
Impacts of incomplete revascularization following off-pump coronary artery bypass grafting on clinical outcomes of patients with triple-vessel lesions: insights from a single-center study of propensity-matched data
Introduction
Complete revascularization (CR) is considered as a requirement in percutaneous coronary intervention (PCI) and is implied when a patient is referred for coronary artery bypass grafting (CABG) (1-3). A recent meta-analysis has promoted the status quo, i.e., that most favorable outcomes are associated with surgical CR (1), but what of the patient who is not fully revascularized? Increasing evidence has suggested that surgical CR may not be the only overriding tenet (3). Comorbidities and anatomical variables often conspire against a successful surgical CR Jeny(4-6). The concept of “reasonable incomplete revascularization (IR)” was initially proposed by Dauerman in 2011 (7). Since then, based on increasing reports, IR has been considered an acceptable strategy of surgical revascularization in some categories of patients (7-11).
IR was noted as a weak point of off-pump CABG during its initial practice (12). However, throughout the past decade, off-pump CABG became one of the mainstream procedures of CABG because of its low incidence of perioperative complications. Many surgeons have adopted the off-pump technique as their routine, and the data are supportive of off-pump CABG providing comparable completeness of revascularization compared with on-pump CABG (13). Additionally, current comparisons presented several limitations. The total off-pump experience was relatively small in previous randomized controlled trials, such as the SYNTAX and ART trials (14). In observational studies, on-pump CABG had usually been the first-choice strategy (15,16), thus introducing a selection bias with high-risk patients undergoing off-pump CABG.
The extent of IR has been investigated in some cardiac surgery trials, and real-life registry trials have indicated a surgical IR rate of 13–40% (4-11). The range of IR rate reported in previous studies was shown to be wide. The magnitude of the impacts of off-pump IR on clinical outcomes of patients with triple-vessel disease remained unclear in real-world practice. Additionally, data about the incidence of off-pump IR and the impacts of off-pump IR on clinical outcomes came almost entirely from American and European published studies; there has been lack of data from Chinese patients with triple-vessel disease.
The current study aimed to determine the incidence of IR in a cohort of 1,349 consecutive Chinese patients with a triple-vessel lesion who underwent first-time, isolated off-pump CABG in our institute, where off-pump CABG surgery has been the first choice in patients referring for surgical revascularization. This study also provided a present-day assessment of the impacts of off-pump IR vs. off-pump CR on in-hospital and follow-up outcomes in a single-center study of propensity-matched data.
Methods
Definition of IR
There were various criteria of CR in previous reports, including anatomical or traditional, functional, numerical, score-based, and physiology-based CR (1). Considering the advantages and disadvantages of various criteria, the retrospective characteristics of this study and the time span of this study population, the criterion of anatomic CR was available in this study. Incomplete surgical revascularization was defined as any diseased coronary system with vessel size ≥1.5 mm with at least one significant diameter stenosis >50% failing to receive a graft. The same definition was used in the majority of previous studies (1,17).
Study protocol
This study protocol was approved by the ethics committee of Zhongshan Hospital Fudan University (No. Y2017-049) and was consistent with the Declaration of Helsinki.
The inclusion criteria were triple-vessel lesions, isolated off-pump CABG, and no history of cardiac surgery. Exclusion criteria were as follows: concomitant procedures, hybrid procedures, revascularization of the left anterior descending artery (LAD) using arterial or venous conduits other than the left internal mammary artery (LIMA), and intra-operative emergent conversion to on-pump CABG.
All included patients were entered into either an IR group (patients who receiving off-pump IR) or a CR group (patients who receiving off-pump CR). The decision to assign patients to the IR group or the CR group was made by two independent researchers. Any disagreement was resolved by discussion with the senior researchers. Peri-operative data were obtained from our institutional database and reviewed using a standard data collection form. If patients developed symptoms or doubtful symptoms of coronary heart disease during follow-up, clinic visit should be performed at the time; on the other hand, asymptomatic patients were followed up at 3 and 6 months after discharge, and thereafter at 6-month intervals. Data collection was performed by trained staff (two people). The trained staff, however, did not know the purpose of the study.
