
Ischaemic conditioning of the stomach previous to esophageal surgery
Introduction
Oesophageal surgery is technically challenging and demanding. Anastomotic leakage is one of the most threatening complications after oesophageal surgery, because of its high rate of morbidity and mortality (1). Gastric conduit is the most common technique used for reconstruction in esophageal surgery. Failure of the esophagogastric anastomosis is due to multiple causes, however, conduit ischemia has been described as the most fragile aspect of esophageal reconstruction (2). Gastric ischaemic conditioning has been described and investigated through the last decades as a procedure before the operation to improve vascularization of the gastric conduit.
The aim of this study is to define the concept of ischaemic conditioning, the anatomic and physio-pathologic background, and to analyse the current evidence based on the experience and results previously published. The main intent of this manuscript is to investigate the influence of this technique in the esophageal anastomosis and leakage rates.
A comprehensive review has been made to collect all the articles related to ischaemic conditioning of the stomach since 1970 until 2018. MEDLINE and PubMed database searches were performed. Related articles cited in the chosen studies were also investigated. Both experimental studies with animals and studies with humans were included.
The esophagogastric anastomosis
Some aspects make the esophagogastric anastomosis more prone to leak than others in the digestive tube. The anatomic characteristics and the technical particularities of esophageal surgery have the leading role in this surgical complication.
After gastric mobilization, the right gastroepiploic artery (RGEA) is responsible for supplying the gastric conduit. Anatomic studies (3,4) have demonstrated that only an intramural vascular network vascularizes the upper part of the gastric tube. This part can be compromised by manipulation, tension or strangulation during surgery. The anastomosis can be under tension because it has to be mobilized to the neck or to the thorax. Moreover, the path of the gastric conduit for reaching the neck is longer than for the thorax, and it has to go through the narrow upper chest aperture. The alteration of the venous drainage of the gastric tube may also increase the possibility of ischemia of this especial conduit. Intrinsic characteristics of the esophagus, as the absence of serosa layer and the longitudinal muscle fibres, make this anastomosis more fragile.
The conceptual basis of the ischemic conditioning is that interrupting vascularization a period of time before making the anastomosis, may enable the gastric fundus to adapt to ischemic conditions. This would improve the blood flow, preventing the sudden decrease in blood supply, which becomes precarious after mobilizing the stomach, helping to maintain adequate tissue perfusion.
Physiopathology/anatomic background
The left gastric (LGA) and the short gastric (SGA) arteries supply the major blood flow to the stomach. El-Eishi et al. (5) in their studies of the arterial supply of the human stomach, demonstrated that as a general rule, branches of the main arteries run a short subserous course, penetrating the muscular layer and reaching the submucosa. In the submucosa coat, they branch and anastomose forming a plexus. Anastomosis between the right gastric artery (RGA), LGA and SGA have also been found.
Some anatomical studies have described the features of blood supply to the gastric conduit wall (6,7). LGA and SGA have been ligated while creating the gastric conduit. The gastric tube receives its vascularization from the caudal end through the RGEA and RGA. The RGA is a small vessel of about 0.2 mm, whose importance has been described because gastric pull up is easier and tension decreases after its division. The vascularization of the gastric tube is also impaired due to the necessary ligation of the left gastroepiploic artery (LGEA) from its splenic source. Hence, its remnant fills easily through the RGEA but it may entail reversed flow.
Finally, the RGEA is the exclusive blood supplier of the gastric conduit. As this artery is usually not as long as the gastric tube, the blood supply to the 20% upper cranial part of the conduit arrives through a dense microscopic network of small vessels, as has been demonstrated by injecting small particle resin in Liebermann’s study (6).
Buunen et al. (7) studied the vascular anatomy of the gastric tube and found that in 70% of the specimens an anastomosis between the right and left gastroepiploic arteries was present. Moreover, leaving the LGEA in situ increases the feeding arterial arcaded-length along the gastric tube in 5.0 cm.
Two-stage esophagectomy is occasionally done in cases of high-risk anastomosis, especially in patients with comorbidities or when poor graft perfusion is observed intraoperatively, delaying making the esophagogastric anastomosis. Oezcelik et al. [2009] (8) described their experience with a group of 37 high-risk patients and showed it is an effective strategy, with 35 delayed esophagogastric anastomosis and no leakages. This interval of time between operations would help the gastric conduit adapt to its new vascularization. But two-stage esophagectomy has the inconvenience of needing two different operations and temporal enteral nutrition through a feeding jejunostomy (with the complications that this can entail).
This delayed phenomenon has been studied by plastic surgeons with skin and muscle flaps in reconstructive surgery, who demonstrated that after partial devascularisation of pediculated skin flaps and delayed transposition, blood flow to the distal part of the flap improved due to arterial dilation (9). However, this mechanism is poorly understood.
