Chun Chen: the “practices” and “philosophy” of a surgeon
In 1997, a review from Henrik Kehlet, a Danish professor, on how to control the morbidity and mortality associated with major surgeries was published. In this article, he officially proposed the concept of enhanced recovery after surgery (ERAS), an idea of utilizing multi-modal strategies to facilitate patient recovery (1).
In 2007, initiated by Jieshou Li, Academician of the Chinese Academy of Engineering, and other experts, the General Surgery Department of Nanjing General Hospital of Nanjing Military Command was the first to practice ERAS in China. Professor Zhiwei Jiang and Academician Jieshou Li published the first clinical research on the application of ERAS in gastric cancer surgery in the world (2). Since then, the concept of ERAS has become better known in China.
In the following 10 years, ERAS has become widespread in clinical surgery in China: many associations set up the ERAS commissions/groups, the experts of various subspecialties reached ERAS consensuses, and through practices, clinical departments of hospitals have developed a series of measures based on China’s conditions. So far, thousands of patients have benefited from ERAS.
The essence of ERAS is to utilize a series of evidence-based preoperative, intraoperative, and postoperative optimization measures to reduce patients’ physiological and psychological stress response after surgery and to speed up recovery ultimately. Among these measures, perioperative airway management constitutes one of the most important part of ERAS, especially in the thoracic surgery, as it effectively reduces complications, shortens hospital stay, lowers readmission rate and mortality risk, improves prognosis, and decreases healthcare costs (3).
Therefore, AME Publishing Company has planned and launched this special issue of “ERAS and Perioperative Airway Management | Meeting the Experts”, where over 10 opinion leaders in ERAS have been invited to reflect and share their perspectives on the concepts and practices of ERAS, perioperative airway management, and expectations for the future.
Expert's introduction
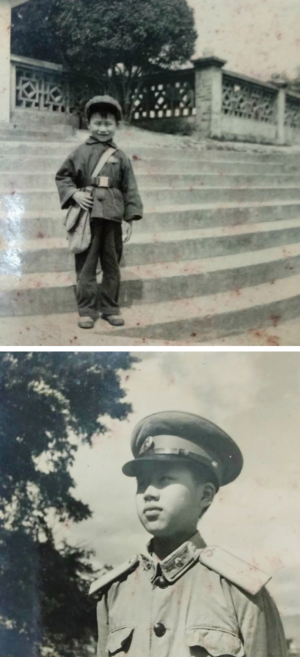
Chun Chen (Figure 1) is the vice president of the Union Hospital of Fujian Medical University, director of the Thoracic Surgery Department, PhD & MD in surgery, chief physician, and supervisor for doctoral candidate. He is a member of the International Association for the Study of Lung Cancer (IASLC), standing committee member of Chinese Association of Thoracic Surgeons, vice president of Chinese International Exchange and Promotion Association for Thoracic Surgery, head of the Group of Minimally Invasive Esophageal Surgery and Three Field Lymphadenectomy, standing committee member of the Lung Cancer Commission and the Esophageal Cancer Commission of Chinese Anti-Cancer Association, member of the Mediastinum Group of Chinese Society for Thoracic and Cardiovascular Surgery. He is the first chairman of Fujian Society for Thoracic Surgery, president of Fujian Cross-Straits Association of Cancer Prevention and Treatment, vice chairman of the Thoracic Surgery Commission of Cross-Straits Medicine Exchange Association, dual-disciplinary professional in Fujian province, and Expert of Outstanding Contribution from Fujian Health and Family Planning Commission. He is committed to research in thoracic tumors and clinical application of minimally invasive thoracic surgery. His expertise lies in minimally invasive surgery for lung cancer and esophageal cancer. So far, he has undertaken over 10 research projects at provincial or above levels and published over 30 papers on SCI-cited and key journals in China. Under his leadership, his department ranked among the top 5 thoracic surgical services in east China in China’s Hospital Rankings, released by Fudan University, for 3 consecutive years (2014–2016), and was nominated for Chinese top 10 thoracic surgical services in 2016 Chinese Hospital Specialist Reputation Rankings released in November, 2017, the best place ever for thoracic surgery services of Fujian province.
JTD: As a doctor, what do you think of your job?