Baseline and procedure characteristics and the incidence of IR following off-pump CABG were investigated and analyzed. The in-hospital and follow-up outcomes between the IR group and the CR group were compared. To reduce the effects of treatment selection bias and potential confounding on clinical outcomes, differences in baseline characteristics were adjusted by using propensity score matching (1:1).
Surgical techniques and postoperative medications
In our institute, off-pump CABG surgery has been the first choice in patients who were referred for surgical revascularization, whereas on-pump CABG was conducted in patients with severely impaired left ventricular function, deeply intra-myocardial target vessels, previous cardiac surgery, or concomitant open-heart surgery. All patients received off-pump CABG through a median full sternotomy. The LIMA grafting to the LAD has been the first choice. Saphenous vein and radial artery were harvested with an open technique, and sequential or separate aorto-saphenous vein or radial artery-coronary bypass grafting was performed in the remaining coronary arteries. Choices of conduits and their configurations for target vessels other than the LAD were determined on the basis of conduit availability, number of grafts, the target territory, and the surgeon’s preference concerning these factors for achieving CR. The details of the off-pump CABG procedure were consistent with those of previous studies (18). The quality of anastomosis was assessed intra-operatively after grafting with a transit-time flow probe (Medistim Butterfly Flowmeter, Oslo, Norway). Measured pulsatility index of grafts or sequential segments was lower than 5, suggesting high-quality anastomoses. Otherwise, re-anastomosis may be considered.
Subcutaneous injection of low molecular weight heparin within 6 hours following off-pump CABG was routinely conducted, except for patients receiving re-operation for bleeding. Statin medication, aspirin, and clopidogrel were routinely prescribed to all patients starting from postoperative day 1 or 2. Clopidogrel was discontinued after 1 year, but statin medication and aspirin were continued indefinitely.
Outcomes
Follow-up outcomes included all-cause mortality and repeat revascularization. Repeat revascularization was defined as a second percutaneous coronary intervention or a repeat CABG surgery to deal with graft failure or new high-grade native coronary artery stenosis.
In-hospital outcomes included surgical mortality and major postoperative morbidity. Surgical mortality was defined as death within 30 days after surgery or during the same hospitalization. Major postoperative morbidity included myocardial infarction associated with CABG, re-exploration for bleeding, deep sternal wound infection, stroke, postoperative dialysis, and prolonged ventilation of more than 24 hours (19-21).
In addition, the incidence of IR following off-pump CABG was recorded.
Statistical analysis
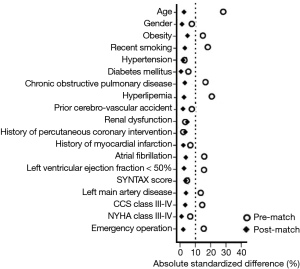
Normally distributed continuous variables were expressed as the mean ± standard deviation and were compared between groups using the Student’s t-test. Nonnormally distributed continuous variables were expressed as the median and quartiles and were compared between groups with the Wilcoxon rank sum test. Categorical variables were expressed as frequency distributions and single percentages and were compared between groups using χ2 test or Fisher’s exact test, when appropriate. To reduce the effects of treatment selection bias and potential confounding on clinical outcomes, differences in baseline were adjusted by using propensity score matching. The non-parsimonious logistic regression propensity model included the following 19 variables: age; gender; obesity (body mass index of more than 30 kg/m2); smoking history; hypertension; diabetes mellitus; chronic obstructive pulmonary disease; hyperlipidemia; prior cerebro-vascular accident; renal dysfunction; history of percutaneous coronary intervention; recent myocardial infarction; atrial fibrillation; impaired left ventricular function (left ventricular ejection fraction of less than 50%); SYNTAX score; left main artery disease; Canadian Cardiovascular Society (CCS) class III–IV; New York Heart Association (NYHA) class III–IV; and emergency operation. Propensity scores were created to quantify the likelihood of a given patient receiving off-pump IR. Pairs of patients receiving off-pump IR and off-pump CR were derived using greedy 1:1 matching with a calliper of width 0.2 of standard deviation of the logit of the propensity score. Every patient in the IR group was matched with a patient in the CR group by the closest propensity score (within 0.030). The quality of the matching was assessed by comparing selected pre-treatment variables in propensity score-matched patient using the standardized mean difference. McNemar and paired Student’s t-tests were used for comparisons with the matched groups. Multivariate Cox regression analysis was used to determine the independent risk factors for cardiac death at follow-up. The intervals to death and events were compared using the Kaplan-Meier method with the log-rank test for group comparisons. The impacts of grouping (IR vs. CR) as independent factors on in-hospital outcomes were evaluated by multivariable logistic regression analysis using the backward elimination method. A value of two-sided P less than 0.05 was considered statistically significant. Statistical analysis was performed with SPSS statistical package version 22.0 (SPSS Inc., Chicago, IL, USA).
