
Review of different approaches of the left recurrent laryngeal nerve area for lymphadenectomy during minimally invasive esophagectomy
Introduction
For completing the total mediastinal lymphadenectomy, doing the left recurrent laryngeal nerve (LRLN) lymph node resection forms an important part of the intervention (1). Because of the location and the risks of damage to the nerve, this part of the procedure can be challenging (2). Note that the lymph nodes are numbered as 4 L and 2 L and in the Japanese classifications as 106recL and 106tbL (3,4).
Anatomically, the LRLN branches from the left vagal nerve, recurs around the aorta arch, and ascends into de groove between the trachea and the esophagus in the direction to the left vocal cord. Aim of the operation is to resect the located lymph nodes—posterior as well as anterior—and doing so without any harm to the nerve. In some cases, growth of the tumor or affected LN in the nerve will imply its partial resection.
The thoracoscopic approach for esophageal resection and lymphadenectomy is increasingly used because of perfect visualization and its postoperative advantages; these boons are the reduction of morbidity and increase of the quality of life without compromising the oncological safety of the operation (5,6).
Methods
Search strategy
A literature search is made using the PubMed about how to approach the left recurrent laryngeal nerve lymphadenectomy by minimally invasive esophagectomy.
Surgical approaches
Thoracoscopy can be performed in lateral or in prone position (7,8). In both positions all LRLN approaches are available (9,10). In carrying out some it seems that the proximal esophagus can be an obstacle to properly visualize the area. Therefore, some tricks are used in order to improve the visualization. These concern the position of the patient by the semi-prone position (11) or by division or retraction of the esophagus and some rotation of the trachea once the mobilization of the esophagus has been completed before starting the LRLN lymphadenectomy.
Five approaches to accomplish this lymphadenectomy of the LRLN are described and commented on.
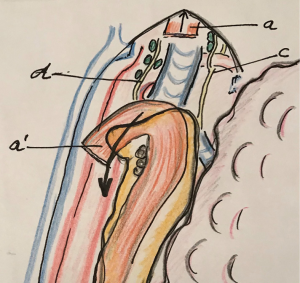
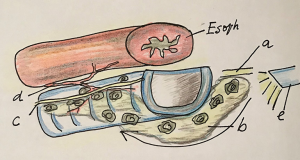
After section of the proximal esophagus at the upper mediastinum
Once that the esophagus is dissected free up to the thoracic apex, the esophagus is divided at the upper mediastinum, proximal of the tumor by means of a stapler. Japanese surgeons have described two methods after esophageal division in order to visualize the left upper mediastinum: the “stripping method” and the “bascule method”. In the first method, the proximal esophagus (and the nasogastric tube) once divided, is stripped by pulling the nasogastric tube in the reverse direction and retracted toward the neck (Figure 1) (12,13). In the second method, the proximal esophagus is kept attached to the left upper mediastinum and after division the tissue including the LRLN and lymph nodes remain attached to the proximal part of the esophagus. This proximal esophagus and tissues are drawn through a gap between the vertebral body and the scapula obtaining an optimal operative field for the lymphadenectomy. Using this traction, a two-dimensional membrane is easily recognizable and dissection of the lymph nodes from the LRLN should be easy (14). In both methods, retraction of the divided proximal esophagus will create an optimal view of the LRLN area.
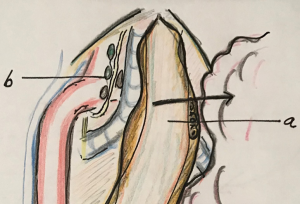
After complete mobilization of the esophagus and its retraction
In this approach the proximal esophagus is not divided after complete mobilization but retracted to the right side in order to visualize the left paratracheal groove. To accomplish this retraction there are two different ways: the standard lateral retraction of the esophagus to the right by means of an instrument (Figure 2); and the “suspension method” in which a traction loop is used, internally or externally, to suspend the proximal esophagus. In this way tissues and lymph node around the LRLN are tented helping to improve the exposure and the lymphadenectomy (15,16).