Chun Chen: It’s a fantastic job. As doctors, we’ve got to master the basic skills and do everything accurately and perfectly in order to help the patients. Sometimes, if we advance the scalpel by 1 mm, it may cut the arteries; other times, if we fall short by 1 mm, we may leave behind residual tumor. We need to be strict and precise. I often tell my patients that we are the performers of surgery and they are the recipients. If things go wrong with the surgery, it does not help to say “I’m sorry I didn’t do it well”, because it may cause patients lifelong pains, or even cost their life.
JTD: As a teacher, do you have any suggestions for the young people to take care of the present and well prepare for the future?
Chun Chen: Many young doctors are too eager for success. They want to do every part of a surgery by themselves only after learning some basic surgical skills. I think it’s really dangerous. Just like toddlers, at the age of four or five, they are most likely to fall, because despite the basic walking skills they have gained, they have no idea about the risks going forward. Young people should first set their goals, and then try to do their job well with patience. This is the key point for them to live in the present and seize the future. A surgeon, for example, should master the knowledge and communication skills and behave gently to lay a solid foundation for surgery before developing their unique strengths that make themselves better than and different from others.
JTD: If you were not a doctor or teacher, what do you want to be?
Chun Chen: I am particularly attached to soldiers and I really appreciate their fighting spirit. My father was a military doctor. I grew up with my father’s story about his experience in guerrilla wars. He told me that, for example, in a battle, only 5 of the 23 soldiers of his platoon survived. When I applied for admission to university, I was most interested in the military medical universities, where I can fulfill my aspiration to be both a doctor and a soldier. Unfortunately, I was rejected due to suboptimal visual acuity. It has been many years since my father served the military and since I applied for the military medical university, but still, after I watched the film Youth together with my father, it struck a responsive chord in our hearts. (Note: the Chinese film Youth chronicles the lives of a group of idealistic adolescents in a military art troupe in the People’s Liberation Army during the Cultural Revolution.)
My doctor dream and military dream
In 1966, Chun Chen was born in a military camp. He grew up in the barracks as his father was a military doctor in the army. Influenced by his father, he was full of respect and longing for both soldiers and doctors.
“In the army, whenever called upon for help in the middle of the night, he took his medicine kit and left home without hesitation or complaints. After he retired, he has always been ready and willing to help our neighbors with slight illness.” said Dr. Chen when recollecting his childhood.
In 1981, Chun Chen was enrolled in Fujian Medical University at the age of 15. Since he most aspired to a career in medicine and military, almost all of his university applications were related to the “medicine” and “military schools” (Figure 2). However, he failed to have both of his dreams come true at the same time because he did not meet the eyesight requirements of the military schools.
In 1986, Chun Chen graduated from Fujian Medical University at the age of 20, and started his rotation in Fujian Medical College Affiliated Hospital (now Union Hospital of Fujian Medical University). As a straightforward person appreciating the solider-like shrewdness of surgeons who won recognition from the then director of the Thoracic Surgery Department, he decided to choose thoracic surgery as his specialty during the rotation to the Thoracic Surgery Department.
“The Union Hospital was closed in 1969, and all staff were disbanded and sent to rural areas. We had a hard time when the hospital was reopened in 1984, with only one building (the red mansion) in the hospital. In 1986, we only had 9 sickbeds in the Thoracic Surgery Department. Despite the shabby conditions, there were a lot of work to do. At that time, the Thoracic Surgery Department was actually Cardiothoracic Surgery Department which was also responsible for cardiac surgery, so our job was anything but easy. However, hard as it was, we should get it done. Otherwise, what about patients? We can go forward step by step and solve the problems one by one.”
Since then, he embarked on his 30-year career in thoracic surgery based in the Thoracic Surgery Department of the Union Hospital of Fujian Medical University.
Hardworking
“Genius is 30% inspiration and 70% perspiration. No pains, no gains.” Just as what is written in the lyrics of the famous song in South Fujianese dialect No Pains, No Gains, Chun Chen is an ultimate southern Fujian man who really goes all out in work.
In the hospital, he is among the clinical front-line colleagues. He carries on making ward rounds every morning even though as a chief physician, he is required to do it only once a week. He starts from 7:30 o’clock and spends about 45 minutes for a round. Sometimes he selectively makes rounds again at night.
