
Regionally surgical resection of stage-IV adenocarcinoma acquired tyrosine kinases inhibitor-resistance
Introduction
A 65-year-old male presented with a mass at left lower lobe (LLL) in November 2010, without a history of smoking. Computer tomography (CT) and positron emission tomography (PET)-CT scans showed a 41 mm × 38 mm solid mass at LLL with small nodules interspersed in both lungs. The largest nodule had a maximum diameter of about 12 mm at left upper lobe (LUL) and was considered to be a metastasis according to fludeoxyglucose (FDG)-PET result. The biopsy guided by CT pathologically confirmed lung adenocarcinoma of the primary lesion.
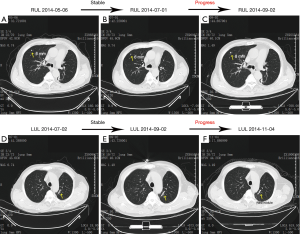
The medication history is summarized in Table 1 including chemotherapy and targeted therapy of epidermal growth factor receptor (EGFR) inhibitors. At the three months follow-up after the 1st Course of chemotherapy, CT scan showed an increase in the size of the metastatic lesion, and we decided to alter medication strategy to course 2. In February 2012, both primary and metastatic lesions progressed. EGFR mutation test of the sample collected at the time of diagnosis showed exon 19 deletions of the EGFR kinase domain. The patient started to receive tyrosine kinases inhibitor (TKI) therapy of erlotinib from March 2012 and got a partial response (PR), indicating decreases of at least 30% for both primary and metastatic lesions. However, the primary lesion progressed after 18 months, and an increase in standard uptake value (SUV) of PET/CT was noticed without other tumor activities. After discussion and paper research, we decided to surgically resect the lesion acquired resistance of EGFR TKI (Figure 1). Following 12 months reuse of erlotinib therapy after surgery, tumor progression was observed, a new lesion was found in right upper lobe (RUL), and the metastatic lesion at LUL showed an increase in size (see Figure 2). Therapy strategy remained unchanged as tumor activity was stable. At 21 months later, rapid growth was noted, and the number of metastatic lesions increased. Thus, we introduced chemotherapy (course 4) at the same time with TKI. The patient complained of severe fatigue after two cycles of chemotherapy and refused for the remaining two periods. Biopsy of the RUL lesion was conducted via CT, which showed T790M mutation of the EGFR kinase domain. Taking economic factors into consideration, the patient refused the usage of osimertinib as we recommended, and instead underwent conformal radiotherapy (95%PTV-L60Gy/30F for LUL lesion and 95%PTV-R60Gy/30F for RUL lesion). Radiation did not work well, and the tumor continued to progress. The patient started to receive AZD9291 (osimertinib) from March 2017 and gained complete response by December 2017, indicating all lesions had disappeared during the course. No tumor progression was found at follow-up in July 2018.
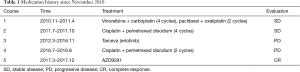
Full table

Operative techniques
The patient was placed in a right lateral decubitus position. A three ports VATS approach was carried out under general anesthesia with single lung ventilation. The surgeon stood in the ventral side of the patient to operate. A 1-cm incision was first made to place a 30-degree thoracoscopy (STORZ) in the eighth intercostal space at the mid-axillary line with the incision expanded to 2-cm to take care of the extensive adhesion. Two additional incisions were then made at the fourth intercostal space in midclavicular line (4-cm, surgical port) and the eighth intercostal space in scapular line (2-cm). Rib resection or rib spreading is not permitted, and all procedures were performed under thoracoscopic assistance. Sharp dissection was performed to separate the adhesion up to the apex, which was the densest part. Thus, we decided to separate at the end. Single-direction thoracoscopic lobectomy was achieved due to the absence of fissure leaving the artery and the pleural adhesion of the apex as the last step of the procedure. The drainage tube was stayed for ten days after surgery due to a prolonged air leak, and the patient was discharged on the 11th day postoperatively.
Comments
The patient with EGFR-mutant advanced NSCLC had received chemotherapy, TKI therapy, local therapy and the reuse of TKI therapy. Good response for the treatment was shown, and the overall survival is 80 months till now. The patient received local therapy with acquired resistance to EGFR TKI (erlotinib). Time to progression after local therapy was 12 months, and the excellent response to treatment was following the previous study (2).
When the patient was identified with acquired resistance of EGFR TKI, we evaluated with PET/CT and found no tumor activity except the primary lung cancer. Hence, we adjusted the treatment strategy of local therapy, which consisted of surgical resection, radiofrequency ablation, and radiation. The tumor was close to the hilum, which could result in poor response either way. After discussion, we decided to conduct lobectomy for LLL. The purpose of the resection was to take out part of the lung that acquired resistance, and therefore lymph node dissection was not performed according to the PET/CT result showing no other tumor activities. Owing to the usage of TKI, extensive and dense pleural adhesion was found during the process of the operation. Extensive capillary hyperplasia was observed in the adhesion, which could lead to blood oozing in multiple sites. The blood loss of oozing should be given attention because a large amount of blood oozing could result in blood coagulation dysfunction that leads to a more substantial range of bleeding. Hence, we applied energy platform (electric coagulation or ultrasonic scalpel) on separating the adhesion to minimize the amount of blood oozing.
Additionally, we observed that EGFR mutation points were different between the primary tumor of LLL and the metastasis at RUL. The first gene test was done with the samples collected at the time of diagnosis. To confirm the gene mutation of the primary lesion, we conducted NGS gene test of 139 lung cancer-related genes on the samples from resected tissue. The result showed L858R and T790M mutation at exon 21 of EGFR kinase domain. The finding was by the RUL lesion.
Interestingly, this result was different from the previous test of the biopsy before a surgical operation. The alteration of the gene mutation can be explained by the intratumoral heterogeneity of cancer, reported by last study (3) since biopsy can only capture part of the tissue instead of the whole tumor. Thus, surgical biopsy has remained the gold standard for the pathology. Regarding this feature in tumor progression, it may be considered whether the patient could gain this kind of complete response if we modify the medication strategy after the tumor acquired the first resistance to TKI. This problem should be validated with larger examples from clinical practice.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional ethics review boards of Ningbo No. 2 Hospital and written informed consent was obtained from all patients.
References
- Yang M, Zheng E, Xu X, et al. Surgical resection of the primary lesion that acquired resistance of EGFR TKI. Asvide 2019;6:016. Available online: http://www.asvide.com/article/view/29630
- Moiseyenko FV, Moiseyenko VM, Aleksakhina SN, et al. Survival Outcomes in EGFR Mutation-Positive Lung Cancer Patients Treated with Gefitinib until or beyond Progression. Oncol Res Treat 2016;39:605-14. [Crossref] [PubMed]
- Cai W, Lin D, Wu C, et al. Intratumoral Heterogeneity of ALK-Rearranged and ALK/EGFR Coaltered Lung Adenocarcinoma. J Clin Oncol 2015;33:3701-9. [Crossref] [PubMed]
(English Language Editor: Jeremy Dean Chapnick, AME Publishing Company)