Results
Study population
From January 2011 to December 2013, 1,420 consecutive patients who met inclusion criteria were identified, accounting for 73.0% of all CABG cases during the same period. Among them, 71 patients were excluded (revascularization of the LAD using the right internal mammary artery, radial artery, or saphenous vein conduit in 58 patients and intra-operative emergent conversion to on-pump CABG in 13), leaving 1,349 eligible patients for data analysis.
Among all included patients, 268 patients who underwent IR were entered into the IR group, and the remaining 1,081 patients who received CR were entered into the CR group. As shown in Table 1, patients in the IR group compared with the CR group were older (66.8±9.3 vs. 65.3±8.2 years, P=0.009), had higher proportions of women and NYHA class III and IV (17.5% vs. 12.4%, P=0.027, and 19.8% vs. 14.7%, P=0.041, respectively) and were more likely to have concomitant with diabetes mellitus treated with insulin and atrial fibrillation (1.9% vs. 0.6%, P=0.048, and 3.4% vs. 1.4%, P=0.038, respectively). In addition, significant differences were observed between the two groups in the distribution of low, intermediate and high SYNTAX score (P=0.035), and the IR group had a higher proportion of high SYNTAX score (33 or more) compared to the CR group.

Full table
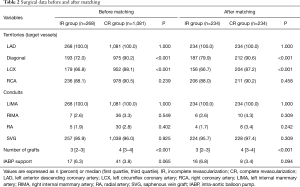
Table 2 lists diseased territories, grafted territories, and the grafts. The diagonal arteries and circumflex territories were more likely to remain ungrafted in the IR group compared with the CR group (72.0% vs. 90.2%, P<0.001, and 66.8% vs. 88.1%, P<0.001, respectively). No significant difference between the two groups was found in the proportions of use of arterial and venous conduits. Patients in the IR group compared with the CR group received a higher proportion of emergency operation (4.8% vs. 2.6%, P=0.039) but a significantly lower number of grafts (median, 3 vs. 4, P<0.001). Patients in the IR group had a trend of a higher proportion of intra-aortic balloon pump supports in comparison with patients in the CR group (6.3% vs. 3.8%, P=0.065).
Full table
Incidence of off-pump IR
In the cohort of 1,349 consecutive Chinese patients undergoing first-time, isolated off-pump CABG with LIMA grafting to the LAD, 268 patients received IR, and the incidence of off-pump IR was 19.9%. This off-pump IR rate was achieved with a high proportion (over 70.0%) of off-pump CABG to all CABG cases during the same period.
Propensity score matching
Bivariate analyses were conducted to examine differences in baseline characteristics between patients in the IR group (n=268) and those in the CR group (n=1,081). Propensity scores were then calculated using a multivariate logistic regression model based on predefined 19 variables. The area under the receiver operating characteristic curve was 0.69 (95% confidence interval, 0.58–0.76; P=0.031). The Hosmer-Lemeshow goodness for this model was 14.112 (P=0.713). Using matching propensity scores, 234 pairs of patients were successfully established in a 1:1 manner. As shown in Figure 1, all the absolute standardized differences after matching were <10%, indicating an adequate balance.
Propensity score matching selected 234 pairs of patients comparable for all baseline variables (as shown in Table 1). Patients in the matched IR group compared with the matched CR group had significantly lower proportions of revascularization of the diagonal artery and left circumflex territory (as presented in Table 2). In addition, patients in the matched IR group received fewer grafts compared to patients in the matched CR group (P<0.001).
In-hospital outcomes
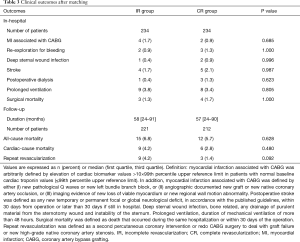
Surgical mortality and major postoperative morbidity are shown in Table 3. Patients in the two matched groups had a similar surgical mortality (1.3% vs. 1.7%, P=1.000). No significant differences between the two matched groups were found for the incidence of major postoperative morbidity.