If not in the hospital, he is out for study. For more than a decade, he has been working almost all year around. On weekends he often travels to other cities for exchanges and studies with other colleagues. According to the doctors familiar with him, if you are to visit him, you’d better come during the working time from Monday to Friday, and almost everyone knows that he goes out for ongoing study on weekends.
Innovation
People often confuse “hardworking” and “foolhardy”, but Chun Chen never mistakes it. His innovations prove it. In his eyes, innovation is not a slogan, but something embodied in real-world practices.
In 2008, Chun Chen pioneered the “esophageal suspension method” with patient in lateral decubitus position in China for the dissection of the lymph nodes around the left recurrent laryngeal nerve, which has significantly reduced the incidence of hoarseness after surgery, enhanced the efficacy of lymph node dissection, and afforded patients better quality of life. He leads the nation in this technique (Figure 3).
In the same year, he led the province in starting the conventional three-port technique for thoracoscopy, and then developed the modified bronchial sleeve anastomosis (featuring a quarter-based approach to suturing the bronchial lumen), which was the first case reported in the world.
In 2016, he performed the first da Vinci robotic thoracic surgery in Fujian, unfolding the robot era of Fujian healthcare services.
His endeavors and innovations ranked him among the top 10 esophageal surgery specialists as listed in 2015 and 2016 Top 100 Chinese Doctors, and led his department to the nomination of the nation’s top 10 thoracic surgery departments in 2017 China’s Hospital Rankings, the best results ever in the history of thoracic surgery of Fujian province (Figure 4).
When asked why he is so innovative, he modestly repeated that sometimes he was just looking for tricks and then inspiration strikes; but more often, innovations come from deep reflection and are realized with teamwork. Still, he generously shared his experience of innovation:
Before making innovations, you should lay a solid foundation first, just as before practicing martial arts, you should master the stable horse stance first. With a mastery of the basic skills, you will gradually become proficient in whatever you do, whether it is lung segmentectomy, esophageal cancer surgery, or robotic surgery.
Then, you should learn to catch problems and raise questions. There are many doctors who have conducted many surgeries but gained nothing from them.
Besides, keep studying, learn from others, and never be afraid to try. Through research, learning from others and exploration, we created the “esophageal suspension method” for lymphadenectomy of the left recurrent laryngeal nerve with patient in the lateral decubitus position. In the past, we found that in esophageal cancer surgery, it was hard to approach the left recurrent laryngeal nerve lymph nodes as they were deeply hidden. What should we do? Later, we learned from Professor Lijie Tan that a good exposure can be obtained in the lateral decubitus position, so we adopted this method. Things improved in this way, but still it was not that satisfactory. Can we make it better? We went out to see, to learn, and to find solutions, we discussed together, and finally came up with an idea: can we suspend the esophagus? Eventually, the lymph nodes around the left recurrent laryngeal nerve are perfectly dissected when the esophagus is suspended and patient in the lateral decubitus position. Professor Tan also uses this method now. Both of us learn from each other and draw on others’ experience.
Breakthrough
As it is put in The Book of Changes, “Metaphysical problems constitute philosophy, and physics problems lead to practices”.
If lymphadenectomy around the left recurrent laryngeal nerve with “esophageal suspension” in lateral decubitus position and the “quartered-based” modified bronchial sleeve anastomosis represent Chun Chen’s innovation in medical techniques and in “practices”, then his proposal of the whole process management of esophageal cancer embodies his breakthrough in medical ideas and in “philosophy”.
Though patients have benefited a great deal from the new techniques and methods of esophagus cancer surgery, Chun Chen was beset with their high morbidities and prolonged hospital stay after surgery.
“Sometimes the surgery was successfully done, but the patients suffered anastomotic leakage or respiratory failure after surgery. Doctors were disappointed and frustrated, and nurses had to keep changing dressings all day long. Therefore, I thought it’s time to make improvement.”
Right then, ERAS came to him. Based on the concept of ERAS, Chun Chen put forward the idea of “whole process management of esophageal cancer” and took the initiative to develop new techniques for ERAS, which has achieved remarkable results by reducing the incidence of anastomotic leakage after esophageal cancer surgery from 30% to 1.3%.