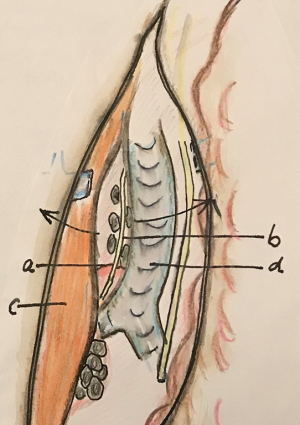
Dissection between trachea and esophagus. Leaving the esophagus attached laterally
After the lymphadenectomy of the right recurrent laryngeal nerve (RRLN), the proximal esophagus is mobilized on its right and anterior side and then the space between the trachea and the esophagus is dissected free thereby making an ample window. Through this window the LRLN area can be approached and consequently the lymphadenectomy is performed (Figure 3). Osugi et al., use this approach in thoracoscopy in lateral position to perform the LRLN lymphadenectomy. Lin et al., perform the so-called “looping method” in which the traction of the esophagus is done by an external loop around the esophagus (Figure 4) (17,18).
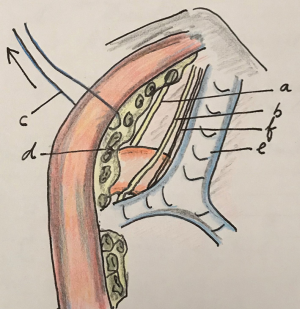
Pretracheal dissection of the LN up to the LRLN area
After starting, in prone position, the lymphadenectomy of the right side between the right vagal nerve and the trachea, the lymphadenectomy can be continued “en bloc” along the anterior wall of the trachea up to the area of the LRLN (Figure 5) (10).
By transcervical mediastinoscopy
Fujiwara et al., perform the esophageal resection by transcervical incision under a mediastinoscope to dissect completely the esophagus and corresponding lymph node stations. After exposure of the LRLN, surrounding lymph nodes are resected keeping the nodes attached to the esophagus (19).
Most surgeons use the thoracoscopy in semiprone or prone position to perform this LRLN lymphadenectomy, but others use the lateral decubitus position (17). Finally, a hybrid form of thoracoscopy is performed by Kaburagi et al., they use for the lymphadenectomy of the upper part the lateral approach and for the middle and distal part of the mediastinum the thoracoscopy in prone position (20).
All the procedures, here described, can be also be performed by robot assisted minimally invasive esophagectomy (RAMIE) (21).
Discussion
Lymphadenectomy of the supracarinal lymph nodes by thoracoscopic esophagectomy is an important part of the total mediastinal lymphadenectomy. Especially on the left side, the lymphadenectomy of the groups 2 L and 4 L, along the LRLN nerve can be challenging. It can be difficult because the need for optimal visualization of the area and the need for a gentle dissection in order to avoid trauma of the nerve.
We have treated five different ways for upper mediastinal dissection especially of the left recurrent laryngeal nerve area, each one with pros and cons. Until now, no evidence is available for determining which approach is preferred. At the same time, regarding the different approaches of performing the thoracoscopy—whether the lateral or the prone positions—literature indicates some advantages of the prone position such as less pulmonary complications, less blood loss and more mediastinal lymph node harvest (22). In order to obtain an optimal visualization, other authors have suggested important advantages using the semiprone position for performing the lymphadenectomy of this difficult area (11). In the West, esophageal surgeons, probably less experienced with this upper mediastinal lymphadenectomy, think that the visualization in prone position may be optimal for this area.
Probably these differences of concept are attributable to the position of the trocars during thoracoscopy in prone position. In the West the trocars are placed between the scapula and the spine whereas in the East surgeons accustomed to put the trocars on lateral of the scapula (5,11). Important point of discussion is the use of an electric device to stimulate the vagal nerve for monitoring the LRLN during this lymphadenectomy (23). More evidence about this technique is needed.
It is clear that more standardization on how to perform this important lymphadenectomy is necessary with gaining optimal dissection and low damage to the recurrent nerve.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Bumm R, Wang J. More or less surgery for esophageal cancer: extent of lymphadenectomy for squamous cell esophageal carcinoma-How much is necessary? Dis Esophagus 1994;7:151-5. [Crossref]
- Fujita H, Kakegawa T, Yamana H, et al. Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 1996;222:654-62. [PubMed]
- Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997;111:1718-23. [Crossref] [PubMed]
- Japan Society for Esophageal Diseases (JSED). Guidelines for Clinical and Pathologic Studies on Carcinoma of the Esophagus, 9th ed. Kanehara & Co, Ltd., Tokyo, 2008.