Full table
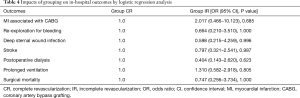
The impacts of grouping (the matched IR group vs. the matched CR group) on surgical mortality and major postoperative morbidity are shown in Table 4. Grouping (IR vs. CR) was not an independent risk factor for surgical mortality or a predictor of major postoperative morbidity in multivariable logistic regression analysis.
Full table
Follow-up outcomes
A total of 433 patients (221 patients in the IR group and 212 patients in the CR group) received a follow-up survey, and the follow-up rate was 92.5%. In the duration of 24 to 91 months follow-up, with the median of 58 months, 27 patients died, and all-cause mortality was 6.2%. No significant differences between the two matched groups were found with regard to all-cause mortality and cardiac-cause mortality (6.8% vs. 5.7%, P=0.628, and 4.2% vs. 2.8%, P=0.480, respectively). Additionally, a total of 12 patients (2.8%) received repeat revascularization at follow-up. All 12 patients preferred to PCI rather than repetition of CABG surgery due to graft failure (6 patients: 4 in the IR group and 2 in the CR group) or disease progressions that were not grafted at the time of the initial surgery (6 patients: 5 in the IR group and 1 in the CR group).
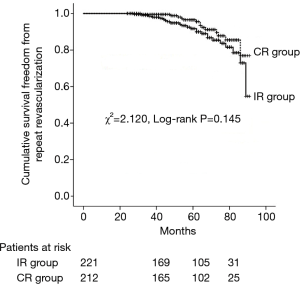
As presented in Table 5, multivariate Cox regression analysis showed that IR was not an independent predictor of cardiac death at follow-up (HR =1.215; 95% CI, 0.883–2.164; P=0.371). As shown in Figure 2, the two matched groups received a similar cumulative survival freedom from repeat revascularization in Kaplan-Meier curves (χ2=2.120, log-rank P=0.145).
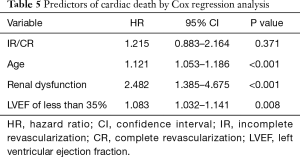
Full table
Discussion
The main findings of the current study were as follows: (I) CR was achieved in the majority of isolated off-pump CABG cases (80.1%); (II) compared with off-pump CR, off-pump IR with the LIMA grafting to the LAD received acceptable in-hospital and mid-term outcomes.
In this cohort of 1,349 consecutive Chinese patients with a triple-vessel lesion undergoing first-time, isolated off-pump CABG, the incidence of off-pump IR was 19.9%, indicating that over 80.0% of patients with a triple-vessel lesion who underwent isolated off-pump CABG received CR. It means that CR could be achieved in the majority of off-pump CABG cases (over 80.0%). It should be emphasized that off-pump IR rate in this cohort was relatively low (19.9%). In a report on the Veterans Affairs Continuous Improvement in Cardiac Surgery Program, involving 41,139 patients with left main and three-vessel lesion, the IR rate among 6,367 off-pump CABG cases was up to 29.0% (22). Recently, Head and colleagues conducted the SYNTAX trial and reported an IR rate of 36.8% (23). The off-pump IR rate in the present study was lower than that in those previous reports. The lower off-pump IR rate in this study may be related to the high proportion of off-pump CABG to all CABG cases during the same period in our institute. More recently, a study involving a total of 7,427 off-pump CABG and 7,128 on-pump CABG cases reported the off-pump IR rate of 13.3% (12), which was below the 19.9% in the current study. The reason for this difference needs to be further explored.