“The whole process management of esophageal cancer is to conduct systematic management of patients before, during and after surgery with the joint efforts of nursing, rehabilitation, surgery and anesthesia teams. This management method has largely reduced the complication rate, with no anastomotic leakage found among over 100 patients undergoing esophageal cancer surgery. It sounds incredible even to us. Before we did this, the entire inpatient area became busy if anastomotic leakage was formed. But now, during rounds, we see everyone sound and stable after surgery. We are dealing with more and more surgeries but coping with less and less workload from each case. Meanwhile, patients enjoy fast recovery and early discharge.”
Being a teacher
When it comes to teachers, it is put in the ancient prose On Teaching that, “A teacher is one who propagates the doctrine, imparts knowledge, and resolves confusion.” And also, as the old saying goes, “a teacher for one day is a father for a lifetime”.
As a teacher, Chun Chen has met these centuries old standards in the Chines society by imparting knowledge to his students, helping them clearing up confusion and treating them as his own kids (Figure 5).
Not being content with his own studies of professional knowledge and skills, he has also made painstaking efforts to train young doctors. He developed a set of “modular” training program to help the young doctors move forward step by step, save them from unnecessary twists and turns, and promote their performance quickly. At present, his training mode has been highly recognized nationwide among counterparts.
When mentioning the young doctors, he likes to call them “the kids” with effusive love and warmth.
“As an individual’s ability is limited, it is important for the team to make a concerted effort with the contribution of every team member. It’s hard for a surgeon to improve himself/herself after his/her skills reach a certain level. And if his/her skills cannot be passed on, all the efforts become in vain. Therefore, I try my best to help the kids wherever I can do so.”
“Modular training starts with the basics by helping the kids master the fundamental knowledge and entry-level skills, and then goes deeper step by step to the more complicated and difficult parts. Instead of throwing these kids to all kinds of difficult surgeries all at once, the program allows them to progress from easy to hard, and from simple to complicated levels. In this process, senior doctors will offer advice and instructions at their side. If we do not keep an eye on them or do not teach them in this way, they are bound to take detours.”
This is Chun Chen, a hardworking man from southern Fujian, an innovative practitioner, a pioneer with ground-breaking ideas, a teacher regarding his students as “the kids”, and a thoracic surgeon aspiring to be a doctor and solider since childhood.
He has lived up to the ancient idea that “a superior man is not a utensil” (Annotation: a superior man won’t be content with his achievements in one field. Rather, he is knowledgeable and capable to live in a changing environment).
Interview
JTD: What’s your understanding of ERAS?
Chun Chen: As you know, we have attached great importance to ERAS in recent years. Actually, many things that we had been doing were consistent with this concept, though no one summarized those practices into a title or theory. Now in China, many people have a partial understanding of ERAS, equaling it to an improved surgical step or a well-done surgery. In fact, ERAS is a comprehensive, in-depth and systematic concept covering preoperative, intraoperative as well as postoperative care and requiring teamwork of nursing, rehabilitation, surgery, and anesthesia professionals. It is a complete system with both high-quality techniques and high-quality services.
JTD: How do you perform ERAS?
Chun Chen: We mainly apply ERAS in esophageal cancer, because it is a unique disease requiring a complicated operation. If there is anything wrong with one or two steps in the operations, it will result in complications, usually life-threatening and difficult to handle.
First of all, we have improved preoperative assessment and nursing. For example, we pay close attention to patients with respiratory tract lesions. We maintain good airway management by instructing patients how to cough and how to take a deep breath, send patients with impaired pulmonary function to the Pneumology Department for recuperation, and perform proper preoperative assessment on high-risk patients with diabetes mellitus, hypertension, or with suspected varicosities or thrombus.
During surgery, we focus on the three major complications with the esophageal cancer surgery, namely recurrent laryngeal nerve impairment, anastomotic leakage, and severe pulmonary infection caused by prolonged surgery or intubation.
After surgery, we make good use of our bronchoscope, a privileged asset, and every young doctor knows how to use it for sputum suction. It’s known that patients of esophageal cancer are often admitted to intensive care unit (ICU) after surgery due to lung infections, sputum obstruction, etc. Now when patients are found to have sputum obstruction or difficulty in sputum excretion and may need intubation, we can readily help them with sputum suction under bronchoscopy. Meanwhile, we work on preventing anastomotic leakage. We noticed that postoperative anastomotic leakage is rare now, thanks to the advanced technologies. So, most of the leakage cases are late-onset. According to our protocol, though the feeding tube is removed 8 days after surgery, the patients are not recommended to eat anything. They will be provided with nutrition through enterostomy and do not start to eat until 15–20 days after surgery. “No fistula formed” is a gold standard for care as we do everything for patients to go home lightheartedly.
