The use of an online pictorial Epworth Sleepiness Scale in the assessment of age and gender specific differences in excessive daytime sleepiness
Introduction
Conditions associated with excessive daytime sleepiness (EDS) are multi-factorial, but sleep disorders are highly prevalent amongst patients with EDS (1,2). The occurrence of isolated EDS in the general population is estimated to be between 2.5% and 18%, depending on the quantification method used (3-6). However, when co-morbidity is present debilitating sleepiness may be more common and the impact on public health becomes significant (7,8).
It is difficult to assess subjective EDS accurately because symptoms may differ significantly from objective measures of sleepiness (9,10). The most widely used self-administered questionnaire, developed for obstructive sleep apnoea (OSA), is the Epworth Sleepiness Scale (ESS). It has also been used in patients with other sleep disorders and has been translated and validated in several languages (11-17).
Recently, a pictorial version of the ESS (pESS) has been developed in the United Kingdom and was validated against the traditional ESS; the pictorial version produces scores comparable to the traditional ESS but is similarly useful to those with and without diminished literacy. Furthermore, pictures were shown to be more helpful to patients compared to words. It was reported that the pESS was easy and more frequently preferred compared to the conventional ESS (18).
By using the pictorial ESS we sought to determine the level of EDS in the general population. We hypothesised that the use of an online version of the pictorial ESS would enable us to study gender and age specific differences in EDS on a large scale.
Patients and methods
This study was a collaborative project between the British Lung Foundation (BLF), King’s Health Partners at Guy’s and St Thomas’ NHS Hospital Foundation Trust and King’s College London. Interested subjects accessed the BLF webpage where an English version of the pESS had been displayed as part of their campaign to raise awareness of OSA in the United Kingdom. Following a short explanation and the recording of self-reported age (lifetime decade) and gender (male/female) the eight domains of the pESS were filled in, followed by an analysis and explanations. In accordance with the traditional ESS, a cut-off of >10 points was used to define EDS (11,17).
Data acquisition started in March 2012 and ended in October 2012; the final scores and those of each item score were recorded and compared to previous data using the pictorial ESS and the traditional ESS (17,18). The impact of gender and age on total and item scores was also explored. Based on indicated age subjects were categorized into lifetime decades with the exceptions of ages 0-19 years and above 80 years, which were combined into one age category respectively.
Statistical analysis
Statistical analysis of the data was performed using SPSS (Version17.0, SPSS Inc, Chicago/IL, USA). Data are reported as mean (standard deviation, SD), if not otherwise indicated. Following testing for normality, means were compared using Student’s t-test and Chi-square statistics; Mann Whitney rank sum test (two-tailed) was used if data were non-normally distributed. Comparisons between age groups and pictorial ESS scores of different questions were made using one-way ANOVA and post-hoc test using the least significant difference (LSD) or Kruskal-Wallis test if there was a non-Gaussian distribution. The P value for trend (P trend) between age and sleepiness was calculated using simple and multiple linear regression analysis to further describe age and gender interaction. We considered a P<0.05 to be statistically significant (19).
Results
Within the group of 8,098 subjects, there was a statistically significant association between sleepiness and age (P<0.001, Figure 1A). In this group, 49% (3,946) of subjects were male and they tended to score higher [10.2 (5.4) points] than female subjects [9.8 (5.0) points, P=0.007]; in the group of the excessively sleepy subjects the score was higher if the subject was male [15.1 (3.4) vs. 14.6 (3.1) points, P<0.001]. Overall 44.3% (3,583) of the responders of this population scored >10 points on the pictorial ESS.
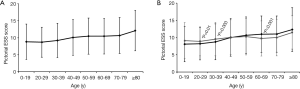
Further analysis of the interaction of different factors determined significant differences between genders when age was considered. Female subjects tended to score significantly higher than males in their 3rd lifetime decade [8.9 (4.2) vs. 8.2 (4.6) points, P=0.01] and 4th lifetime decade [9.6 (4.8) vs. 8.8 (5.2) points, P=0.003], whilst male subjects were more sleepy in their 7th lifetime decade [11.0 (5.3) vs. 9.7 (5.1) points, P<0.001] (Figure 1B). The relationship between age and EDS was closer in male than female subjects (difference in slopes, beta (male)—beta (females) =0.4, P=0.002).