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Straatman J, van der Wielen N, Cuesta MA, et al. Minimally Invasive versus Open esophageal resection: Three-year follow up of the previously reported randomized control trial: the TIME trial. Ann Surg 2017;266:232-6. [Crossref] [PubMed]
- Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al. Minimally invasive esophagectomy: outcomes in 222 patients. Ann Surg 2003;238:486-94. [PubMed]
- Palanivelu C, Prakash A, Senthilkumar R, et al. Minimally Invasive Esophagectomy: thoracoscopic mobilization of the esophagus and mediastinal lymphadenectomy in prone position: experience of 130 patients. J Am Coll Surg 2006;203:7-16. [Crossref] [PubMed]
- Noshiro H, Iwasaki H, Kobayashi K, et al. Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc 2010;24:2965-73. [Crossref] [PubMed]
- Cuesta MA, van der Wielen N, Weijs TJ, et al. Surgical anatomy of the supracarinal esophagus based on a minimally invasive approach: vascular and nervous anatomy and technical steps to resection and lymphadenectomy. Surg Endosc 2017;31:1863-70. [Crossref] [PubMed]
- Kawakubo H, Takeuchi H, Kitagawa Y. Current status and future perspectives on Minimally Invasive Esophagectomy. Korean J Thorac Cardiovasc Surg 2013;46:241-8. [Crossref] [PubMed]
- Makino H, Nomura T, Miyashita M, et al. Esophageal stripping creates a clear operative field for lymph node dissection along the left recurrent laryngeal nerve in prone video-assisted thoracoscopic surgery. J Nippon Med Sch 2011;78:199-204. [Crossref] [PubMed]
- Makino H, Yoshida H, Maruyama H, et al. An original technique for lymph node dissection along the left recurrent laryngeal nerve after stripping the residual esophagus during video-assisted thoracoscopic surgery of esophagus. J Vis Surg 2016;2:166. [Crossref] [PubMed]
- Oshikiri T, Yasuda T, Harada H, et al. A new method (the “Bascule method”) for lymphadenectomy along the left recurrent laryngeal nerve during prone esophagectomy for esophageal cancer. Surg Endosc 2015;29:2442-50. [Crossref] [PubMed]
- Xi Y, Ma Z, Shen Y, et al. A novel method for lymphadenectomy along the left laryngeal recurrent nerve during thoracoscopic esophagectomy for esophageal carcinoma. J Thorac Dis 2016;8:24-30. [PubMed]
- Zheng W, Zhu Y, Guo CH, et al. Esophageal suspension method in scavenging peripheral lymph nodes of the left recurrent laryngeal nerve in thoracic esophageal carcinoma through semi-prone-position thoracoscopy. J Cancer Res Ther 2014;10:985-90. [Crossref] [PubMed]
- Osugi H, Narumiya K, Kudou K. Supracarinal dissection of the esophagus and lymphadenectomy by MIE. J Thorac Dis 2017;9:S741-50. [Crossref] [PubMed]
- Lin M, Shen Y, Feng M, et al. Minimally invasive esophagectomy: Chinese experiences. J Vis Surg 2016;2:134. [Crossref] [PubMed]
- Fujiwara H, Shiozaki A, Konishi H, et al. Mediastinoscope and laparoscope-assisted esophagectomy. J Vis Surg 2016;2:125. [Crossref] [PubMed]
- Kaburagi T, Takeuchi H, Kawakubo H, et al. Clinical utility of a novel hybrid position combining the left lateral decubitus and prone positions during thoracoscopic esophagectomy. World J Surg 2014;38:410-8. [Crossref] [PubMed]
- Suda K, Kawamura Y, Inaba K, et al. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg 2012;36:1608-16. [Crossref] [PubMed]
- Markar SR, Wiggins T, Antonowicz S, et al. Minimally invasive esophagectomy: Lateral decubitus vs. prone positioning; systematic review and pooled analysis. Surg Oncol 2015;24:212-9. [Crossref] [PubMed]
- Wong I, Tong DKH, Tsang RKY, et al. Continuous intraoperative vagus nerve stimulation for monitoring of recurrent laryngeal nerve during minimally invasive esophagectomy. J Vis Surg 2017;3:9. [Crossref] [PubMed]