A key finding of this study was that patients in the IR group and in the CR group received similar in-hospital and follow-up outcomes. In our study, univariate analysis showed the two groups had comparable surgical mortality and major postoperative morbidity. Furthermore, multivariable logistic regression analysis revealed that grouping (IR vs. CR) was not an independent risk factor for surgical mortality or a predictor of major postoperative morbidity. Additionally, multivariate Cox regression analysis showed that IR was not an independent predictor of cardiac death at follow-up, and Kaplan-Meier curves showed a similar cumulative survival freedom from repeat revascularization between the two groups. These results suggested that patients with off-pump IR shared similar in-hospital and follow-up outcomes with patients with off-pump CR. The optimal degree of revascularization for patients with triple-vessel lesion remained an unsolved issue. A body of evidence showed that surgical CR compared to surgical IR was associated with reduced adverse cardiovascular events and improved prognosis. However, it has been reported that patients with surgical IR were more likely to present with multiple comorbidities and unfavorable anatomy, and this could bias the data in favor of surgical CR Jeny(24). In recent years, the concept of surgical IR progressed from a suboptimal or a defective treatment towards the most appropriate revascularization technique in some categories of patients (3). Vander Salm and colleagues conducted a RCT study involving 1,507 CABG patients and found no differences in cardiac-related mortality or major adverse cardio-cerebral vascular events for CR compared with IR (8). Rastan and colleagues performed a cohort study involving 8,806 CABG patients and found that complex coronary artery disease was associated with IR, and IR was not related to in-hospital mortality (9). Afterwards, a study conducted by Head and colleagues on 870 CABG patients reported that no differences emerged between the IR group and the CR group in terms of major adverse cardio-cerebral vascular events (23). Another RCT study conducted by Milojevic reported that surgical IR did not increase the risk of death or cardiac adverse events during a median follow-up period of 5 years (10). The present study indicated that patients in the IR group and in the CR group received similar short-term and follow-up outcomes. Our results were consistent with these previous studies. Grafting of the LIMA to the LAD has been proven to be of paramount importance to surgical revascularization and is the most effective strategy, and it has excellent clinical outcomes. The BARI trial supported the hypothesis that grafting more than one target other than the LAD did not confer any long-term advantage and was associated with an increased mortality risk (8). In a large cohort study, Rastan et al. indicated that in the presence of LIMA-LAD graft, reasonable surgical IR of the circumflex or right coronary artery territory did not adversely affect early or long-term survival in patients with multivessel lesions (9). These evidence suggested that LIMA grafting to the LAD may determine survival rate, independent of the presence of other grafts. In this study, all selected patients received LIMA grafting to the LAD, with additional conduits grafting to other target vessels. A well-functioning LIMA-LAD improved survival in patients with multivessel lesions and was an established tenant of practice (25). Therefore, off-pump IR with LIMA grafting to the LAD may be an appropriate revascularization strategy in some categories of patients. This study stressed, once again, the importance of LIMA grafting to the LAD in surgical revascularization.
In this study, the IR group compared with the CR group had a higher proportion of high SYNTAX score (score of 33 or more), suggesting that patients with off-pump IR were more likely to present with severely or diffusely diseased coronary arteries or small coronary arteries. It meant that patients with triple-vessel lesion and high SYNTAX scores were more likely to receive IR during off-pump CABG. This study also showed that the diagonal arteries and circumflex territories were more likely to remain ungrafted in the IR group compared with the CR group, suggesting that target vessels of left ventricular lateral wall were less likely to be revascularized during off-pump CABG. This may be related to unstable hemodynamics during off-pump CABG due to lack of good presentation of the target arteries on the lateral aspect of the heart without cardiopulmonary bypass support.
The strategy of IR with the LIMA grafting to the LAD may be an attractive alternative. However, it did not translate into surgical IR as a preferred strategy relative to surgical CR. The strategy of off-pump IR with the LIMA grafting to the LAD may be a relatively favorable choice when it is more difficult to achieve surgical CR. This category contained patients with severely diffuse lesions or patients without enough conduits to allow revascularization of all potential target vessels. Elderly patients, especially elderly female patients, with concomitant reduced functional capacity and increased comorbid conditions may be suitable candidates. In the real-life surgical scenario, decision-making regarding which target to graft was often driven by the subjective evaluation of the surgeon, of the caliber of the vessel and of the additional intraoperative risk to obtain a CR of targets which were originally considered adequate (>1.5 mm) on the basis of an angiogram (3). During surgery, a vessel was not grafted if it was small and had a poor runoff, as assessed by the surgeon while observing and feeling the vessels (1).