The concept of gastric ischemic conditioning was first applied and described by Akiyama et al. (10), who diverted the stomach’s blood supply by the embolization of LGA, splenic artery (SA) and RGA with microcoils, three weeks before surgery. In the angiography of conditioned patients, dilation of the RGEA and increased flow in the upper part of the stomach was described. Measurements with a laser flow meter demonstrated that the stomach’s blood flow was better preserved after preoperative embolization therapy (PET). They theorized that the difference in blood flow before and after constructing the gastric conduit would be reduced and would help to maintain adequate blood flow to the gastric fundus. This improvement in vascularization may contribute to decrease anastomotic leaks.
Moreover, it has been demonstrated that the formation of the gastric conduit impairs arterial inflow and venous drainage in the gastric fundus, where the esophagogastric anastomosis is assembled (2,11).
Based on these characteristics, ischemic conditioning of the stomach allows the tissue to adapt to the sudden stop of the blood flow in the creation of the gastric conduit. It is theorized to be able to reduce the rate of anastomotic leak due to the improvement of the ischemia at the anastomotic site.
Studies in animals
Ischaemic conditioning has been studied in animals (12-20) undergoing laparoscopy or laparotomy, evaluating the gastric blood supply and histological changes in the gastric conduit and anastomotic site. These studies have shown alterations in the blood flow after making the gastric conduit, with a progressive recuperation of circulation within days. Moreover, histological benefits have been reported with the adaptation of the tissue to ischaemic conditions.
A sudden drop in blood flow in the stomach has been demonstrated in many studies when the gastric conduit is formed, measuring with laser Doppler flowmetry the restoration of the blood supply (13,14,17,19)
In studies with rats, Urschel et al. (20) discovered after conditioning, a progressive increase of circulation in the proximal stomach, reaching 81% of the previous values after 14 days compared with baseline, and normal blood flow was recovered after 3 weeks.
Alfabet et al. (12) performed a descriptive study with 24 rats that underwent partial gastric devascularization by ligating the left gastric vessels. In this study, tissue perfusion and microcirculation were measured at 1 cm distal from the cardiac region, where blood flow increased progressively the following days reaching the basal values in the 14th postoperative day.
Leme et al. (16) observed similar results in a comparative study with rats in which blood supply reached the initial levels at 14 days.
Benefits in the anastomotic wound healing have been reported in histological studies (15,18,19,21) observing vasodilation, angiogenesis and increased blood flow to the gastric fundus and anastomotic site.
In a study with opossums, Reavis et al. (19) performed laparoscopic ligation of RGA, LGA and short vessels. At relaparotomy, they described better circulation in the gastric fundus, with increased vasodilation and angiogenesis, less anastomotic collagen deposition, ischemic injury and muscular atrophy.
Perry et al. (18), by analysing the histology of resected anastomosis in opossums, evidenced increased neovascularization and muscularis propia preservation, decreased inflammation and less collagen deposition in animals treated with 30 days of gastric conditioning.
Lamas et al. (15) studied the histological recovery of the gastric fundus in rats after partial gastric ischemia. They concluded that ischemic injury to the tissue was higher at the 3rd–5th days postoperatively and started to decrease after 10 days, showing no difference with normal tissue at days 15–21.
Improved microcirculation is another important manifestation of possible benefit of the ischemic conditioning of the stomach. Mittermair et al. (17) in a comparative study in rats proved that gastric microcirculation improves progressively after gastric devascularisation, using intravital fluorescence microscopy to analyse the gastric microcirculation in the great and lesser curvatures at different times after the procedure.
In a comparative study with mongrel dogs (13) proximal gastric blood flow was evaluated with fluorescent microspheres 3 weeks after ligating the left gastric and SGA. They concluded that ligation of both arteries was more effective than ligating the short arteries alone or no preconditioning.
Technical aspects and options
Two techniques in patients for conditioning of the stomach have been published: the laparoscopic ischemic conditioning (LIC) and the percutaneous conditioning by interventional radiology.
LIC
The procedure consists in the surgical interruption of the gastric arteries, generally at the time of staging laparoscopy. It was first described by Nguyen et al. (22) in nine patients, with LGA ligation and jejunostomy tube placement at the time of staging laparoscopy. Since that first report, the methodology of LIC has been heterogeneous and varies from one study to another.
In most studies and series, only the LGA is interrupted, and only in 4 of them the SGA are also interrupted (23-26). It has been described as arterial ligation in continuity or with vessel division (24). Furthermore, one study (27) included the complete mobilization of the stomach, and another (28) included the preparation of the gastric conduit, and some studies describe the addition of a feeding jejunostomy tube placement (21-23,25,26). They argue that preparing the gastric tube can circumscribe necrosis of the fundus at the time of reconstruction (in case that there was impaired circulation), allowing making the anastomosis with more guarantees. Veeramootoo et al. (29) performed the only randomized control trial, comparing two groups of patients: the one with the laparoscopic staging and gastric conditioning followed by minimally invasive esophagectomy (MIE) after two weeks, compared with MIE as control group. With a laser Doppler flowmetry the flow was measured in two locations, the fundus and the great curve of the stomach. There were no differences in the perfusion at the two points between the two groups, being 38% of baseline levels the perfusion coefficient at the fundus.
