Ventricular arrhythmias and sudden death in patients with Ebstein anomaly: insights from a retrospective cohort study
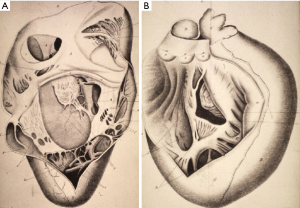
Ebstein anomaly accounts for <1% of all congenital heart defects (CHDs), with a prevalence of ~1 per 200,000 live births. In 1866, Wilhelm Ebstein described “A very rare case of insufficiency of the tricuspid valve, caused by a severe congenital malformation”. He reported the pathological findings of a 19 year-old cyanotic male, Joseph Prescher, who complained of shortness of breath and palpitations since childhood and subsequently died from heart failure. Ebstein’s meticulous description of the malformed tricuspid valve was complemented by the drawings produced by his colleague, Dr. Wyss, shown in Figure 1 (1). Ebstein anomaly is characterized by (I) adherence of septal and posterior tricuspid valve leaflets to the underlying myocardium, (II) downward (apical) displacement of the functional tricuspid annulus, (III) dilation of the “atrialized” portion of the right ventricle (RV), (IV) redundancy, fenestrations, and tethering of the anterior tricuspid valve leaflet, and (V) dilation of the right atrioventricular junction (2).
Despite major improvements in the care and outcomes of patients with Ebstein anomaly over the past decades, ventricular arrhythmias and sudden death remain feared complications. The incidence of life-threatening arrhythmias is poorly defined and the risk profile understudied, considering that the literature is largely limited to small retrospective studies. Within this context, Attenhofer Jost presented an analysis of their impressive single-center retrospective cohort of 968 consecutive patients with Ebstein anomaly managed at the Mayo Clinic between April 1972 and December 2015 (3). Patients were 25 years of age on average at first presentation, and 41.5% were male. Sustained ventricular arrhythmias [ventricular tachycardia (VT) or fibrillation (VF)] were combined with resuscitated cardiac arrest and sudden death into a composite outcome that the authors labeled “sudden death”. This outcome occurred in 65 patients during a follow-up that averaged 13.2 years, with 31 witnessed sudden deaths, 10 sustained VT/VFs, 10 resuscitated out-of-hospital cardiac arrests, and 14 unwitnessed deaths with autopsy reports or death certificates consistent with sudden death. When assessed from birth, corresponding 10-, 50-, and 70-year rates of ventricular arrhythmias/sudden death were 0.8%, 8.3%, and 14.6%, respectively.
Attenhofer Jost et al. are to be commended for undertaking the largest study to date on the incidence and predictors of ventricular arrhythmias/sudden death in patients with Ebstein anomaly. Assuming a linear risk, the estimated incidence of the combined outcome was ~0.2% per year, a finding consistent with prior reports (4,5) and within the range of CHD substrates associated with an increased risk for sudden death, such as tetralogy of Fallot (6,7). There are, however, numerous challenges to calculating incidence rates from retrospective studies. One important issue in estimating survival from birth in a predominantly adult cohort (i.e., average age 25 years at presentation) is so-called immortal-time bias. “Immortal-time” refers to a span of time during which it is impossible for at least one of the components of the outcome to have occurred. If a child with Ebstein anomaly died suddenly prior to presentation at the Mayo Clinic, that patient would have escaped detection. It is, therefore, not possible for a study patient to have died suddenly between birth and enrollment such that, statistically, selected individuals were “immortal” during this time frame. Not accounting for this bias can result in an under-estimation of the incidence of sudden death. Validated techniques to address immortal-time bias include Manel-Byar and landmark methods.
Conversely, an analysis of malignant ventricular arrhythmias and sudden death based on the experience of a single quaternary center with world-renowned expertise can result in an over-estimation of risk owing to the fact that more complex patients are preferentially referred. For example, most adults with Ebstein anomaly have mild forms and do not require surgery. In contrast, 80% of patients in Attenhofer Jost et al.’s study had severe Ebstein anomaly with tricuspid valve surgery performed in 83%. Given the potential for this referral bias to have a major impact on the estimated incidence of sudden death, results should not be extrapolated to the larger lower-risk population (3). This is particularly relevant to the issue of relying on such sudden death risk estimates in selecting appropriate candidates for primary prevention implantable cardioverter-defibrillators (ICD). Unlike tetralogy of Fallot for example (8), expert consensus recommendations have yet to specifically address primary prevention ICDs in Ebstein anomaly (9). In Attenhofer Jost et al.’s study, 24 (2.5%) patients had ICDs, 14 for secondary and 10 for primary prevention. Seven of 14 (50%) patients with secondary prevention ICDs received appropriate shocks. In contrast, no patient with a prophylactic ICD had appropriate anti-tachycardia pacing or shocks, a finding that precludes the identification of factors associated with ventricular arrhythmias and sudden death in primary prevention ICD recipients.