This study had some potential limitations. First, despite using propensity score matching, it was only a single-center observational study involving a small sample size, which may influence the generalizability of its results. A multi-center study with a larger sample size would be required before final confirmation. Second, in our institute, off-pump CABG surgery has been the first choice for patients who were referred for surgical revascularization, and the proportion of off-pump CABG to all CABG cases during the same period was over 70.0%. Therefore, our results may not be in line with evidence from medical centers with low proportion of off-pump to all CABG cases or for surgeons in their learning curve period. In addition, our results might be true only for cardiac surgeons and anesthesiologists who were fully accustomed to the off-pump CABG. Third, the definition of surgical IR itself could have been a confounding factor. Different definitions of IR have been used in studies regarding the incompleteness of surgical revascularization. In this study, IR was defined as any diseased coronary system with vessel size ≥1.5 mm with at least one significant diameter stenosis >50% failing to receive a graft, which was used in the majority of previous studies (1,17). Some patients in the IR group in this study might have been allocated to the CR group or vice versa if other definitions had been used. Unfortunately, surgical revascularization is still mainly driven by an “anatomy-based strategy” (26,27), and fractional flow reserve guided revascularization is not routinely used. Therefore, it is very difficult to know if the smaller caliber vessels normally left ungrafted during surgery are actually not functionally significant, and if this might partially justify the difference in event-free survival. Finally, the duration of follow-up was relatively short. A longer observation period was needed to confirm our findings.
Conclusions
CR may be achieved in the majority of off-pump CABG cases (over 80%). Compared with off-pump CR, off-pump IR with the LIMA grafting to the LAD was associated with acceptable in-hospital and mid-term outcomes.
Acknowledgements
The authors would like to thank The American Journal Experts Team for the linguistic revision of the manuscript.
Funding: This study was supported by the Science and Technology Commission of Shanghai Municipality (Project Number: 14411967100), National Natural Science Foundation of China (No. 81771971) and Shanghai Pujiang Program (17PJ1401500).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study protocol was approved by the ethics committee of Zhongshan Hospital Fudan University (No. Y2017-049) and was consistent with the Declaration of Helsinki.
References
- Garcia S, Sandoval Y, Roukoz H, et al. Outcomes after complete versus incomplete revascularization of patients with multivessel coronary artery disease: a meta-analysis of 89,883 patients enrolled in randomized clinical trials and observational studies. J Am Coll Cardiol 2013;62:1421-31. [Crossref] [PubMed]
- Tsujita K, Yamanaga K, Kaikita K, et al. How should we treat myocardial infarction patients with multivessel disease? – Staged revascularization? Or stent them all acutely? Circ J 2016;80:318-20. [Crossref] [PubMed]
- Spadaccio C, Nappi F, Nenna A, et al. Is it time to change how we think about incomplete coronary revascularization? Int J Cardiol 2016;224:295-8. [Crossref] [PubMed]
- Schwann TA, Yammine MB, El-Hage-Sleiman AM, et al. The effect of completeness of revascularization during CABG with single versus multiple arterial grafts. J Card Surg 2018;33:620-8. [Crossref] [PubMed]
- Généreux P, Palmerini T, Caixeta A, et al. Quantification and impact of untreated coronary artery disease after percutaneous coronary intervention: the residual SYNTAX (Synergy Between PCI with Taxus and Cardiac Surgery) score. J Am Coll Cardiol 2012;59:2165-74. [Crossref] [PubMed]
- Farooq V, Serruys PW, Bourantas CV, et al. Quantification of incomplete revascularization and its association with five-year mortality in the synergy between percutaneous coronary intervention with taxus and cardiac surgery (SYNTAX) trial validation of the residual SYNTAX score. Circulation 2013;128:141-51. [Crossref] [PubMed]
- Dauerman HL. Reasonable incomplete revascularization. Circulation 2011;123:2337-40. [Crossref] [PubMed]