Zahedi et al. (25) emphasizes an ischemic demarcation of the gastric conduit that leads to modifying the planned transection line from the expected location in 17% of the preconditioned patients. There is one study (26) describing the addition of mobilizing of the gastroesophageal junction and 4 cm of mediastinal and celiac node dissection for oncological staging. Bludau et al. (30) did not find any differences in the levels of vascular endothelial growth factor (VEGF) in the gastric fundus comparing levels before and after laparoscopic gastric conditioning (4–5 days).
In addition, gastric conditioning may enable the division of this long procedure into two shorter interventions in a way that has been shown to be feasible and safe.
On the other hand, laparoscopic ischaemic conditioning is a demanding procedure that requires experience in esophageal and minimally invasive surgery. Many disadvantages of laparoscopic conditioning have been described, such as increasing the difficulty of posterior dissection and lymphadenectomy due to adhesions (31,32). Besides, it constitutes a major surgical intervention and is associated with additional costs and general anaesthesia (surgical room, staplers, orotracheal intubation). Other complications like incarcerated hiatal hernia, arrhythmia and wound infection have been mentioned (24). There is also risk of arterial injury, bleeding and conversion to open procedure, but none of these have been reported.
Percutaneous conditioning by interventional radiology
Days or weeks before surgery, the RGA, LGA and SA are embolized with different materials (microcoils, plugs, etc.) leaving the RGEA permeable. This procedure is performed under local anaesthesia by vascular radiologists and the most common approach is through the right femoral artery. A final angiogram confirms the occlusion of these arteries. It is a minimally invasive procedure with short hospital stays of 24–48 hours. Percutaneous embolization has been described as a feasible and safe procedure, with different results regarding anastomotic leak rates in patients, with a trend to reduce the incidence of this complication.
Seven studies describe the experience with percutaneous ischemic conditioning with embolization (10,33-38). In all of them, the procedure protocol includes embolization of RGA, LGA and SA, in a variable period before surgery (5 to 21 days). In some cases, the procedure is incomplete due to difficulty of embolizing the RGA.
Akiyama et al. (10) and Isomura et al. (34) studied the effect of embolization in gastric blood flow after the creation of the gastric tube. The conditioned patients presented significant less decrease in the blood flow, compared to non-conditioned patients, describing subjectively better colour of the gastric tube after ischaemic conditioning (34) (27.5% vs. 68.9%, P<0.005).
The largest series published belongs to Miró et al. (38) including 97 patients with oesophageal reconstruction by gastroplasty with cervical anastomosis, and angiographic embolization of RGA, LGA and SA. They reported 6 anastomotic leaks (7%) that were treated conservatively.
Complications of the preoperative arterial embolization have been reported in the literature. The most frequent are mild abdominal pain, nausea and splenic infarction and necrosis (33-35,37,38). In one case, hospital stay longer than 48 hours was described (37). Difficulties in catheterization due to stenosis in the celiac trunk or due to the small size of the RGA have also been described (36). There is also one case of distal pancreatitis (36). Akiyama et al. (33) mentioned arterial extravasation inducing inflammatory changes around the vascular structures. All the complications were treated conservatively. There was one case where problems with the femoral artery such as haemorrhage were treated within the same procedure (38).
Which arteries are interrupted?
In the published articles and clinical trials using the laparoscopic approach, the interrupted arteries to cause the ischemic conditioning are different. Some of them only stop the flux of the LGA (22,27,28,31,39,40) while others ligate the LGA and SGA (23-26). In the series and articles about laparoscopic conditioning, there is no report of RGA ligation.
On the other hand, in preoperative embolization, most of them perform the complete procedure described by Akiyama et al. (10). The impossibility to embolize RGA is described as incomplete conditioning. For example, in one case the RGA could not be embolized due to anatomic difficulty. In this patient, the RGEA was not dilated and the effect of preoperative embolization was not seen.
RGA is a little artery with difficult catheterization. Isomura et al. (34) reported that failure to embolize RGA was associated with a significant decrease in gastric tissue blood flow while preparing the gastric tube, which implies that blood supply will increase when ligating the RGA. The best route described is via the LGA using a microcatheter. However, this arcade can be too small or too tortuous adding difficulty to the procedure. They also describe embolization of accessory LGA and inferior phrenic artery in two patients, to ensure maximum vascularization through RGEA. Diana et al. (35) showed the need for a second embolization procedure in two patients due to insufficient effect in angiographic control. Miró et al. (38) in his series with 97 patients, reported incomplete gastric conditioning in 9 patients due to impossibility to catheterize the RGA.