Such care reduces the incidence of anastomotic leakage from 30% to 1.3%.
JTD: This is really impressive. Can you give us a few examples to explain how you made it?
Chun Chen: Take the control of serious complications as an example. In thoracoscopic surgery for esophageal cancer, many patients ended up with a trachea-gastric fistula after esophageal resection, a severe complication. We encountered four or five cases like this. Through efforts of the care team, the fistula was put under control in most of the cases, but patients endured great pain and suffering; and some passed away despite all that had been done. Then we drew out some lessons. For patients with gastro-tracheal fistula that has not resulted in extravasation, conservative therapy is adopted; otherwise, the plastic surgeons are invited to perform myocutaneous flap inversion for fistula closure and tissue repair. This technique has turned out effective in several cases.
Another example is that, as we know that the most difficult part of lymphadenectomy is for those around the left recurrent laryngeal nerve. In the past, we just tried to push down the esophagus or pulled it forward, but the result was not satisfactory. After several brainstorming sessions and trials with our team members, we found that the problem can be solved simply by lifting up the esophagus, and the dissection results were good. This method has also been adopted by other surgeons, especially during surgeries in lateral decubitus position.
We call it the “suspension method”. It was originally performed with electric hooks, which could be beautifully done but contributing to a high rate of hoarseness in patients. Later we attributed it to the nerve injury caused by electric shock. Therefore, we now use an ultrasonic knife to do the dissection instead. In addition, we found that during cervical anastomosis, if the tracheal-esophageal release is stopped too low, the nerves are still clung to the esophagus above the release level and therefore dragged when the esophagus is pulled against the neck. Therefore, the release should go higher so that surgeons see the nodes more clearly and reduce injury. With our efforts in these two aspects, now the postoperative hoarseness rate is at a very low level. I think it is a great practice.
JTD: ERAS covers preoperative, intraoperative and postoperative care, which requires the cooperation of nursing, rehabilitation, surgery and anesthesia teams. How do you collaborate with each other?
Chun Chen: Besides cooperation of nursing, recovery, surgery and anesthesia teams, we also designate task teams. For example, we have a nursing team responsible for perioperative airway management. What’s more, doctors are assigned different tasks based on their seniority and they work together. Most young doctors are responsible for improving patients’ physical conditions before surgery and postoperative monitoring, while the senior doctors are more engaged in the surgery. I oversee the whole process and give guidance.
JTD: Why do you designate a team for perioperative airway management alone?
Chun Chen: Perioperative airway management is a vital part of ERAS. “It’s the breath of life”. It is even more important than some perioperative and postoperative measures, as it has a direct bearing on the prognosis of the patients.
JTD: Is there anything that needs our special attention in perioperative airway management?
Chun Chen: It’s important to keep the respiratory tract unobstructed before, during and after surgery, monitor the changes of the small airway and signs for airway obstruction, and well manage airway anesthesia during surgery. Putting all these things together, it is a systematic process for preoperative, intraoperative and postoperative care.
Before surgery, a special part of the process involves respiratory training, coughing exercise, breathing exercise, treatment for comorbidities, etc. Patient management is tailored to their status of obstruction, comorbidity, physical fitness and weight, resulting in individualized care. During surgery, the procedures should be carried out reliably, accurately, swiftly, and efficiently as much as possible, because we position patients in lateral decubitus, and pneumonia often occurs to the down side. The shorter the operation time is, the more the patients can benefit. Meanwhile, it’s important to maintain patients’ body temperature during surgery; otherwise, postoperative pulmonary infection may get worse. After surgery, we closely observe and monitor the lung and the patency of the trachea so as to detect and treat problems timely.
JTD: You have made significant achievements in curing both esophageal cancer and lung cancer, and therefore you are honored as a dual-disciplinary specialist. What are the main similarities and differences in terms of ERAS between esophagus and lung cancer?
