
Examining EML4-ALK variants in the clinical setting: the next frontier?
The discovery of the fusion of anaplastic lymphoma kinase (ALK) with echinoderm microtubule-associated protein like 4 (EML4) and the resulting oncoprotein with a valuable clinical target has dramatically improved the survival trajectory in 4–7% of patients with non-small cell lung cancer (NSCLC) over the last decade. A phase III clinical trial (PROFILE 1007) examining previously treated patients, compared crizotinib to investigator’s choice of second-line chemotherapy for patients with ALK rearranged tumors and reported a significant improvement in objective response rate (ORR) with targeted therapy (65% vs. 20%; P<0.0001) (1). The frontline PROFILE 1014 study demonstrated crizotinib’s superiority to chemotherapy with respect to both response rates (ORR 74% vs. 45%, P<0.001) and progression-free survival (PFS) (10.9 vs. 7.0 months; P<0.001) (2). However, despite robust initial responses, more than half of the patients developed resistance to crizotinib by the end of first year. Various resistance mechanisms have been identified, including kinase domain mutations, copy number alterations, bypass tracks, paracrine signaling leading to ALK independent growth, and epithelial to mesenchymal transition (3). Newer generation ALK inhibitors such as alectinib, brigatinib, and lorlatinib have overcome some of these resistance processes and have extended the median time to progression to more than 2 years (4).
Since the initial discovery of EML4-ALK fusion protein, fifteen variants of the oncoprotein have been identified through reverse-transcriptase polymerase chain reaction (RT-PCR) or next generation sequencing (NGS). These variants are defined by the specific EML4 breakpoint that binds to the entire intracellular kinase domain of ALK (5). Variants 1, 2, 3a/b account for close to 90% of EMLA4-ALK cases. In vitro studies have demonstrated that these variants differ in their stability and sensitivity to ALK inhibitors, with variants 1 and 2 being unstable and more sensitive to ALK inhibitors and variant 3a/b being more stable with a lower sensitivity to targeted agents (6). The majority of clinical trials examining ALK inhibitors in ALK rearranged tumors did not examine the association between response rates or outcomes to specific EML4-ALK variants, perhaps missing a valuable predictive marker for response. In the phase I study which examined crizotinib in ALK-rearranged NSCLC, RT-PCR studies were done on 31 of the 82 patients, which identified variants 1, 2, 3a/b, and 9. However the patient sample size was too small to identify any correlation between the specific EML4-ALK variants and subsequent response rate (7).
Over the last couple of years, a handful of retrospective studies have reported mixed results in regards to responses to ALK inhibitors in relation to the specific ALK variant present (Table 1).
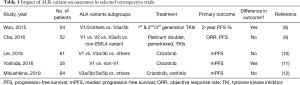
Full table
Cha et al. reported on 52 patients with ALK rearranged lung cancer and examined specific fusion variants and whether there were differences in therapeutic efficacy amongst the different variants. They did not identify differences in sensitivities of ALK inhibitors based on the ALK fusion variant (9). Similarly, Lei et al. examined 61 patients with ALK variants (grouped as variant 1, 3a/3b, and others) and noted no differences in PFS to crizotinib amongst the subgroups but did identify a weak correlation to treatment response based on the percentage of ALK-positive cells on FISH analyses (10). Conversely, Yoshida et al. in their retrospective study of 35 patients, found that there was a statistically significant difference in PFS in patients taking crizotinib with variant 1 vs. non-variant 1 ALK rearrangements (11 vs. 4.2 months; P<0.05) (11). Finally, Woo et al. divided their 54 patients in two subgroups—variants 1/2/others vs. variant 3a/3b, with about half the patients being in the latter group. The specific stratification strategy employed rested on the differential stability of the variants due to presence of the tandem atypical β-propeller in EML protein (TAPE) domain, which is absent in variants 3a/3b and 5a/5b. The 2-year PFS in patients treated with crizotinib was 76% in the variants 1/2/others and 26.4% (P=0.034) in variants 3a/3b. There was no difference in overall survival amongst the different variants. The authors postulated that this was due to an overall low mortality rate in a relatively short follow-up period and an imbalance of more heavily pretreated patients in the in the variant 1/2/others group (8).