Time between gastric conditioning and surgery
The needed time between gastric conditioning and surgery to let the stomach adapt to the ischemia is controversial. Most studies show waiting periods of approximately 2 weeks (22,29,31,35-37,39,40) to perform the esophagectomy, and even in one case 75 days (24). Yet, other authors prefer waiting 4–5 days (25-28).
In experimental studies, circulation at the gastric fundus and proximal stomach after gastric conditioning was measured within an interval between 1–90 days, proving that after a sudden drop of blood flow, perfusion increases with time from ligation, reaching initial levels 2 or 3 weeks after the procedure (12,16,20).
Veeramootoo et al. (39) assessed the influence of operation timing after ischemic conditioning, in a prospective series with 42 conditioned patients. All seven patients with surgery 5 days after ischemic conditioning (laparoscopic ligation of LGA) had ischemia of the gastric conduit and leakage. On the other hand, the anastomotic leak rate for patients with 2-week delay after conditioning was 2 patients out of 35. In conclusion, operation timing after LIC had a significant impact on conduit failure rate (P<0.0001) and the benefit of ischemic conditioning at 2 weeks compared with no conditioning neared significance (P=0.07). On the other hand, in a larger study with a cohort of 419 patients (238 of them with LIC) and time interval of 4–5 days (27), leakage rates reported were similar for both groups (7.6% for LIC patients and 9.4% in controls) and no increase in the leak rate was described.
Bludau et al. (41) studied the mucosal oxygen saturation (MOS) in the stomach after laparoscopic partial gastric devascularisation (gastrolysis) in human patients, finding that immediately after gastrolysis the MOS decreased in gastric fundus, which was almost completely recovered 5 days later (at the time of reconstruction).
Ghelfi et al. (37) obtained significant differences in anastomotic leak rates in conditioned patients that underwent surgery 3 weeks after percutaneous conditioning.
There are no standardized protocols in human studies and, even inside the same series, the time for each patient is different. In these cases, the difficulty for scheduling may play an important role in the differences in timing.
Published results: series and evidences
The rational for gastric conditioning is the potential decrease in anastomotic leak rate, however, the results regarding the leak rate in the published studies are different. A trend towards a reduction of leakages is observed, but statistical significance is not always reached. The results of comparative studies using ischaemic conditioning that report leakage rates are shown in Table 1.
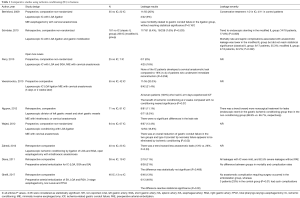
Full table
Studies that describe leak severity with ischemic conditioning show a tendency of using stents as treatment and less need for reoperation when comparing with control patients without conditioning.
Hölscher et al. (28) describes in his series 83 conditioned patients by ligating the LGA, mobilizing the stomach and preparing the gastric conduit in an average time of 4.3 days before open esophagectomy with intrathoracic anastomosis. They report 6% of leaks, all of them minor and stented, with no mortality at 90 days.
In another study by Yetasook et al. (26) describes 23 conditioned patients by laparoscopic ligation of LGA and SGA with intrathoracic anastomosis and 3 (13%) leakages were reported (two cases treated with stent and one observed).
Farran et al. (36) published a series using percutaneous conditioning in 39 patients with cervical anastomosis and reported a leakage rate of 3%. The largest series described with conditioning using preoperative arterial embolization is Miró et al. (38), with 97 patients, all of them with cervical anastomosis and 6 (6%) anastomotic leakages. These leaks were all minor, could be treated with antibiotics, nil-per-mouth and enteral nutrition.
In a recent publication by Ghelfi et al. (37) in a retrospective comparative study with 45 embolized patients and 13 controls, the difference in leakage and mortality was statistically significant, with better results for conditioned patients. Anastomotic leakage occurred in 6 conditioned patients (13%) and in 6 patients in the control group (46%, P=0.02). Besides, the mortality rate was 2% in preoperative embolization group and 23% in the control group (P=0.03).
One study (25) described that some patients presented ischemic changes in the fundus that led to modifying the planned transection line.
Isomura et al. (34) employ the same strategy as Akiyama et al. (10), demonstrating that the reduction in gastric tissue blood flow was significantly higher in non-embolized patients (27.5% vs. 68.9%, P<0.005).
Review articles, meta-analysis and randomized controlled trial of gastric conditioning
Yuan et al. (42) reviewed the anatomic basis of ischemic conditioning, the prevalence of ischemic events on the gastric conduit, the methodology to assess the microcirculation before and after gastric devascularization, animal experiments, and clinical studies until 2011. In this review, all the different techniques used to quantify the microcirculation of the gastrointestinal tract with their respective advantages and disadvantages were described.
