
Drug eluting stents versus bare metal stents for the treatment of saphenous vein grafts failure: learnings from the DIVA trial
We read with great interest the DIVA (Drug eluting stent versus bare metal stent in saphenous vein graft angioplasty) trial by Brilakis and colleagues (1) that was designed to answer a remaining controversial question on the choice of the optimal stent type for the treatment of saphenous vein grafts (SVG) failure. This trial was undertaken by leading investigators in percutaneous coronary implantation (PCI) who compared the efficacy of drug-eluting stent (DES) with bare-metal stents (BMS) for the treatment of de novo SVG stenosis. SVG failure following coronary artery bypass graft (CABG) surgery is a common finding with a reported rate ranging from 25 to over 50% within 10 years (2). It is a serious clinical issue and repeat CABG for SVG occlusion is associated with poor outcomes (3). Therefore, PCI represents the preferred treatment option when native coronary PCI is not feasible and represents 6% of all PCIs in the United States (3,4). Nevertheless, SVG PCIs are at risk of higher complications and worse outcome compared to native coronary artery intervention (5). While evidence of the superiority of DES over BMS is well demonstrated in native coronary artery PCI, conflicting data are available on the optimal stent to use in SVG failure.
Before the DIVA trial, four randomized trials designed to assess the efficacy of DES over BMS in SVG failure were conducted [RRISC (6), SOS (7), ISAR-CABG (8) and BASKET-SAVAGE (9) trials] and all showed the superiority of DES over BMS in reducing the primary endpoint at 6 or 12 months (Table 1). Because of their various sizes, substantial limitations and controversial data at long term follow-up, results from these trials could not be extrapolated. In that context, the results of the DIVA trial were widely expected. The DIVA trial was a double-blind, randomized controlled trial conducted in 25 American departments of Veterans affairs centers. Among 3,482 screened patients, 597 (17%) patients met eligibility criteria [patients aged at least 18 years, with at least one significant de-novo SVG lesion (50–99% stenosis of a 2.25–4.5 mm diameter SVG) requiring PCI with intent to use embolic protection devices, and agreed to participate and take medication as prescribed]. They were randomly assigned to either DES (n=292) or BMS (n=305). The primary endpoint was a 12-month incidence of target vessel failure (TVF) defined as a composite of cardiac death, target vessel myocardial infarction or target vessel revascularization (TVR). The DIVA trial showed no difference between DES and BMS on the primary endpoint at 12 months which occurred in 17% of the patients assigned to DES vs. 19% of the patients from the BMS group (adjusted hazard ratio 0.92; 95% CI, 0.63–1.34, P=0.70). In both groups, TVF was mainly driven by TVR (12% in the DES group vs. 11% in the BMS group). In addition, no difference was found among all individual endpoints of the composite primary endpoint.
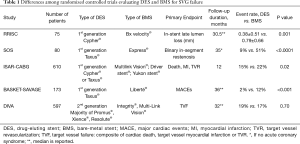
Full table
This is the first trial that failed to show the superiority of DES over BMS at 12 months follow-up. Nevertheless, these results do not deliver a completely new message. They are consistent with long-term results of previous trials which found a loss of superiority of DES over BMS at long term follow-up (i.e., 3-year follow-up of the RRISC trial (10) and 5-year follow-up of the ISAR-CABG trial (11). In contrast, other studies with long-term follow-up such as SOS or BASKET-SAVAGE, which used only first-generation paclitaxel-eluting stents, showed a sustained benefit. If large randomized trials have confirmed that DES were associated with a lower risk of restenosis as compared with BMS for native coronary arteries, these results mainly highlight that SVG disease does not have the exact same pathophysiology than native coronary artery disease (CAD) and portends a higher risk of complications (12). Indeed, histological findings showed that SVG atherosclerotic lesions are usually concentric, with diffuse foam cells present on the luminal surface in early disease and a larger number of foam cells and extracellular lipids in the intima in advanced disease. In addition, these lesions often present an inflammatory infiltrate in the intima, consisting of lymphocytes, plasma cells and macrophages, which sometimes infiltrate the medial and adventitial layers. Therefore, the SVG plaques are fragile with no fibrous cap to prevent the lesion components from contact with the blood stream. These lesions differ substantially from those of native coronary atherosclerotic lesions, which are usually eccentric, have a fibrous cap and fewer inflammatory cells (13). In addition, because of this heavy atherosclerotic burden in SVG and the frequent distal embolization of friable material during PCI, both short and long-term results of SVG PCI cannot be reproduced as compared to native coronary artery PCI. Nevertheless, these differences cannot solely explain the differences between the results of the DIVA trial as compared to previous trials.
