
One-stage video-assisted thoracic surgery for bilateral multiple pulmonary nodules
Introduction
With the widespread use of multi-slice spiral computed tomography (CT) and the increasing popularization of health examination, the detection rate of pulmonary nodules has climbed year to year, from 0.2% to 40–60% (1). Among the cases detected, a certain proportion has been related to bilateral multiple pulmonary nodules (BMPNs). For these patients, there is still heated debate concerning the best treatment plan. In trying to find the optimum path of diagnosis and possible treatment for these patients, we performed a one-stage video-assisted thoracic surgery (VATS) in our hospital. This studies aim was to investigate the clinical effect and the value of applying one-stage VATS for BMPNs. Ultimately, the patients had satisfactory surgical results and recovered well.
Methods
Inclusive and exclusive criteria of patients
Inclusive criteria
Patients underwent lung-function testing, bronchoscopy, CT scans, complete blood counts and serum biochemistry tests. Positron emission tomography-CT (PET-CT) was not included as a conventional examination for patients. Their preoperative examinations showed possibility of bilateral multiple primary lung cancer (MPLC). Each of the patients’ situation had been multidisciplinary discussed before surgery to ensure one-staged VATS was suitable. Patients were not permitted from smoking or drinking for over 7 days before the surgeries. Before the operations, the patients all signed informed consent forms for one-staged VATS.
Exclusive criteria
Preoperative examinations indicated advanced lung cancer, metastasis from other tumors and other benign lesions. Multidisciplinary discussion before surgery concluded that one-staged VATS might be intolerable. Patients rejected one-staged VATS.
We retrospectively analyzed the clinical data of patients in our department between January 1st, 2016 and June 30th, 2018. In total, there were 132 patients in whom bilateral MPLC was suspected. Eighteen of them underwent one-stage VATS. The others rejected one-staged surgery due to economic burden, risk factors and other reasons. They underwent unilateral surgery or two-stage surgery or no treatment.
The clinical data, including basic characteristics, results of preoperative examinations, duration of surgery, time of keeping chest drains, postoperative complications, time of hospitalization, and tumor characteristics, were collected.
All resected specimens including the lymph nodes were examined for pathologic staging, and histologic typing was formed according to the World Health Organization classification. At least three senior pathologists at our hospital signed the pathologic report. Regarding primary lung cancer, TNM stage was determined according to the American Joint Committee on Cancer staging system, 8th edition, and the Revised International System for Staging Lung Cancer.
The study was approved by Huazhong University of Science and Technology Tongji Medical College (Wuhan, China) ethics review committee.
Clinical data of patients
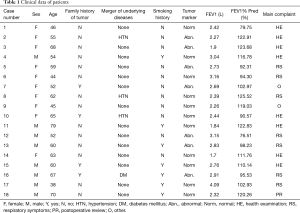
Among the 18 patients mentioned, there were 8 males and 10 females, with an age range of 38–79 (57.72±10.49) years. Eight of them were found by BMPNs through routine physical examination, 7 while coming to the hospital for respiratory symptoms like cough, sputum and hemoptysis, 2 when visiting the hospital for irrelevant symptoms like abdominal pain and gynecologic symptoms, and 1 was found in routine reexamination after a left upper lung adenocarcinoma resection 2 years ago.
Three female patients had hypertension, 1 male patient had diabetes mellitus, 7 male patients had a smoking history, and 4 patients had a history of a tumor.
Preoperative examinations showed that 7 patients had abnormal tumor markers. However, the tumor markers were slightly elevated (higher than normal value <20.00%), which indicated the high possibility of advanced-staged lung cancer and the relatively low possibility of small cell lung cancer (SCLC) (2,3).
A preoperative pulmonary function test showed that forced expiratory volume in one second (FEV1) was 1.70–4.09 (2.72±0.55) L and the FEV1/predicted value ratio (FEV1% Pred) was 76.51–125.52% (104.39%±15.55%). In the 18 patients, 42 nodules were found in both lungs, 20 in the left lung and 22 in the right lung, with an average of 2.3 nodules per person (Table 1).
Full table
Clinical data of nodules
A total of 42 pulmonary nodules were found in 18 patients, with an average of 5–35 (14.19±7.40) mm diameter. Thirty-two nodules were ground glass opacity (GGO) (76.19%), and there were 24 nodules on the upper lobe, 12 on the lower lobe and 6 nodules on the middle lobe (Table 2, Figure 1).

Full table

Results
Surgical data
Anesthetizations adopted general anesthesia, double-cavity tracheal cannulas and one-lung ventilation. The patients were in full lateral position on the operating table, right side up, and two arms were forward and fixed on the special support. Depending on the operating table, sandbags were needed to extend the ribs in order to improve exposure in the occasional absence of rib spreading.