- Vander Salm TJ, Kip KE, Jones RH, et al. What constitutes optimal surgical revascularization? Answers from the Bypass Angioplasty Revascularization Investigation (BARI). J Am Coll Cardiol 2002;39:565-72. [Crossref] [PubMed]
- Rastan AJ, Walther T, Falk V, et al. Does reasonable incomplete surgical revascularization affect early or long-term survival in patients with multivessel coronary artery disease receiving left internal mammary artery bypass to left anterior descending artery? Circulation 2009;120:S70-7. [Crossref] [PubMed]
- Milojevic M, Head SJ, Parasca CA, et al. Causes of death following PCI versus CABG in complex CAD: 5-year follow-up of SYNTAX. J Am Coll Cardiol 2016;67:42-55. [Crossref] [PubMed]
- Benedetto U, Gaudino M, Di Franco A, et al. Incomplete revascularization and long-term survival after coronary artery bypass surgery. Int J Cardiol 2018;254:59-63. [Crossref] [PubMed]
- Benedetto U, Caputo M, Patel NN, et al. Long-term survival after off-pump versus on-pump coronary artery bypass graft surgery. Does completeness of revascularization play a role? Int J Cardiol 2017;246:32-6. [Crossref] [PubMed]
- Puskas JD, Williams WH, Duke PG, et al. Off-pump coronary bypass grafting provides complete revascularization with reduced myocardial injury, transfusion requirements, and length of stay: a prospective randomized comparison of two hundred unselected patients undergoing off-pump versus conventional coronary artery bypass grafting. J Thorac Cardiovasc Surg 2003;125:797-808. [Crossref] [PubMed]
- van Dijk D, Spoor M, Hijman R, et al. Cognitive and cardiac outcomes 5 years after off-pump vs on-pump coronary artery bypass graft surgery. JAMA 2007;297:701-8. [Crossref] [PubMed]
- Chikwe J, Lee T, Itagaki S, et al. Long-term outcomes after off-pump versus on-pump coronary artery bypass grafting by experienced surgeons. J Am Coll Cardiol 2018;72:1478-86. [Crossref] [PubMed]
- Bakaeen FG, Chu D, Kelly RF, et al. Performing coronary artery bypass grafting off-pump may compromise long-term survival in a veteran population. Ann Thorac Surg 2013;95:1952-8; discussion 1959-60.
- Kereiakes DJ. Complete revascularization: a quality-performance metric? J Am Coll Cardiol 2013;62:1432-5. [Crossref] [PubMed]
- Xia L, Ji Q, Song K, et al. Early clinical outcomes of on-pump beating-heart versus off-pump technique for surgical revascularization in patients with severe left ventricular dysfunction: the experience of a single center. J Cardiothorac Surg 2017;12:11. [Crossref] [PubMed]
- Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularization in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart 2010;96:662-7. [Crossref] [PubMed]
- Ji Q, Shi Y, Xia L, et al. Revascularization of left coronary system using a skeletonized left internal mammary artery - sequential vs. separate grafting. Circ J 2017;82:102-9. [Crossref] [PubMed]
- Ji Q, Lai H, Sun Y, et al. Impact of presurgical mild acute respiratory distress syndrome on surgical mortality after surgical repair of acute type A aortic dissection. Int Heart J 2017;58:739-45. [Crossref] [PubMed]
- Omer S, Cornwell LD, Rosengart TK, et al. Completeness of coronary revascularization and survival: Impact of age and off-pump surgery. J Thorac Cardiovasc Surg 2014;148:1307-15.e1. [Crossref] [PubMed]
- Head SJ, Mack MJ, Holmes DR Jr, et al. Incidence, predictors and outcomes of incomplete revascularization after percutaneous coronary intervention and coronary artery bypass grafting: a subgroup analysis of 3-year SYNTAX data. Eur J Cardiothorac Surg 2012;41:535-41. [Crossref] [PubMed]
- Leviner DB, Torregrossa G, Puskas JD. Incomplete revascularization: what the surgeon needs to know. Ann Cardiothorac Surg 2018;7:463-9. [Crossref] [PubMed]
- Milojevic M, Head SJ, Holmes DR Jr. Reply: Incomplete revascularization in PCI and CABG: When two plus two does not make four. J Am Coll Cardiol 2016;68:878-9. [Crossref] [PubMed]
- Ferguson TB Jr, Chen C, Babb JD, et al. Fractional flow reserve-guided coronary artery bypass grafting: can intraoperative physiologic imaging guide decision making? J Thorac Cardiovasc Surg 2013;146:824-35.e1. [Crossref] [PubMed]
- Ferguson TB Jr, Chen C, Buch AN. Fractional flow reserve-guided coronary bypass surgery: should surgeons use it? Curr Opin Cardiol 2013;28:654-60. [Crossref] [PubMed]