First, the main difference of the DIVA trial with previous trials was the quasi systematic use of contemporary secondary generation DES whereas first generation stents eluting paclitaxel and sirolimus were implanted in the other trials (i.e., Cypher (sirolimus-eluting stent) in the RRISC trial, Taxus (paclitaxel-eluting stent) in the SOS and the BASKET-SAVAGE trials and either Cypher or Taxus in the ISAR-CABG trial). Given the different pathophysiological perspective between SVG disease and native CAD, the pharmacological effect of the different drugs on the vessel wall might also be different in SVG and in native coronary arteries. Jeger et al. hypothesized that the specific effect of the drugs used in first-generation DES, particularly paclitaxel, might lead to an adequate treatment effect in SVG, whereas the smaller amount of smooth muscle cells in the walls of SVG, compared with native coronary arteries, might not necessitate drugs as effective as in second-generation DES (14). However, safety of primary stent generation is also unproven as higher events were found in the DES group in the long-term follow-up of the RRISC and ISAR-CABG trials. In addition, a recent meta-analysis of specific trials which compared the efficacy of first versus second-generation DES found a superiority of second-generation DES in the treatment of SVG failure (15). One other hypothesis to explain the lack of difference between DES and BMS in the DIVA trial is the use of more recent BMS with thinner platforms that could have reconciled differences between BMS and DES.
Second, the secondary prevention of the atherosclerostic disease progression has become more aggressive in the last decade with the emergence of more powerful antiplatelet and statin therapy. This might also mitigate differences between DES and BMS in such small sample size trials. Comparison of dual antiplatelet therapy duration, the use of statins and low-density lipoprotein cholesterol levels could have also been informative. Unfortunately, such data were not consistently reported in all trials. Indeed, even if recent small-sized randomized controlled trial (16) showed no difference in vein graft occlusion 1 year after CABG between high and low-dose atorvastatin, meta-analysis demonstrated that compared with moderate statin therapy, long-term aggressive statin further decreased the atherosclerotic progression of SVG, and reduced the risks of repeated myocardial infarction and coronary revascularization after CABG (17). Therefore, as low-density lipoprotein cholesterol objectives have varied during the timeframes of the DIVA and previous trials, this parameter might have mitigated these results. In addition, looking at patient characteristics, the ISAR-CABG trial, enrolled fewer diabetics (36% vs. 60%), fewer hypertensive (72% vs. 96%), fewer current smokers (7% vs. 22.5%), more stable angina patients (61% vs. 32%), and lower body mass index patients (27.5 vs. 30.6), as compared with the DIVA trial. The over-representation of diabetic patients in the DIVA trial (59% vs. 46% in BASKET-SAVAGE, 16% in RRISC, 44% in SOS, and 37% in ISAR-CABG) could have impacted the results. Because of differences in anatomical vascular wall constitution, the superiority of DES over BMS in SVG failure in diabetic patients may not be as strong as it is in native coronary artery lesion. Nevertheless, it is unclear whether such differences in patient demographics could have an effect on the comparison and the examined outcomes.
Third, we can hypothesize that the systematic intent to use of embolic protection device (level class I in American Heart Association guidelines) (18) that was specifically mentioned in the eligibility criteria unlike in the other trials could have influenced outcomes by reducing events. Nevertheless, we observed that embolic protection device was not systematically used in the DIVA trial, 69% of the procedures (same rate as in the RRISC trial). As the use of embolic devices was extremely variable in the different trials (<5% in the ISAR-CABG, 80% in the RRISC trial), we can scarcely conclude on the impact of embolic devices on the results of the DIVA trial. Moreover, the systematic use of such a device in SVG PCI was recently debated in the light of a recent meta-analysis that showed no benefice of routine use of embolic device during SVG PCI (19).