In another review (43), the more relevant studies regarding ischemic conditioning to reduce leakage were selected. In the end, seven studies were chosen and preoperative ischemic conditioning with gastric vessel ligation prior to esophagectomy could not be demonstrated to reduce anastomotic leaks (24,26-28,31,33,39).
Kechagias et al. (44) reviewed all clinical and experimental studies regarding ischaemic conditioning. They concluded that further research with improved methodology and protocols may be able to clarify the role of ischaemic conditioning, and systematic conditioning was not recommended in all the patients.
In the literature, two meta-analysis can be found concerning the gastric ischaemic conditioning.
Markar et al. (45) studied technical factors that are known to affect anastomotic integrity, with a systematic review and meta-analysis. For the analysis of the ischaemic conditioning of the gastric conduit, they included 12 comparative studies and 1,215 patients. Pooled analysis demonstrated no significant difference between the groups in the incidence of anastomotic leak [pooled odds ratio (OR) =0.73; 95% CI: 0.5–1.06; P=0.1]. The sensitivity analysis of only preoperative vessel embolization and only laparoscopic vessel ligation showed no statistically significant differences in the incidence of leaks in pooled analysis compared with control groups (embolization: pooled OR =0.42; 95% CI: 0.14–1.25; P=0.12; ligation: pooled OR =0.78; 95% CI: 0.52–1.17; P=0.23).
A meta-analysis by Heger et al. (46) reviewed 23 articles, and included 11 for the systematic review. There were eight controlled clinical trials and three retrospective studies, with 595 conditioned patients and 557 control patients with no conditioning. In these articles, there was no significant reduction in the incidence of leakage in the conditioned group compared to control patients (OR 0.76; 95% CI: 0.51–1.13; P=0.18; I2 =0%). In addition, the two existent approaches (percutaneous and laparoscopic) were compared to each other and none of them revealed significant statistical reduction of anastomotic leakage (embolization: OR 0.49; 95% CI: 0.15–1.61; P=0.24; I2 =0%; ligation: OR 0.80; 95% CI: 0.53–1.22; P=0.31; I2 =0%). No differences in major complications and in-hospital mortality were found between both groups. This review showed that in conditioned patients the reoperation rate was lower than in control groups, and there is a trend towards less severe leaks and more conservative treatments (reoperation rate was 24.4% after preconditioning compared to 69% in non-preconditioned patients) (OR 0.20; 95% CI: 0.08–0.53; P=0.001; I2 =14%). With the current evidence, gastric preconditioning cannot be assumed to reduce the overall rate of anastomotic leakage but seems to reduce its severity.
There is only one randomized controlled trial performed by Veeramootoo et al. (29). They performed this trial with two arms: one with the laparoscopic staging and gastric conditioning followed by MIE after two weeks, and the other with MIE as control group. The endpoint was perfusion comparison at fundus and greater curvature. They concluded that LIC does not translate into an improved perfusion of the gastric conduit tip.
Discussion
Gastric ischemic conditioning before esophageal surgery has been described and used as a method to improve vascularization of the gastric conduit. Experimental studies in animals released hopeful results, demonstrating that the fundus and the anastomotic site are submitted to ischemia when the gastric conduit is created, and that there is an adaptation to this new situation that improves the blood flow.
Some studies have demonstrated these benefits in humans. Akiyama et al. first report of gastric conditioning (10) found a reduction in the blood flow drop with preoperative arterial embolization (23% vs. 65%) maintaining more than 50% of the original tissue blood flow (P=0.001). Bludau et al. (41) studied in patients the MOS in the stomach after laparoscopic partial gastric devascularisation. Immediately after gastrolysis, the MOS decreased in the gastric fundus, which was almost completely recovered 5 days later (at time of reconstruction). Nevertheless, in a randomized controlled trial Veeramootoo et al. (29) did not report any benefits in LIC, as there was no improvement of circulation at conduit tip.
Pham et al. (21) reported in an immunohistologic analysis, an increase in microvessel accounts of 29% following partial (short gastric vessel ligation) ischemic preconditioning and 67% after complete (short and left gastric vessel ligation) ischemic preconditioning (P<0.0001).
It is irrefutable that ensuring an adequate blood flow in the gastric fundus plays an essential role in securing the anastomosis. A recent study (47) assessed the circulation of the gastric graft with laser-assisted fluorescent-dye angiography (LAA). They found that leaks were significant less likely when the anastomosis was placed in an area of good circulation compared to when the anastomosis was placed in an area with a lesser blood supply assessed by LAA (2% vs. 45%, P<0.0001).
In spite of these results, it is difficult to resolve if ischemic conditioning translates into a decrease in the anastomotic leak rate. Most of the studies published showed a trend towards a decrease in leakage rates when compared to controls but have failed to show statistical significance (Table 1).