Despite such limitations, the study provides valuable insights. In an analysis that considered factors collected at the time of the first encounter at the Mayo Clinic, multivariable predictors of the composite outcome were history of VT [hazard ratio (HR) 6.0], heart failure (HR 5.7), tricuspid valve surgery (HR 5.9), syncope (HR 2.0), pulmonary stenosis (HR 3.4), and hemoglobin >15 g/dL (HR 2.1) (3). In exploratory analyses, additional factors associated with ventricular arrhythmias and sudden death not incorporated in the multivariable model included increased QRS duration, QTc interval >500 ms, left ventricular non-compaction, mitral regurgitation, and atrial arrhythmias. Despite the low prevalence of coronary artery disease (5.9%) in this young population, it was also significantly associated with the composite outcome (HR 2.4). This observation highlights the prognostic importance of acquired diseases in the aging population with CHD.
In general, much has been learned about the RV and its association with ventricular arrhythmias and sudden death by studying patients with CHD. In Attenhofer Jost et al.’s study, neither the anatomic severity of Ebstein anomaly nor degree of RV enlargement or tricuspid regurgitation was predictive of ventricular arrhythmias and sudden death, which contrasts with previous reports (5,10,11). It is difficult to know to what extent under-representation of patients with mild forms of Ebstein anomaly may have influenced these findings. RV systolic dysfunction did, however, exhibit a dose-dependent relationship with the composite outcome. While reasons underlying disparities between RV structural and functional parameters are unclear, the authors speculated that they may be due, in part, to limitations of conventional echocardiography, which may not adequately assess the shape of a crescentic RV that is dependent on left ventricular (LV) septal motion. It remains to be determined whether a more reliable determination of RV size and function provided by advanced imaging modalities, such as three-dimensional echocardiography or cardiac magnetic resonance (CMR), would result in consistent associations between RV metrics and ventricular arrhythmias and sudden death. Rydman et al. recently reported that CMR-derived indices of RV and LV function and volumes carried prognostic information regarding major adverse cardiovascular events in adults with unrepaired Ebstein anomaly (12). In addition, while the mean LV ejection fraction was normal in Attenhofer Jost et al.’s study (58.3%±8.3%), LV systolic dysfunction has been associated with poorer survival in other cohorts (13).
Prior reports have suggested that earlier presentation and diagnosis of Ebstein anomaly is associated with coexisting cardiac defects and poorer outcomes (10,14,15). The high event rate observed in Attenhofer Jost et al.’s study, in which most patients required surgical intervention, is concordant with these observations. Importantly, the authors observed a higher incidence of ventricular arrhythmias/sudden death in patients who underwent tricuspid valve surgery (3). A causal association cannot be established from a retrospective observational study where residual confounding remains a plausible alternative explanation. Nevertheless, Attenhofer Jost et al. raised the possibility that tricuspid valve surgery may itself have a proarrhythmic effect and called into question the need for and appropriate timing of surgical intervention (3). While tricuspid valve surgery has been shown to improve functional outcomes in selected patients with Ebstein anomaly (16), surgical proarrhythmic effects associated with ventriculotomy incisions and patches are well recognized in other forms of CHD, and ventricular arrhythmias have been reported after surgical repair of Ebstein anomaly (4). It could be hypothesized that the atrialized portion of the RV is particularly vulnerable to such proarrhythmic effects considering that, in our experience, ventricular arrhythmias can be induced by non-aggressive programmed stimulation at this site. The authors also reported that a bi-atrial Maze was strongly associated with ventricular arrhythmias and sudden death in comparison to a right-sided Maze (HR 18.4). Given the non-randomized study design, it is likely that the arrhythmia burden, a marker of poorer prognosis, was higher in patients with bi-atrial versus right-sided Maze procedures. While it is reasonable to consider concomitant atrial arrhythmia surgery in adults with Ebstein anomaly undergoing cardiac surgery, a left atrial Cox Maze III procedure should generally be avoided in the absence of documented atrial fibrillation (9,17).
Finally, over the inclusion period that spanned four decades, substantial refinements in management and surgical approaches occurred that could impact risk assessment (18), as appropriately acknowledged by the authors. Forty percent of operated patients in the present cohort had tricuspid valve repair (3). While few details are provided regarding the valve reconstruction techniques used, investigators at the Mayo Clinic have pioneered technical modifications that have been incorporated over time (11). Most recently, the cone procedure, described by da Silva and colleagues, has emerged as a more anatomical approach whereby septal leaflet mobilization allows circumferential 360° leaflet reattachment, resulting in superior leaflet-to-leaflet coaptation when compared to earlier monocuspid valve repairs (19). These considerations underscore the difficulty of risk assessment in adults with CHD who constitute a “moving target”, as they are subjected to, and benefit from, continued improvements in surgical and medical care over the years. From an arrhythmia perspective, there is some data to suggest that an aggressive diagnostic strategy that includes preoperative electrophysiological testing can contribute to lowering the risk for sudden death in patients with Ebstein anomaly undergoing the cone procedure (20).