For very small nodules, we applied CT-guided localization with medical glue and coeruleum methylenum injection to locate the lesions preoperatively. The choice of surgical priority side depended on the characteristic of the nodules. We firstly dealt with the nodules in relatively larger size, for they had higher malignant potential (4). If the bilateral pulmonary nodules were similar in size, number, and likelihood of malignancy, the right pulmonary nodule was removed first. The operation plan was determined by the size and location of nodules, the patient’s pulmonary function reserve, and the frozen section examinations.
We used single-port and double-port VATS to complete the surgery. The patient was lying in the lateral position. Incisions of 3–5 cm were made in front of the midaxillary line (Figure 2). Olympus 30-degree thoracoscopy (Figure 3) was placed to observe the development of thoracic adhesion, pulmonary fissure, and the location of the lesion. According to the location of the lesion, the way of resection, and difficulty of operation, it was decided whether to add another endoscopic port. After the operation, 1–2 #12 CVC drainage tubes or #16 drainage tubes were placed in the thoracic cavity.
After one side of the operation was completed, the patient was turned over. Based on the ventilation status, it was decided whether to continue the contralateral operation or not. If the patient was tolerating well, the opposite-side operation was performed with the same method.
Postoperative data
Surgical procedures
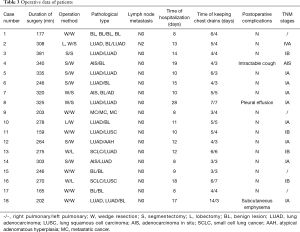
All patients underwent single-port and double-port VATS surgeries. No operations turned into thoracotomy. Wedge resection was performed in 26 (65.00%) patients, segmentectomy in 10 (25.00%) patients, and lobectomy in 4 (10.00%) patients.
Unilaterally lobar plus lobal wedge plus contralateral segmental resection was performed in 1 case (5.56%), unilaterally lobal plus contralateral wedge resection was performed in 3 cases (16.67%), unilaterally segmental plus contralateral wedge resection was performed in 7 cases (38.89%), bilaterally segmental resection was performed in 1 (5.56%), and bilateral wedge resection was performed in 6 cases (33.33%) (Table 3).
Full table
Pathological data
There were 14 benign lesions (35.71%), 1 atypical adenomatous hyperplasia (2.38%) and 27 malignant tumors (62.90%). Among the malignant tumors, there were 19 primary lung adenocarcinomas, 2 squamous cell carcinomas, 2 small cell carcinomas and 3 metastatic tumors.
Unilateral primary lung tumors were observed in 5 cases (27.78%) and bilateral primary lung tumors were observed in 9 cases (50.00%). Lymph node metastases were only found in 1 patient (Table 3).
Postoperative hospitalization data
The overall duration of hospitalization after surgery was 12.58±5.87 days. Postoperative complications occurred in 3 cases (16.7%), subcutaneous emphysema in 1 case, pleural effusion in 1 case and intractable cough in 1 case (Table 3). No patient died within 30 days after the operation.
Discussion
At present, there is no unified consensus or guidance on the diagnosis and treatment of BMPNs. Clinically, there is still controversy about the diagnosis and treatment.
The size, location and the characteristic of nodules usually determine the means of diagnosis token. The accuracy rate of percutaneous lung biopsy is relatively low for nodules centrally located, of small size and in small solid proportions. For pulmonary nodules, especially for those of GGO, the diagnostic effect of PET-CT is often limited (5,6). Indeed, it is usually impossible to clinically determine the nature of the pulmonary nodules with 100% certainty. As is often the case, we can only get a tendentious diagnosis of the nature of nodules through a series of examinations. However, with the advancement of VATS, especially uniport VATS, patients can receive the same results as taking traditional thoracotomy by suffering from less trauma and recovering more quickly. Therefore, we value VATS not only as an important treatment, but also as an effective examination method. For patients with small peripheral nodules, VATS should be taken into consideration. During the operation, firstly, we do wedged resection of the lesion. Based on the results of the frozen section, we then decide whether to expand the scope of resection. In this way, the diagnosis can be clear and surgical resection achieved.
Whether to intervene the nodules, when to take the intervention, whether to take it bilaterally or unilaterally, concurrently or separately, are all important considerations when deciding up the treatment plan. Furthermore, on the one hand, we need to avoid over-treatment, while on the other hand, we have to avoid delays so as not to miss the best timing for treatment.
So far, surgical resection is the main treatment for lung cancer. For patients with BMPNs, we should be cautious with the diagnosis of lung cancer regarding contralateral lung metastasis, and be aware of the possibility of MPLC. MPLC is mostly early cancer and the survival rate in the following 5 years after the surgeries is relatively high. Proposed originally by Beyreuther (7) in 1924, MPLC used to be regarded as a rare disease, but in recent years, domestic and foreign research reports all point out that its incidence is on the rise (8,9). MPLC and advanced lung cancer share different clinical treatments and prognoses. The latter has almost no operative chance, and the long-term survival rate is low. It has been reported that the 5-year survival rate of stage I MPLC is as high as 75.8%, which is much higher than that of advanced lung cancer (10). When we suspect BMPNs of all being cancerous, but without evidence to show that they are advanced lung cancers, active treatments are necessary and surgical resections should be the first choice.