Yet, it is also relevant to note that the studies with ischemic conditioning show differences in the leakage severity, because all the studies point to minor leakages with less need for surgery and reduced morbidity in conditioned patients. In the study by Schröder et al. (27) including 419 patients, ischemic conditioning led to endoscopic stenting to treat leakages instead of surgical reintervention (14/18 patients, 77.8%) (P=0.006).
It is important to highlight the quality of the published studies, because only one of them is randomized, they only report a single-centre finding and the sample size remains small. Besides, surgical techniques and anastomosis types differ between studies. In addition, there is no established protocol for ischaemic conditioning, with different arteries involved and varying time intervals in the published series. There are many variables that can influence the leak rate (48-50); it is a multifactorial complication and drawing conclusions remains difficult.
The usability of ischemic conditioning has been discussed since its application. Urschel (51) pointed out that for gastric conditioning to be clinically useful, the benefit reducing leaks must be greater than the costs and morbidity of the conditioning procedure itself.
Probably not all the patients will benefit from this technique, but some patients who are at risk for ischemia at the site of anastomosis could be good candidates. The localization of the anastomosis plays an important role in the leakage rate, because in the thorax less part of the fundus is needed. Hence, probably the longer the gastric conduit, the bigger the benefit for the ischemic conditioning. As Kechagias et al. (44) highlighted in his review, identifying preoperative predictive factors may help to better select the patients for gastric ischemic conditioning. van Rossum et al. (52) developed a vascular calcification score assigned by computed tomographic (CT) images. In patients with anastomotic leakage, presence and severity of calcifications of the aorta and celiac axis arteries were compared to those of patients without leakage. In this study, atherosclerotic calcifications of the aorta and of the right post-celiac arteries that supply the gastric tube was an independent risk factor for anastomotic leakage after esophagectomy.
Standardization of anaesthesia and surgical techniques may play an important role to unify all the possible factors that influence the anastomotic leak rate. Moreover, the Esophageal Complications Consensus Group (ECCG) created a standardized list of complications, for defining and recording perioperative complications associated with esophagectomy (53), which will help to standardize international data collection and facilitate comparative studies and quality improvement projects.
In conclusion, there is no evidence that ischemic conditioning influences the anastomotic leak rate. However, the evidence encourages to think that it can reduce the severity of this complication. Further research with randomized controlled trials, with standardization of surgical technique and ischemic conditioning protocols, is needed to clarify these results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Blencowe NS, Strong S, McNair AGK, et al. Reporting of short-term clinical outcomes after esophagectomy: A systematic review. Ann Surg 2012;255:658-66. [Crossref] [PubMed]
- Reavis KM. The esophageal anastomosis: How improving blood supply affects leak rate. J Gastrointest Surg 2009;13:1558-60. [Crossref] [PubMed]
- Urschel JD. Esophagogastrostomy anastomotic leaks complicating esophagectomy: A review. Am J Surg 1995;169:634-40. [Crossref] [PubMed]
- Thomas DM, Langford RM, Russell RCG, et al. The anatomical basis for gastric mobilization in total oesophagectomy. Br J Surg 1979;66:230-3. [Crossref] [PubMed]
- el-Eishi HI, Ayoub SF, Abd-El-Khalek M. The arterial supply of the human stomach. Acta anat 1973;86:565-80. [Crossref] [PubMed]
- Liebermann-Meffert DM, Meier R, Siewert JR. Vascular anatomy of the gastric tube used for esophageal reconstruction. Ann Thorac Surg 1992;54:1110-5. [Crossref] [PubMed]
- Buunen M, Rooijens PP, Smaal HJ, et al. Vascular anatomy of the stomach related to gastric tube construction. Dis Esophagus 2008;21:272-4. [Crossref] [PubMed]
- Oezcelik A, Banki F, DeMeester SR, et al. Delayed Esophagogastrostomy: A Safe Strategy for Management of Patients with Ischemic Gastric Conduit at Time of Esophagectomy. J Am Coll Surg 2009;208:1030-4. [Crossref] [PubMed]
- Dhar SC, Taylor GI. The delay phenomenon. The story unfolds. Plast Reconstr Surg 1999;104:2079-91. [Crossref] [PubMed]
- Akiyama S, Ito S, Sekiguchi H, et al. Preoperative embolization of gastric arteries for esophageal cancer. Surgery 1996;120:542-6. [Crossref] [PubMed]
- Pham TH, Perry KA, Enestvedt CK, et al. Decreased conduit perfusion measured by spectroscopy is associated with anastomotic complications. Ann Thorac Surg 2011;91:380-5. [Crossref] [PubMed]
- Alfabet C, De Souza Montero EF, Paes Leme LF, et al. Progressive gastric perfusion in rats: Role of ischemic conditioning. Microsurgery 2003;23:513-6. [Crossref] [PubMed]
- Beck SM, Malay MB, Gagné DJ, et al. Experimental model of laparoscopic gastric ischemic preconditioning prior to transhiatal esophagectomy. Surg Endosc 2011;25:2470-7. [Crossref]
- Cuenca-Abente F, Assalia A, del Genio G, et al. Laparoscopic partial gastric transection and devascularization in order to enhance its flow. Ann Surg Innov Res 2008;2:3. [Crossref] [PubMed]
- Lamas S, Azuara D, de Oca J, et al. Time course of necrosis/apoptosis and neovascularization during experimental gastric conditioning. Dis Esophagus 2008;21:370-6. [Crossref] [PubMed]
- Fernando L, Leme P, Frasson E, et al. Videolaparoscopic model for the gastric ischemic conditioning in rats. Acta Cir Bras 2004;19:565-70.