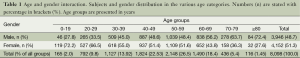
Gender distribution was significantly different in the various age categories. There were more female subjects in the age categories up to 59 years, while male subjects dominated the older age groups (P<0.001). Most of the subjects were between their 4th and 7th lifetime decade (see age and gender interaction, Table 1).
Full table
Item analysis
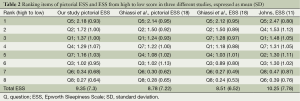
A sub-analysis of the item responses was performed (Figure 2A), with the following differences: the item “Lying down to rest in the afternoon when circumstances permit” (item q5) scored highest (P<0.001), while “as a passenger in a car stopped for a few minutes in traffic” (item q8) or “sitting and talking to someone” (item q6) scored lowest (P<0.001).

When considering gender, male subjects tended to score higher in most of the items, except for item q4 (“as a passenger in a car for an hour without a break”), in which female subjects had the higher score (Figure 2B). A rank sum analysis of each item of the pictorial ESS was performed and compared to previous work (11,18) indicating a high agreement with historical data (Table 2).
Full table
Discussion
The online use of the pictorial ESS provides valid and reliable data for assessing EDS and facilitates outreach to the general population beyond the boundaries of local primary care and secondary health service provision. Wider access to the pictorial ESS in the general population by use of modern media enabled us to collate demographic information from a large group of people within relatively short time, and to identify those who might be at risk of undiagnosed sleep disorders. The pictorial ESS was made available on a public website along with information provided regarding sleep disorders and, specifically, OSA. Although this point was not specifically tested, it is likely that the online use of the pESS raised public awareness about conditions associated with sleep disorders and OSA, thereby helping to accelerate time to diagnosis and access to treatment.
Male subjects were particularly sleepier in their 7th lifetime decade, while female subjects scored higher in their 3rd and 4th decade. Gender specific differences raise the question of whether extrinsic (traditional social structures, e.g., family during 3rd and 4th decade and retirement in the 7th decade) and intrinsic factors (hormonal influences and prevalence of OSA) might contribute to subjective symptom perception and differences in psychological “coping”, but such assumptions remain controversial (20,21). The gender specific differences in EDS, although statistically significant, were small and, although important to a large population-based cohort, they are unlikely to be clinically relevant for the individual subject.
On the other hand, our data revealed that there is a clear effect of age on the prevalence of EDS independent of gender specific differences. Several studies describe that there is no correlation between EDS and age (22-24), while others demonstrate a preference for male adults with a single peak or a bimodal distribution of EDS (4-6,25-27). However, our data for the first time revealed that higher scores in the pictorial ESS were associated with higher age, although this might have been due to responder bias.
Wakefulness and vigilance in the elderly are affected by decreased light exposure, inactivity, daytime naps, bereavement, medical conditions and medication or degenerative changes of the central nervous system (28,29). In addition, the circadian rhythm seems to change in aging people. A higher prevalence of sleep disorders like OSA, periodic limb movements, insomnia as well as other co-morbidities associated with organic failures in the elderly contribute further to more severe levels of EDS (2,26,29,30).
While marginal differences were observed between genders regarding the percentage of sleepy subjects, male subjects tended to score significantly higher overall. This is in accordance with other studies that have proposed a higher basic wake drive in women, resulting in less sleepy behaviour and relatively lower scores in the traditional ESS (30-32). Furthermore, male subjects are more likely to be overweight and to have sleep disorders (9,33). Objective data of standardized multiple measurements report significantly shorter sleep latencies in men compared to women, indicating that men are more sleepy than women using objective measures (9,34) and the effect is even more severe with older age (35). Furthermore, self-reported sleep disturbance and tiredness are diminished in the elderly (36) and, therefore, data provision to understand sleepiness in public health scenarios becomes even more important in order to provide an appropriate clinical service. In this context it is of interest to note that lying down to rest in the afternoon is a natural physiological tendency and this could explain why this item was scored highest in our analysis. On the other hand, two items that scored lowest might be explained by low social acceptance and increased levels of alertness: dozing off while sitting and talking to someone and whilst being a passenger in a car stopped in traffic.
