Needless to say, the active effort to discover underlying cases is essential.
Acknowledgements
The authors would like to express their utmost gratitude to Dr. Maki Kawaguchi for taking quick and appropriate measures to the emergent situation.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Chen JC, Holinger LD. Congenital tracheal anomalies: pathology study using serial macrosections and review of the literature. Pediatr Pathol 1994;14:513-37. [Crossref] [PubMed]
- Schweiger C, Cohen AP, Rutter MJ. Tracheal and bronchial stenoses and other obstructive conditions. J Thorac Dis 2016;8:3369-78. [Crossref] [PubMed]
- Oka M, Haga H, Nakazato H, et al. Possible congenital tracheal stenosis in a 60-year-old female. Nihon Kyobu Shikkan Gakkai Zasshi 1984;22:1027-32. [PubMed]
- Saito S, Dohi S, Tajima K. Failure of double-lumen endobronchial tube placement: congenital tracheal stenosis in an adult. Anesthesiology 1987;66:83-5. [Crossref] [PubMed]
- Esener Z, Tür A, Diren B. Difficulty in endotracheal intubation due to congenital tracheal stenosis: a case report. Anesthesiology 1988;69:279-81. [Crossref] [PubMed]
- Asai T, Fujise K, Uchida M. Laryngeal mask and tracheal stenosis. Anaesthesia 1993;48:81. [Crossref] [PubMed]
- Grillo HC. Slide tracheoplasty for long-segment congenital tracheal stenosis. Ann Thorac Surg 1994;58:613-9 discussion 619-21.
- Grillo HC, Wright CD, Vlahakes GJ, et al. Management of congenital tracheal stenosis by means of slide tracheoplasty or resection and reconstruction, with long-term follow-up of growth after slide tracheoplasty. J Thorac Cardiovasc Surg 2002;123:145-52. [Crossref] [PubMed]
- Shiga K, Tateda M, Yokoyama J, et al. An adult case of asymptomatic congenital tracheal stenosis. Nihon Jibiinkoka Gakkai Kaiho 1999;102:1258-61. [Crossref] [PubMed]
- Nagappan R, Parkin G, Wright CA, et al. Adult long-segment tracheal stenosis attributable to complete tracheal rings masquerading as asthma. Crit Care Med 2002;30:238-40. [Crossref] [PubMed]
- Fujimoto K, Yamaguchi A, Kawahito K, et al. Use of a larynyngeal mask airway during aortic valve replacement. Jpn J Thorac Cardiovasc Surg 2003;51:308-10. [Crossref] [PubMed]
- Nakamura H, Takahashi T, Hashimoto H, et al. A case of congenital tracheal stenosis discovered during general anesthesia. Masui 2003;52:1153-4.
- Yokomura K, Chida K, Suda T, et al. An adult case of asymptomatic congenital tracheal stenosis. Nihon Kokyuki Gakkai Zasshi 2005;43:673-7. [PubMed]
- Numasaki M, Ohrui T, Sato A, et al. Congenital tracheal stenosis and an anomalous origin of the right upper lobe bronchus. Lancet 2008;371:1526. [Crossref] [PubMed]