- Mittermair C, Klaus A, Scheidl S, et al. Functional capillary density in ischemic conditioning: implications for esophageal resection with the gastric conduit. Am J Surg 2008;196:88-92. [Crossref] [PubMed]
- Perry KA, Banarjee A, Liu J, et al. Gastric ischemic conditioning increases neovascularization and reduces inflammation and fibrosis during gastroesophageal anastomotic healing. Surg Endosc 2013;27:753-60. [Crossref] [PubMed]
- Reavis KM, Chang EY, Hunter JG, et al. Utilization of the delay phenomenon improves blood flow and reduces collagen deposition in esophagogastric anastomoses. Ann Surg 2005;241:736-45; discussion 745-7. [Crossref]
- Urschel JD, Antkowiak JG, Delacure MD, et al. Ischemic conditioning (Delay Phenomenon) improves esophagogastric anastomotic wound healing in the rat. J Surg Oncol 1997;66:254-6. [Crossref] [PubMed]
- Pham TH, Melton SD, McLaren PJ, et al. Laparoscopic ischemic conditioning of the stomach increases neovascularization of the gastric conduit in patients undergoing esophagectomy for cancer. J Surg Oncol 2017;116:391-7. [Crossref] [PubMed]
- Nguyen NT, Longoria M, Sabio A, et al. Preoperative laparoscopic ligation of the left gastric vessels in preparation for esophagectomy. Ann Thorac Surg 2006;81:2318-20. [Crossref] [PubMed]
- Perry KA, Enestvedt CK, Pham TH, et al. Esophageal replacement following gastric devascularization is safe, feasible, and may decrease anastomotic complications. J Gastrointest Surg 2010;14:1069-73. [Crossref] [PubMed]
- Nguyen NT, Nguyen XM, Reavis KM, et al. Minimally invasive esophagectomy with and without gastric ischemic conditioning. Surg Endosc 2012;26:1637-41. [Crossref] [PubMed]
- Zahedi M, Ganai S, Yetasook AK, et al. Tu1767 Laparoscopic ischemic conditioning as a modality to reduce gastric conduit morbidity following esophagectomy. Gastroenterology 2012;142:S-1094. [Crossref]
- Yetasook AK, Leung D, Howington JA, et al. Laparoscopic ischemic conditioning of the stomach prior to esophagectomy. Dis Esophagus 2013;26:479-86. [Crossref] [PubMed]
- Schröder W, Höscher AH, Bludau M, et al. Ivor-lewis esophagectomy with and without laparoscopic conditioning of the gastric conduit. World J Surg 2010;34:738-43. [Crossref] [PubMed]
- Hölscher AH, Schneider PM, Gutschow C, et al. Laparoscopic ischemic conditioning of the stomach for esophageal replacement. Ann Surg 2007;245:241-6. [Crossref] [PubMed]
- Veeramootoo D, Shore AC, Wajed SA. Randomized controlled trial of laparoscopic gastric ischemic conditioning prior to minimally invasive esophagectomy, the LOGIC trial. Surg Endosc 2012;26:1822-9. [Crossref] [PubMed]
- Bludau M, Hölscher AH, Vallböhmer D, et al. Vascular endothelial growth factor expression following ischemic conditioning of the gastric conduit. Dis Esophagus 2013;26:847-52. [Crossref] [PubMed]
- Berrisford RG, Veeramootoo D, Parameswaran R, et al. Laparoscopic ischaemic conditioning of the stomach may reduce gastric-conduit morbidity following total minimally invasive oesophagectomy. Eur J Cardiothorac Surg 2009;36:888-93. [Crossref] [PubMed]
- Varela E, Reavis KM, Hinojosa MW, et al. Laparoscopic gastric ischemic conditioning prior to esophagogastrectomy: Technique and review. Surg Innov 2008;15:132-5. [Crossref] [PubMed]
- Akiyama S, Kodera Y, Sekiguchi H, et al. Preoperative embolization therapy for esophageal operation. J Surg Oncol 1998;69:219-23. [Crossref] [PubMed]
- Isomura T, Itoh S, Endo T, et al. Efficacy of gastric blood supply redistribution by transarterial embolization: Preoperative procedure to prevent postoperative anastomotic leaks following esophagoplasty for esophageal carcinoma. Cardiovasc Intervent Radiol 1999;22:119-23. [Crossref] [PubMed]