There are clear limitations to our approach of capturing online data; no data were recorded regarding multiple confounders (snoring, witnessed apneas, shift work, ethnicity, profession, literacy problems, socio-economic factors). Participants were self-selected, leading to a responder bias. This study is not a representative observational study, because female subjects might be more likely to use health-related websites. They may respond on behalf of male partners; females are also more likely to report sleepiness as a passenger in a car and thus our data should be interpreted with caution.
Furthermore, the self-administered approach of the online pictorial ESS further allows possible errors or duplications, although the online version used allowed only one item to be ticked per question in an attempt to minimize possible errors. However, these limitations do not negate the usefulness of modern media to reach out to the general population on a large scale, raise awareness of OSA, and support local services to identify healthcare requirements. The large number of participants reveals the enormous potential of modern and social media to reach out to people for future research in this area.
Conclusions
The use of an online questionnaire, the pictorial ESS, via a charitable webpage can help to raise awareness of a common condition, OSA, which is commonly associated with subjective EDS, with significant health consequences. We detected a high prevalence of EDS in the general population, greater than shown by other community surveys (3,4,24,36). Those observations have been affected by responder bias but, nonetheless, our findings have serious implications on health burden in the general population because of the sheer numbers of subjects enrolled. Interestingly, in the studied population, gender and age data related to the symptom of sleepiness in several ways, and this had not previously been revealed by other studies, indicating specific differences that will require future evaluation.
Our approach might encourage clinical services to reach out to the general population to raise awareness of EDS and help to identify those at risk of undiagnosed sleep disorders. Consequently, this action may help to shorten the time to diagnosis and treatment. The large scale of our dataset raises the potential that there might be systematic gender and age specific differences in the perception of daytime sleepiness. However, concepts of somnificity are complex and multi-factorial and explaining the causes behind our observations will require a more tailored approach.
Acknowledgements
The data acquisition was supported by the British Lung Foundation. The University Hospital of Patras, Greece kindly supported the study trip of Panagis Drakatos to London. This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Disclosure: The authors declare no conflict of interest.
References
- Panossian LA, Veasey SC. Daytime sleepiness in obesity: mechanisms beyond obstructive sleep apnea--a review. Sleep 2012;35:605-15. [PubMed]
- Slater G, Steier J. Excessive daytime sleepiness in sleep disorders. J Thorac Dis 2012;4:608-16. [PubMed]
- Swanson LM, Arnedt JT, Rosekind MR, et al. Sleep disorders and work performance: findings from the 2008 National Sleep Foundation Sleep in America poll. J Sleep Res 2011;20:487-94. [PubMed]
- Kaneita Y, Ohida T, Uchiyama M, et al. Excessive daytime sleepiness among the Japanese general population. J Epidemiol 2005;15:1-8. [PubMed]
- Pallesen S, Nordhus IH, Omvik S, et al. Prevalence and risk factors of subjective sleepiness in the general adult population. Sleep 2007;30:619-24. [PubMed]
- Bixler EO, Vgontzas AN, Lin HM, et al. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 2005;90:4510-5. [PubMed]
- Hillman DR, Murphy AS, Pezzullo L. The economic cost of sleep disorders. Sleep 2006;29:299-305. [PubMed]
- Ronksley PE, Hemmelgarn BR, Heitman SJ, et al. Excessive daytime sleepiness is associated with increased health care utilization among patients referred for assessment of OSA. Sleep 2011;34:363-70. [PubMed]
- Slater G, Pengo MF, Kosky C, et al. Obesity as an independent predictor of subjective excessive daytime sleepiness. Respir Med 2013;107:305-9. [PubMed]
- Iranzo A. Excessive daytime sleepiness in OSA. Published in: Sleep Apnoea. Edited by McNicholas WT and Bonsignore MR. European Respiratory Society Monograph, 2010;50:17-30.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991;14:540-5. [PubMed]
- Chiner E, Arriero JM, Signes-Costa J, et al. Validation of the Spanish version of the Epworth Sleepiness Scale in patients with a sleep apnea syndrome. Arch Bronconeumol 1999;35:422-7. [PubMed]
- Chen NH, Johns MW, Li HY, et al. Validation of a Chinese version of the Epworth sleepiness scale. Qual Life Res 2002;11:817-21. [PubMed]
- Tsara V, Serasli E, Amfilochiou A, et al. Greek version of the Epworth Sleepiness Scale. Sleep Breath 2004;8:91-5. [PubMed]
- Bloch KE, Schoch OD, Zhang JN, et al. German version of the Epworth Sleepiness Scale. Respiration 1999;66:440-7. [PubMed]
- Johns MW. Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the epworth sleepiness scale: failure of the MSLT as a gold standard. J Sleep Res 2000;9:5-11. [PubMed]
- Johns MW. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 1992;15:376-81. [PubMed]
- Ghiassi R, Murphy K, Cummin AR, et al. Developing a pictorial Epworth Sleepiness Scale. Thorax 2011;66:97-100. [PubMed]
- Fisher RA. Statistical Methods and Scientific Inference. New York: Hafner, 1956.