Chun Chen: Lung cancer surgery is highly risky, but patients can recover quickly after surgery. In contrast, esophageal cancer surgery is a more sophisticated project that involves more details to look for and more steps. Esophageal cancer surgery seems to be less dangerous with low bleeding risk, but actually it comes with more complications. This is the main difference between them.
However, they also have similarities: both require minimally invasive procedures and good management of preoperative, intraoperative, and postoperative care. In particular, it is important to watch out for bleeding and air leaks during surgery. If the surgeon keeps an eye out for the leak point and tie it off timely, the patient will probably be discharged from hospital 3 days after surgery; but if the doctor is “lazy” and ignores the wound surfaces and the leak points, the patient may have to stay in hospital for over one week. These are the factors under the control of the doctors during the surgery. In fact, this reflects the essence of ERAS: as long as the doctors spend a few more minutes on the operation table, and the patients, doctors, and nurses all benefit.
JTD: In your opinion, what’s the role of ERAS in the development of thoracic surgery?
Chun Chen: ERAS marks a milestone of higher requirements for medical quality.
JTD: In recent years, China has accumulated enormous experience in ERAS. How good are we compared to the rest of the world?
Chun Chen: Over the past decade, more and more healthcare professionals have devoted to the details in medical care. As we are starters, the details we worked out are still a little bit crude, but we have come a long way. I believe we will refine the works in the future. We can’t say we are ahead of the world, but I think we are leading in many ways. Ten years ago, we learned endoscopy from other countries. Now, they come to learn our endoscopic techniques. This proves our progress, though it’s a slowly developing process.
JTD: In which aspects do you think we can do better in the next decade?
Chun Chen: I think a major barrier in China remains to be updating our mindset. Take endoscopic procedure for example, a decade ago, we focused on how to perform the procedures; during the last decade, we explored how to do it better. For the future, I believe the trend will be to do our job in a more detailed and refined way.
What’s more, effort should be made to bridge the gap between regions, urban and rural areas, as well as between academic leaders. I hope in the near future, there will be an authoritative statement, especially from those highly influential experts, that clarifies the concept of ERAS and propagates it to all services and regions, so as to benefit more patients, increase case volume and reduce average workload and labor intensity.
Postscript
January 3, 2018 was my first work day in the new year, and also the day to meet with Professor Chun Chen. When I arrived in Fuzhou (Fujian Province), I almost forgot it was still winter as it was such a warm city.
At 17 o’clock sharp, Professor Chun Chen showed up on time. At first sight, he was simply dressed and wore a pair of blue-rimmed glasses, with silver and black hair and a smile on the face. He was full of spirit and energy and didn’t show a slightest trace of tiredness after performing a surgery.
During the interview, he looked at me silently and listened to me carefully when I had questions, and never forgot to express his heartfelt thanks for my praises and recounted details in an impressive way.
Though I had known before the interview that he has received various honors and awards, such as the “Inventor”, “Pioneer”, “Leader”, “Dual-disciplinary Specialist”, “A Top-10 Esophageal Surgery Specialist in China’s Top 100 Doctors List” and “Masters of Cardiothoracic Surgery ACS-Covidien Video Contest”, I never expected that his office would be so simple, with only a desk, a computer, a chair, and a file cabinet. It was an office of several square meters that can only accommodate a few people. There were only books on the desk instead of awards or certificates of honors. To satisfy my curiosity, he opened the cabinet and found out those certificates buried under the thick files. At my request, he had a “rare” group photo taken with them as shown in Figure 4.
Acknowledgements
Special thanks go to Dr. Bin Zheng of the Thoracic Surgery Department, Union Hospital of Fujian Medical University, and Lili Liao of AME Publishing House for their contribution to this article.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Jiang ZW, Li JS, Wang ZM, et al. The safety and efficiency of fast track surgery in gastric cancer patients undergoing D2 gastrectomy. Zhonghua Wai Ke Za Zhi 2007;45:1314-7. [PubMed]
- Chinese Expert Consensus Statement on Multi-disciplinary Perioperative Airway Management. version) Expert Panel. Chinese expert consensus statement on multi-disciplinary perioperative airway management (2016 version). Chinese Journal of Clinical Thoracic and Cardiovascular Surgery 2016;2016:23.
(Science Editor: Kaiping Zhang, JTD, jtd@amepc.org)