Fourth, the DIVA trial reported an impressively high rate of TVF at a median follow-up of 2.7 years (i.e., 34% with BMS vs. 37% in DES) and might just highlight the aggressive nature of SVG disease and the overall worse outcomes compared to native vessel CAD. This highlights the importance to perform native coronary artery PCI whenever feasible, rather than SVG PCI (20).
Based on these discrepancies among results, using different stents types, at different timeframes with probably different medical therapies, and with such small cohorts as compared to stent trials sizes that demonstrated benefit of DES over BMS in native coronary arteries, it is therefore difficult to draw definitive conclusions. Indeed, we could hypothesize that the ideal stent type for SVG disease could be different from the one used for native vessel disease given the different nature of SVG disease pathophysiology. Nevertheless, large-scale, well-conducted, randomized trials are unlikely to be performed given the difficulty to recruit patients in the last largest randomized controlled trials.
Therefore, how should SVG failure be treated? Efforts should be put to treat native coronary artery and be preferred to treating the bypass graft lesion, as it is likely to provide better long-term patency rates (21). However, such procedures can sometimes be complex, with old chronic total occlusions, involving bifurcations and calcified vessels requiring expertise in the treatment of these lesions. Nevertheless, this should not be a drawback to their treatment but should rather encourage cardiologists to refer these patients to experienced operators or chronic total occlusions specialists. Redo CABG surgery should be avoided as it carries high complication risk, especially in patients with patent internal thoracic artery graft. In the end, if PCI of the bypass graft has to be performed, the choice between BMS and DES are likely to be based on economical decision as there is no clear benefit of DES compared to BMS, suggesting that the lower cost BMS can be used in SVG lesions without compromising either safety or efficacy. These decisions might differ between countries, depending on local stent pricing. In all cases, prolonged dual antiplatelet therapy if possible, and intensive statin therapy or other lipid-lowering drugs should be used to reduce the risk of recurrent events (22).
Acknowledgements
None.
Footnote
Conflicts of Interest: F Picard reports consulting fees and speaker fees from Biotronik. The other authors report no conflicts of interest.
References
- Brilakis ES, Edson R, Bhatt DL, et al. Drug-eluting stents versus bare-metal stents in saphenous vein grafts: a double-blind, randomised trial. Lancet 2018;391:1997-2007. [Crossref] [PubMed]
- Goldman S, Zadina K, Moritz T, et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: Results from a Department of Veterans Affairs Cooperative Study. J Am Coll Cardiol 2004;44:2149-56. [Crossref] [PubMed]
- Brilakis ES, Rao SV, Banerjee S, et al. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc Interv 2011;4:844-50. [Crossref] [PubMed]
- Dehmer GJ, Weaver D, Roe MT, et al. A contemporary view of diagnostic cardiac catheterization and percutaneous coronary intervention in the United States: a report from the CathPCI Registry of the National Cardiovascular Data Registry, 2010 through June 2011. J Am Coll Cardiol 2012;60:2017-31. [Crossref] [PubMed]
- Redfors B, Généreux P, Witzenbichler B, et al. Percutaneous Coronary Intervention of Saphenous Vein Graft. Circ Cardiovasc Interv 2017.10. [PubMed]