Moreover, the correct surgical procedures to choose is also crucial for those who may have MPLCs. For example, compared to one-stage surgery, staging surgery is relatively safer and less traumatic. Its postoperative recovery period is often shorter than one-staged surgery. But, as the second operation usually happens at least 4 weeks later, the risk of progression of contralateral tumors cannot be avoided. As for one-stage bilateral pulmonary surgery, one of its limits is that it has special requirements, such as higher requirements for patients’ physical conditions, specific size and the locations of bilateral lung lesions, and certain types of medical teams. However, the fact that one operation can resect multiple lesions of both lungs does warrant our attention, because doing so can circumvent the trauma of the second operation and reduce the medical burden of patients. Additionally, it also avoids the risk of tumor progression and change. Our study showed that the safety of bilateral simultaneous surgery could be ensured by detailed preoperative evaluation, meticulous operation, and professional management after operation. Similarly, Yao et al. (11) reported 29 cases of simultaneous bilateral pulmonary resections by VATS for multiple small nodules. All patients were discharged successfully after operation.
The retrospective studies support that one-stage VATS could be considered in patients with BMPNs. In our study, all patients underwent VATS, because the application of video-assisted thoracoscopic surgery can reduce the trauma of surgery. We believe that thoracoscopic surgery is the basis for simultaneous bilateral lung surgery. Under the premise of ensuring the completeness of excision, sub-lobar resection is a better choice, and can retain pulmonary tissue. However, there is still a need for further multi-center and large-sample studies on the safety and long-term prognosis of simultaneous thoracoscopic surgery for bilateral pulmonary multiple nodules.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Huazhong University of Science and Technology Tongji Medical College (Wuhan, China) ethics review committee (Approval ID: JR-IRB20190106).
References
- Ost DE, Gould MK. Decision making in patients with pulmonary nodules. Am J Respir Crit Care Med 2012;185:363-72. [Crossref] [PubMed]
- Cheng L, Deng L, Li H, et al. Application of Serum Tumor Markers in the Diagnosis and Clinical Staging of Lung Cancer. Hua zhong ke ji da xue xue bao 2010;39:402-7.
- Schneider J, Philipp M, Velcovsky HG, et al. Pro-gastrin-releasing peptide (ProGRP), neuron specific enolase (NSE), carcinoembryonic antigen (CEA) and cytokeratin 19-fragments (CYFRA 21-1) in patients with lung cancer in comparison to other lung diseases. Anticancer Res 2003;23:885-93. [PubMed]
- Li F, Sone S, Abe H, et al. Malignant versus benign nodules at CT screening for lung cancer: comparison of thin-section CT findings. Radiology 2004;233:793-8. [Crossref] [PubMed]
- Wu HB, Wang L, Wang QS, et al. Adenocarcinoma with BAC features presented as the nonsolid nodule is prone to be false-negative on 18F-FDG PET/CT. Biomed Res Int 2015;2015:243681. [PubMed]
- Suzawa N, Ito M, Qiao S, et al. Assessment of factors influencing FDG uptake in non-small cell lung cancer on PET/CT by investigating histological differences in expression of glucose transporters 1 and 3 and tumour size. Lung Cancer 2011;72:191-8. [Crossref] [PubMed]
- Beyreuther H. Multiplicität von Carcinomen bei einem Fall von sog. “Schneeberger” Lungenkrebs mit Tuberkulose. Virchows Archiv für pathologische Anatomie und Physiologie und für klinische Medizin 1924;250:230-43. [Crossref]
- Ishigaki T, Yoshimasu T, Oura S, et al. Surgical treatment for metachronous second primary lung cancer after radical resection of primary lung cancer. Ann Thorac Cardiovasc Surg 2013;19:341-4. [Crossref] [PubMed]
- Ishikawa Y, Nakayama H, Ito H, et al. Surgical treatment for synchronous primary lung adenocarcinomas. Ann Thorac Surg 2014;98:1983-8. [Crossref] [PubMed]
- Mun M, Kohno T. Single-stage surgical treatment of synchronous bilateral multiple lung cancers. Ann Thorac Surg 2007;83:1146-51. [Crossref] [PubMed]
- Yao F, Yang H, Zhao H. Single-stage bilateral pulmonary resections by video-assisted thoracic surgery for multiple small nodules. J Thorac Dis 2016;8:469-75. [Crossref] [PubMed]




