Transcatheter closure of a large patent ductus arteriosus using jugular access in an infant
Introduction
Patent ductus arteriosus (PDA) is a common congenital heart defect accounting to 5–10% of all congenital heart diseases (1). Trans-catheter occlusion using Amplatzer duct occluder (ADO) is nowadays considered to be a safe and effective method (2,3). Femoral venous access is the commonly used route as it allows delivery of larger sheath if necessary. In case femoral route is not feasible trans-jugular access may be used as an alternative. However, only few cases have been reported in children with interrupted inferior vena cava (4-7). We report a case of trans-jugular approach in an infant with large PDA.
Case presentation
A 6-month-old male infant, weighing 8 kg was admitted for percutaneous catheter closure of PDA. On examination, a continuous murmur was heard beneath the left clavicle. The echocardiogram at admission showed a 4.5 mm diameter and high velocity 5 m/s by continuous wave Doppler duct. The left atrium and left ventricle were significantly dilated.
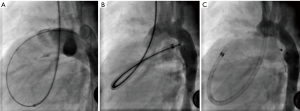
We obtained written and informed consent from the parents for trans-catheter device closure of the duct. At cardiac catheterization, femoral venous access was not possible. On the left, there was a swelling noted at the inguinal region, which was presumably a hernia. On the right groin, femoral vein access could not be obtained despite successful arterial access. We then decided to use the right internal jugular vein for the procedure. After a 6-French short sheath was successfully implanted in the right internal jugular vein, a lateral aortic angiogram was performed through a 4-French pigtail catheter. The duct measured 4.5 mm. A 4-French right Judkins catheter was used to catheterise the right heart cavities. The duct was successfully crossed and a 0.035 J tip guidewire (Wholey hi torque, Medtronic Inc., Minneapolis, MN, USA) was advanced in the descending aorta (Figure 1A). An 8/6 mm ADO (AGA Medical Corporation, Golden Valley, MN, USA) was advanced and positioned inside the duct through a 6-French Amplatzer Torqvue long sheath (Figure 1B). After the device was released, an aortic angiogram demonstrated successful closure with tiny residual shunt (Figure 1C). There were no complications. Post procedure echocardiogram showed no residual shunt across the duct. The patient was discharged after 24 h. At 3 months’ follow up patient was well and echocardiogram showed intact device with no residual shunt.
Discussion
The jugular vein is larger than the femoral vein therefore a large bore sheaths can be safely introduced. However, the trans-jugular approach for PDA occlusion can be more challenging and potentially poorly tolerated as compared to femoral access. This is due to the angulations of the catheter from the right atrium to the pulmonary artery and pulmonary artery to the aorta. Indeed, the tortuosity of a large sheath alongside the rigidity of the delivery system and of the loaded device may transiently compromise the function of the right ventricle, tricuspid and pulmonary valve. In this setting the risk of “mechanical” ventricular arrhythmia is not negligible (8). Finally, in case with such difficult femoral access ultrasound guidance is safe and more effective (9). Unfortunately, this was not available in the centre where the case was performed.
To our knowledge this is the fifth case described. The 4 previously published cases (Table 1) of successful trans-catheter occlusion of the PDA through jugular access were due to interrupted inferior vena cava (4,5,7) and pseudo interrupted inferior vena cava (6). Aggarwal et al. described the technical difficulties while attempting to close the duct via the inferior vena cava-azygous route. They used J tip terumo wire as a snare through the femoral artery to stabilise the catheter and had a difficult tract for the delivery sheath with two angulations. The PDA was subsequently closed successfully via trans-jugular route (7). In our case the use of a relatively soft wire (Wholey hi torque, Medtronic Inc., Minneapolis, MN, USA) instead of a super stiff wire was helpful to carefully advance the long sheath through the PDA.

Full table
The youngest child undergoing trans-jugular closure was 19-month-old described by Subramanian et al. (6). Our case is the first to describe the trans-jugular approach in an infant with a large PDA. Despite small weight and size of the patient we found that the trans-jugular approach was well tolerated in terms of crossing the duct with a large sheath and deploying the device.
Conclusions
The trans-jugular approach seems to be a good alternative to femoral access for trans-catheter closure of PDA in infants. Experience is however necessary to perform this procedure safely and effectively.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: We obtained written and informed consent form the parents for trans-catheter device closure of the duct.
References
- Schneider DJ, Moore JW. Patent ductus arteriosus. Circulation 2006;114:1873-82. [Crossref] [PubMed]
- Wang JK, Wu MH, Hwang JJ, et al. Transcatheter closure of moderate to large patent ductus arteriosus with the Amplatzer duct occluder. Catheter Cardiovasc Interv 2007;69:572-8. [Crossref] [PubMed]
- Baruteau AE, Hascoët S, Baruteau J, et al. Transcatheter closure of patent ductus arteriosus: past, present and future. Arch Cardiovasc Dis 2014;107:122-32. [Crossref] [PubMed]
- Patel NH, Madan TH, Panchal AM, et al. Percutaneous closure of patent ductus arteriosus via internal jugular vein in patient with interrupted inferior vena cava. Ann Pediatr Cardiol 2009;2:162-4. [Crossref] [PubMed]
- Akhtar S, Samad SM, Atiq M. Transcatheter closure of a patent ductus arteriosus in a patient with an anomalous inferior vena cava. Pediatr Cardiol 2010;31:1093-5. [Crossref] [PubMed]
- Subramanian V, Mahadevan KK, Sivasubramonian S, et al. Pseudo interruption of the inferior vena cava complicating the device closure of patent ductus arteriosus: Case report and short review of venous system embryology. Ann Pediatr Cardiol 2014;7:64-6. [Crossref] [PubMed]
- Aggarwal N, Agarwal M, Joshi R, et al. Device closure of patent ductus arteriosus in interrupted inferior vena cava. Indian Heart J 2015;67 Suppl 3:S85-7. [Crossref] [PubMed]
- Ravndal MEA, Christensen AH, Døhlen G, et al. Paediatric cardiac catheterisation in Norway: rates and types of complications in new terms. Cardiol Young 2017;27:1329-35. [Crossref] [PubMed]
- Vezzani A, Manca T, Vercelli A, et al. Ultrasonography as a guide during vascular access procedures and in the diagnosis of complications. J Ultrasound 2013;16:161-70. [Crossref] [PubMed]