- Diana M, Hbner M, Vuilleumier H, et al. Redistribution of gastric blood flow by embolization of gastric arteries before esophagectomy. Ann Thorac Surg 2011;91:1546-51. [Crossref] [PubMed]
- Farran L, Miro M, Alba E, et al. Preoperative gastric conditioning in cervical gastroplasty. Dis Esophagus 2011;24:205-10. [Crossref] [PubMed]
- Ghelfi J, Brichon PY, Frandon J, et al. Ischemic gastric conditioning by preoperative arterial embolization before oncologic esophagectomy: A Single-Center Experience. Cardiovasc Intervent Radiol 2017;40:712-20. [Crossref] [PubMed]
- Miró M, Farran L, Estremiana F, et al. ¿Puede el acondicionamiento gástrico disminuir la incidencia de dehiscencia anastomótica esofagogástrica cervical? Cir Esp 2018;96:102-8. [Crossref] [PubMed]
- Veeramootoo D, Shore AC, Shields B, et al. Ischemic conditioning shows a time-dependant influence on the fate of the gastric conduit after minimally invasive esophagectomy. Surg Endosc 2010;24:1126-31. [Crossref] [PubMed]
- Wajed SA, Veeramootoo D, Shore AC. Surgical optimisation of the gastric conduit for minimally invasive oesophagectomy. Surg Endosc 2012;26:271-6. [Crossref] [PubMed]
- Bludau M, Hölscher AH, Vallböhmer D, et al. Ischemic conditioning of the gastric conduit prior to esophagectomy improves mucosal oxygen saturation. Ann Thorac Surg 2010;90:1121-6. [Crossref] [PubMed]
- Yuan Y, Duranceau A, Ferraro P, et al. Vascular conditioning of the stomach before esophageal reconstruction by gastric interposition. Dis Esophagus 2012;25:740-9. [Crossref] [PubMed]
- Ney A, Kumar R. Does preoperative ischaemic conditioning with gastric vessel ligation reduce anastomotic leaks in oesophagectomy? Interact Cardiovasc Thorac Surg 2014;19:121-4. [Crossref] [PubMed]
- Kechagias A, Van Rossum PS, Ruurda JP, et al. Ischemic Conditioning of the Stomach in the Prevention of Esophagogastric Anastomotic Leakage after Esophagectomy. Ann Thorac Surg 2016;101:1614-23. [Crossref] [PubMed]
- Markar SR, Karthikesalingam A, Thrumurthy S, et al. Volume-outcome relationship in surgery for esophageal malignancy: systematic review and meta-analysis 2000-2011. J Gastrointest Surg 2012;16:1055-63. [Crossref] [PubMed]
- Heger P, Blank S, Diener MK, et al. Gastric preconditioning in advance of esophageal resection-Systematic review and meta-analysis. J Gastrointest Surg 2017;21:1523-32. [Crossref] [PubMed]
- Zehetner J, DeMeester SR, Alicuben ET, et al. Intraoperative assessment of perfusion of the gastric graft and correlation with anastomotic leaks after esophagectomy. Ann Surg 2015;262:74-8. [Crossref] [PubMed]
- Huang J, Zhou Y, Wang C, et al. Logistic regression analysis of the risk factors of anastomotic fistula after radical resection of esophageal-cardiac cancer. Thorac Cancer 2017;8:666-71. [Crossref] [PubMed]
- Van Daele E, Van De Putte D, Ceelen W, et al. Risk factors and consequences of anastomotic leakage after Ivor Lewis oesophagectomy. Interact Cardiovasc Thorac Surg 2016;22:32-7. [Crossref] [PubMed]
- Markar SR, Arya S, Karthikesalingam A, et al. Technical factors that affect anastomotic integrity following esophagectomy: Systematic review and meta-analysis. Ann Surg Oncol 2013;20:4274-81. [Crossref] [PubMed]
- Urschel JD. Esophagogastric anastomotic leaks: The importance of gastric ischemia and therapeutic applications of gastric conditioning. J Invest Surg 1998;11:245-50. [Crossref] [PubMed]
- van Rossum PS, Haverkamp L, Verkooijen HM, et al. Calcification of arteries supplying the gastric tube: a new risk factor for anastomotic leakage after esophageal surgery. Radiology 2015;274:124-32. [Crossref] [PubMed]
- Low DE, Alderson D, Cecconello I, et al. International consensus on standardization of data collection for complications associated with esophagectomy: Esophagectomy Complications Consensus Group (ECCG). Ann Surg 2015;262:286-94. [Crossref] [PubMed]