More recently, Christopoulos and his colleagues published their data on the effect of specific ALK variants and clinical outcomes. They examined all of their stage IV lung cancer patients with EML4-ALK fusion variants 1, 2, and 3a/3b by NGS or RT-PCR. In this larger retrospective study of 67 patients with a longer follow-up, they conclude that the V3 (3a/3b) variant is associated with more typical and atypical metastatic sites at diagnosis, earlier failure after treatment with first or second line ALK inhibitors, platinum-based chemotherapy, and cerebral radiotherapy, and finally, an inferior overall survival (13). Though some of these conclusions were reported in the earlier mentioned retrospective studies, there were unique strengths in their study design that highlight the importance of this additional study.
Christopoulos et al. defined the time to treatment failure by two different methods—traditional progression according to RECIST criteria and by time to next treatment which takes into account the common practice of continuing targeted therapy beyond progression after local ablative therapy for oligoprogressive disease. Recognition of the latter situation is important as this strategy been shown in small, single institution studies to improve overall survival and allow patients to continue on the same targeted therapy for up to a year beyond initial diagnosis of extracranial progression (14). Follow-up for this study was also longer at 29 months, perhaps accounting for the statistical difference in overall survival for the fusion variant 3a/3b. Patients with variant 3a/3b had a shorter PFS after treatment with first- or second-generation tyrosine kinase inhibitor (TKI) (7.3 vs. 39.3 months and 5.0 vs. 11.2 months respectively) as well as after first-line treatment with platinum-based chemotherapy (5.4 vs. 15.2 months). This difference in outcomes for the variant 3a/3b group retained statistical significance when using the alternative method of defining time to treatment failure as the time to next treatment. Interestingly, patients with variant 3a/3b also had a shorter brain PFS (6.1 months vs. not reached), an observation that had not been specifically reported in prior studies. Finally, the median overall survival for variant 3a/3b was 39.8 vs. 59.6 months for V1/V2 patients (13).
Despite the strengths of longer follow-up and a study design more accurately representing the common clinical practice of continuing TKIs after local therapy for oligoprogressive disease, we must be wary of making broad generalizations e that variant 3a/3b of the EML-ALK translocation portends a shorter PFS in patients treated with crizotinib, and perhaps even an inferior survival. With more than 15 different variants already identified, presently published studies do not represent the less common variants which are typically lumped into an “other” group. Furthermore, there is heterogeneity in how each study divided their subgroups, making it difficult to validate these results, some of which are contradictory to each other.
These retrospective data highlight that we must reconsider our ALK rearrangement detection methods. At present, the only two FDA approved methods for detecting EML4-ALK rearrangements are through fluorescence in situ hybridization (FISH) and a standalone immunohistochemistry (IHC) stain [ALK (D5F3) CDx Assay]. While FISH has become the gold standard of ALK mutation detection in the United States, break apart assays fail to pinpoint novel variants, thereby missing valuable opportunities to discover new predictive and prognostic biomarkers. NGS has the ability to quickly and reliably identify ALK rearranged lung cancers and the specific variants involved. Additionally, this method has the ability to isolate resistance mutations that often emerge at disease progression, allowing for a switch to a more effective targeted therapy. Identifying these accompanying genetic alterations may shed light on whether certain ALK variants are associated with the development of specific resistance mutations. However, there are pitfalls to NGS testing—for one, most biopsy specimens are placed formalin fixed paraffin embedded (FPPE) tissues and the ability to extract a sufficient amount of RNA needed for NGS can be variable (15). Therefore, it is unknown if NGS should serve as a companion test to FISH and IHC and the economic impact of such a strategy.
In conclusion, Christopoulos and his colleagues have added another study that adds to the mounting data that the presence specific ALK variants may influence clinical outcomes and potentially serve as predictive biomarkers. The authors should be commended for their study design, but we must be cognizant of the limitations of retrospective analysis. These studies are small and it is premature to alter clinical practice based on the present data. It is insufficient to interpret specific ALK variants on their own. They must be studied in concordance with the accompanying genetic changes to get a more complete picture of the basis for differences in clinical outcome. As we design trials that incorporate more potent, newer generation ALK inhibitors in the first line setting or the use chemotherapy and checkpoint blockade in oncogene driven lung cancers, moving forward, we must study the impact of ALK variants prospectively. Therapeutic strategies that could be adopted for more aggressive variants remains unknown and will likely emerge as a future research question.