In conclusion, Attenhofer Jost and colleagues provided much needed data in an important subgroup of patients with CHD. As the largest study of its kind, it confirms that ventricular arrhythmias and sudden death are major contributors to long-term morbidity and mortality in patients with Ebstein anomaly. The study raises important questions regarding potential proarrhythmic effects of surgical interventions and paves the way for future research addressing risk reduction strategies, including the selection of suitable candidates for primary prevention ICDs.
Acknowledgments
Dr. Khairy is supported by a research chair in electrophysiology and congenital heart disease.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tretter JT, Anderson RH. Ebstein’s or Prescher’s Anomaly? Eur Heart J 2018;39:972-3. [Crossref] [PubMed]
- Attenhofer Jost CH, Connolly HM, Dearani JA, et al. Ebstein’s anomaly. Circulation 2007;115:277-85. [Crossref] [PubMed]
- Attenhofer Jost CH, Tan NY, Hassan A, et al. Sudden death in patients with Ebstein anomaly. Eur Heart J 2018;39:1970-1977a. [Crossref] [PubMed]
- Oh JK, Holmes DR, Hayes DL, et al. Cardiac arrhythmias in patients with surgical repair of Ebstein’s anomaly. J Am Coll Cardiol 1985;6:1351-7. [Crossref] [PubMed]
- Attie F, Rosas M, Rijlaarsdam M, et al. The adult patient with Ebstein anomaly. Outcome in 72 unoperated patients. Medicine (Baltimore) 2000;79:27-36. [Crossref] [PubMed]
- Nollert G, Fischlein T, Bouterwek S, et al. Long-term survival in patients with repair of tetralogy of Fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol 1997;30:1374-83. [Crossref] [PubMed]
- Gatzoulis MA, Balaji S, Webber SA, et al. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of Fallot: a multicentre study. Lancet 2000;356:975-81. [Crossref] [PubMed]
- Khairy P, Harris L, Landzberg MJ, et al. Implantable cardioverter-defibrillators in tetralogy of Fallot. Circulation 2008;117:363-70. [Crossref] [PubMed]
- Khairy P, Van Hare GF, Balaji S, et al. PACES/HRS Expert consensus statement on the recognition and management of arrhythmias in adult congenital heart disease: developed in partnership between the Pediatric and Congenital Electrophysiology Society (PACES) and the Heart Rhythm Society (HRS). Endorsed by the governing bodies of PACES, HRS, the American College of Cardiology (ACC), the American Heart Association (AHA), the European Heart Rhythm Association (EHRA), the Canadian Heart Rhythm Society (CHRS), and the International Society for Adult Congenital Heart Disease (ISACHD). Heart Rhythm 2014;11:e102-65. [Crossref] [PubMed]
- Celermajer DS, Bull C, Till JA, et al. Ebstein’s anomaly: presentation and outcome from fetus to adult. J Am Coll Cardiol 1994;23:170-6. [Crossref] [PubMed]
- Brown ML, Dearani JA, Danielson GK, et al. The outcomes of operations for 539 patients with Ebstein anomaly. J Thorac Cardiovasc Surg 2008;135:1120-36. [Crossref] [PubMed]
- Rydman R, Shiina Y, Diller G-P, et al. Major adverse events and atrial tachycardia in Ebstein’s anomaly predicted by cardiovascular magnetic resonance. Heart 2018;104:37-44. [Crossref] [PubMed]
- Brown ML, Dearani JA, Danielson GK, et al. Effect of Operation for Ebstein Anomaly on Left Ventricular Function. Am J Cardiol 2008;102:1724-7. [Crossref] [PubMed]
- Kapusta L, Eveleigh RM, Poulino SE, et al. Ebstein’s anomaly: factors associated with death in childhood and adolescence: a multi-centre, long-term study. Eur Heart J 2007;28:2661-6. [Crossref] [PubMed]
- Celermajer DS, Cullen S, Sullivan ID, et al. Outcome in neonates with Ebstein’s anomaly. J Am Coll Cardiol 1992;19:1041-6. [Crossref] [PubMed]
- MacLellan-Tobert SG, Driscoll DJ, Mottram CD, et al. Exercise Tolerance in Patients With Ebstein’s Anomaly. J Am Coll Cardiol 1997;29:1615-22. [Crossref] [PubMed]
- Hassan A, Tan NY, Aung H, et al. Outcomes of atrial arrhythmia radiofrequency catheter ablation in patients with Ebstein’s anomaly. Europace 2018;20:535-40. [Crossref] [PubMed]
- Hetzer R, Hacke P, Javier M, et al. The long-term impact of various techniques for tricuspid repair in Ebstein’s anomaly. J Thorac Cardiovasc Surg 2015;150:1212-9. [Crossref] [PubMed]
- da Silva JP, Baumgratz JF, da Fonseca L, et al. The cone reconstruction of the tricuspid valve in Ebstein’s anomaly. The operation: early and midterm results. J Thorac Cardiovasc Surg 2007;133:215-23. [Crossref] [PubMed]
- Shivapour JK, Sherwin ED, Alexander ME, et al. Utility of preoperative electrophysiologic studies in patients with Ebstein’s anomaly undergoing the Cone procedure. Heart Rhythm 2014;11:182-6. [Crossref] [PubMed]