- Vermeersch P, Agostoni P, Verheye S, et al. Randomized Double-Blind Comparison of Sirolimus-Eluting Stent Versus Bare-Metal Stent Implantation in Diseased Saphenous Vein Grafts: Six-Month Angiographic, Intravascular Ultrasound, and Clinical Follow-Up of the RRISC Trial. J Am Coll Cardiol 2006;48:2423-31. [Crossref] [PubMed]
- Brilakis ES, Lichtenwalter C, de Lemos JA, et al. A Randomized Controlled Trial of a Paclitaxel-Eluting Stent Versus a Similar Bare-Metal Stent in Saphenous Vein Graft Lesions: The SOS (Stenting Of Saphenous Vein Grafts) Trial. J Am Coll Cardiol 2009;53:919-28. [Crossref] [PubMed]
- Mehilli J, Pache J, Abdel-Wahab M, et al. Drug-eluting versus bare-metal stents in saphenous vein graft lesions (ISAR-CABG): a randomised controlled superiority trial. Lancet 2011;378:1071-8. [Crossref] [PubMed]
- Jeger R. Study to test the efficacy and safety of drug eluting versus bare-metal stents for saphenous vein graft interventions (BASKET-SAVAGE). Eur Soc Cardiol Meet. 2016 Aug 27 [cited 2018 Nov 11]; Available online: https://www.escardio.org/The-ESC/Press-Office/Press-releases/basket-savage-trial-drug-eluting-stents-more-benefit-in-saphenous-vein-grafts
- Vermeersch P, Agostoni P, Verheye S, et al. Increased Late Mortality After Sirolimus-Eluting Stents Versus Bare-Metal Stents in Diseased Saphenous Vein Grafts: Results From the Randomized DELAYED RRISC Trial. J Am Coll Cardiol 2007;50:261-7. [Crossref] [PubMed]
- Colleran R, Kufner S, Mehilli J, et al. Efficacy Over Time With Drug-Eluting Stents in Saphenous Vein Graft Lesions. J Am Coll Cardiol 2018;71:1973-82. [Crossref] [PubMed]
- de Vries MR, Simons KH, Jukema JW, et al. Vein graft failure: from pathophysiology to clinical outcomes. Nat Rev Cardiol 2016;13:451-70. [Crossref] [PubMed]
- Sarjeant JM, Rabinovitch M. Understanding and treating vein graft atherosclerosis. Cardiovasc Pathol 2002;11:263-71. [Crossref] [PubMed]
- Jeger RV, Möbius-Winkler S. Stents in saphenous vein grafts. Lancet 2018;391:1967-8. [Crossref] [PubMed]
- Shi HT, Chu HX, Gu W, et al. Second-generation versus first-generation drug-eluting stents in saphenous vein graftdisease: A meta-analysis of randomized controlled trials. Int J Cardiol 2016;214:393-7. [Crossref] [PubMed]
- Kulik A, Abreu AM, Boronat V, et al. Intensive versus moderate statin therapy and early graft occlusion after coronary bypass surgery: The Aggressive Cholesterol Therapy to Inhibit Vein Graft Events randomized clinical trial. J Thorac Cardiovasc Surg 2019;157:151-61.e1. [Crossref] [PubMed]
- Kang S, Liu Y, Liu X. Effects of aggressive statin therapy on patients with coronary saphenous vein bypass grafts: a systematic review and meta-analysis of randomized, controlled trials. Clin Ther 2013;35:1125-36. [Crossref] [PubMed]
- Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574-651. [PubMed]
- Paul TK, Bhatheja S, Panchal HB, et al. Outcomes of Saphenous Vein Graft Intervention With and Without Embolic Protection Device: A Comprehensive Review and Meta-Analysis. Circ Cardiovasc Interv 2017.10. [PubMed]
- Brilakis ES, O’Donnell CI, Penny W, et al. Percutaneous Coronary Intervention in Native Coronary Arteries Versus Bypass Grafts in Patients With Prior Coronary Artery Bypass Graft Surgery: Insights From the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. JACC Cardiovasc Interv 2016;9:884-93. [Crossref] [PubMed]
- Mavroudis CA, Kotecha T, Chehab O, et al. Superior long term outcome associated with native vessel versus graft vessel PCI following secondary PCI in patients with prior CABG. Int J Cardiol 2017;228:563-9. [Crossref] [PubMed]
- Sousa-Uva M, Neumann FJ, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur J Cardiothorac Surg 2019;55:4-90. [Crossref] [PubMed]