- Vahtera J, Westerlund H, Hall M, et al. Effect of retirement on sleep disturbances: the GAZEL prospective cohort study. Sleep 2009;32:1459-66. [PubMed]
- Ito Y, Tamakoshi A, Yamaki K, et al. Sleep disturbance and its correlates among elderly Japanese. Arch Gerontol Geriatr 2000;30:85-100. [PubMed]
- Souza JC, Magna LA, Reimao R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arq Neuropsiquiatr 2002;60:558-62. [PubMed]
- Roth T, Roehrs TA. Etiologies and sequelae of excessive daytime sleepiness. Clin Ther 1996;18:562-76; discussion 561. [PubMed]
- Ohayon MM, Caulet M, Philip P, et al. How sleep and mental disorders are related to complaints of daytime sleepiness. Arch Intern Med 1997;157:2645-52. [PubMed]
- Morrell MJ, Finn L, McMillan A, et al. The impact of ageing and sex on the association between sleepiness and sleep disordered breathing. Eur Respir J 2012;40:386-93. [PubMed]
- Gander PH, Marshall NS, Harris R, et al. The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth Sleepiness scores of adults in New Zealand. Sleep 2005;28:249-53. [PubMed]
- Wu S, Wang R, Ma X, et al. Excessive daytime sleepiness assessed by the Epworth Sleepiness Scale and its association with health related quality of life: a population-based study in China. BMC Public Health 2012;12:849. [PubMed]
- Howard ME, Desai AV, Grunstein RR, et al. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am J Respir Crit Care Med 2004;170:1014-21. [PubMed]
- Kryger MH, Roth T, Dement WC. Principles and Practice of Sleep Medicine. 3rd ed. Philadelphia: WB Saunders, 2000:26-38.
- Edwards N, Wilcox I, Sullivan CE. Sleep apnoea in women. Thorax 1998;53 Suppl 3:S12-5. [PubMed]
- Baldwin CM, Kapur VK, Holberg CJ, et al. Associations between gender and measures of daytime somnolence in the Sleep Heart Health Study. Sleep 2004;27:305-11. [PubMed]
- Whitney CW, Enright PL, Newman AB, et al. Correlates of daytime sleepiness in 4578 elderly persons: the Cardiovascular Health Study. Sleep 1998;21:27-36. [PubMed]
- Health Survey for England DOH. Adult obesity prevalence. Health Survey for England and modelled estimates 2006-2008. Available online: http://www.noo.org.uk/uploads/doc/vid_7650_AdultObesityPrevalence.pdf
- Punjabi NM, Bandeen-Roche K, Young T. Predictors of objective sleep tendency in the general population. Sleep 2003;26:678-83. [PubMed]
- Unruh ML, Redline S, An MW, et al. Subjective and objective sleep quality and aging in the sleep heart health study. J Am Geriatr Soc 2008;56:1218-27. [PubMed]
- Grandner MA, Martin JL, Patel NP, et al. Age and sleep disturbances among American men and women: data from the U.S. Behavioral Risk Factor Surveillance System. Sleep 2012;35:395-406. [PubMed]