Acknowledgements
None.
Footnote
Conflicts of Interest: SK Jabbour has received research funding for Merck and Nestle. J Malhotra is on the advisory board of Astra-Zeneca and Pfizer and has received research funding from Oncoceutics. M Patel has no conflicts of interest to declare.
References
- Shaw AT, Kim DW, Nakagawa K, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med 2013;368:2385-94. Erratum in: Crizotinib versus Chemotherapy in Advanced ALK-Positive Lung Cancer. [N Engl J Med 2015]. [Crossref] [PubMed]
- Solomon BJ, Mok T, Kim DW, et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med 2014;371:2167-77. Erratum in: First-Line Crizotinib versus Chemotherapy in ALK-Positive Lung Cancer. [N Engl J Med 2015]. [Crossref] [PubMed]
- Dagogo-Jack I, Shaw AT. Crizotinib resistance: implications for therapeutic strategies. Ann Oncol 2016;27 Suppl 3:iii42-iii50. [Crossref] [PubMed]
- Peters S, Camidge DR, Shaw AT, et al. Alectinib versus Crizotinib in Untreated ALK-Positive Non-Small-Cell Lung Cancer. N Engl J Med 2017;377:829-38. [Crossref] [PubMed]
- Sabir SR, Yeoh S, Jackson G, et al. EML4-ALK Variants: Biological and Molecular Properties, and the Implications for Patients. Cancers (Basel) 2017;9. [Crossref] [PubMed]
- Heuckmann JM, Balke-Want H, Malchers F, et al. Differential protein stability and ALK inhibitor sensitivity of EML4-ALK fusion variants. Clin Cancer Res 2012;18:4682-90. [Crossref] [PubMed]
- Kwak EL, Bang YJ, Camidge DR, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med 2010;363:1693-703. [Crossref] [PubMed]
- Woo CG, Seo S, Kim SW, et al. Differential protein stability and clinical responses of EML4-ALK fusion variants to various ALK inhibitors in advanced ALK-rearranged non-small cell lung cancer. Ann Oncol 2017;28:791-7. [PubMed]
- Cha YJ, Kim HR, Shim HS. Clinical outcomes in ALK-rearranged lung adenocarcinomas according to ALK fusion variants. J Transl Med 2016;14:296. [Crossref] [PubMed]
- Lei YY, Yang JJ, Zhang XC, et al. Anaplastic Lymphoma Kinase Variants and the Percentage of ALK-Positive Tumor Cells and the Efficacy of Crizotinib in Advanced NSCLC. Clin Lung Cancer 2016;17:223-31. [Crossref] [PubMed]
- Yoshida T, Oya Y, Tanaka K, et al. Differential Crizotinib Response Duration Among ALK Fusion Variants in ALK-Positive Non-Small-Cell Lung Cancer. J Clin Oncol 2016;34:3383-9. [Crossref] [PubMed]
- Mitiushkina NV, Tiurin VI, Iyevleva AG, et al. Variability in lung cancer response to ALK inhibitors cannot be explained by the diversity of ALK fusion variants. Biochimie 2018;154:19-24. [Crossref] [PubMed]
- Christopoulos P, Endris V, Bozorgmehr F, et al. EML4-ALK fusion variant V3 is a high-risk feature conferring accelerated metastatic spread, early treatment failure and worse overall survival in ALK+ non-small cell lung cancer. Int J Cancer 2018;142:2589-98. [Crossref] [PubMed]
- Gan GN, Weickhardt AJ, Scheier B, et al. Stereotactic radiation therapy can safely and durably control sites of extra-central nervous system oligoprogressive disease in anaplastic lymphoma kinase-positive lung cancer patients receiving crizotinib. Int J Radiat Oncol Biol Phys 2014;88:892-8. [Crossref] [PubMed]
- Hofman P. ALK in Non-Small Cell Lung Cancer (NSCLC) Pathobiology, Epidemiology, Detection from Tumor Tissue and Algorithm Diagnosis in a Daily Practice. Cancers (Basel) 2017.9. [PubMed]


