
Video-assisted thoracoscopic surgery for ectopic mediastinal parathyroid tumor: subxiphoid and lateral thoracic approach
Introduction
Ectopic mediastinal parathyroid tumor, which is one of the causes of primary hyperparathyroidism, accounts for 0.9% of all mediastinal tumors (1). Surgical approaches for mediastinal tumors include median sternotomy, lateral thoracotomy, mediastinoscopy, manubriotomy, transcervical incision, and thoracoscopic surgery using the lateral and subxiphoid approaches. Currently, thoracoscopic surgery using the lateral thoracic approach is the most common procedures (2-8). We have been performing multi-port mediastinal tumor resection using the lateral thoracic approach since 2008 and single-port mediastinal tumor resection using the subxiphoid approach since 2011 for mediastinal tumors (9). This study aimed to investigate the initial results of an endoscopic surgical approach for the treatment of intramediastinal ectopic parathyroid adenoma and to evaluate the effectiveness of a single-incision resection using the subxiphoid approach.
Methods
A total of 265 patients with mediastinal tumor underwent thoracoscopic surgery using the lateral or subxiphoid approach from 2008 to 2017 in Fujita Health University Hospital. Five (1.89%) of 265 patients who were diagnosed with ectopic mediastinal parathyroid tumor were included in the study and were retrospectively analyzed.
We examined the presence or absence of preoperative clinical symptoms, preoperative chest contrast-enhanced computed tomography findings, preoperative 99mTc-methoxyisobutylisonitrile scintigraphy (99mTc-MIBI scintigraphy) results, pre- and postoperative serum calcium, phosphorous, and intact-PTH hormone levels, operative time, the amount of intraoperative blood loss, the rate of conversion to thoracotomy, intra- and postoperative complications, the amount of postoperative oral analgesics, the administration period of postoperative oral analgesic, the duration of chest tube drainage, the length of hospital stay and pathological examination findings. Data were presented as mean values ± standard deviation. This study was approved by the Institutional Review Board of Fujita Health University (No. HM18-194).
Surgical technique
The operations were performed under general anesthesia. A single-lumen endotracheal tube was used for single-port mediastinal tumor resection using the subxiphoid approach and a double-lumen endotracheal tube for multi-port mediastinal tumor resection using the lateral thoracic approach. It has been reported that seeding of parathyroid adenomas can easily occur (10). Therefore, when performing thymectomy for tumors that had developed in the thymus, we resected the tumors en bloc with surrounding fatty tissues and ensured the actual tumor was not touched. The resected tumors were placed in a bag in the thoracic cavity and removed from the surgical wound.
The multi-port mediastinal tumor resection using the lateral thoracic approach was performed with the patient in lateral decubitus position. The operation was performed using three ports. Skin incisions of 1.5 cm were made in the third intercostal space along the middle axillary line, the fifth intercostal space along the anterior axillary line, and the seventh intercostal space along the posterior axillary line.
We performed single-port mediastinal tumor resection using the subxiphoid approach with the same techniques that we previously reported for thymectomy (9). The patient was placed in supine position with legs open. A 3-cm transverse incision was made 1 cm caudally from the xiphoid process. GelPOINT®Mini (Applied Medical Resources Co., Rancho Santa Margarita, CA, USA) was inserted at the incision site, and three subports were inserted into the GelPOINT®Mini platform. A camera scope and forceps were inserted into the three subports, and the operation was performed.
CO2 insufflation of the mediastinum was performed at 8 mmHg. Both sides of the mediastinal pleura were transected to open both sides of the thoracic cavity. The left and right phrenic nerves were then identified and separated from the pericardium, including the anterior mediastinal pleura, thymus, and surrounding fatty tissue. The cervical region of the thymus was separated at the cranial side from the thyroid gland, on the right side from the right brachiocephalic vein, on the left side from the innominate vein, and on the dorsal side from the brachiocephalic artery and trachea. Finally, the thymus was pulled to either the left or right side. The thymic vein was transected, and the ectopic mediastinal parathyroid tumor with the thymus was removed (Figure 1).

Results
Table 1 summarizes the characteristics of the 5 patients (mean age: 50.6±14.79 years; 1 male and 4 females) with ectopic mediastinal parathyroid tumor who underwent thoracoscopic surgery. Four patients presented with the following symptoms prior to surgery: weight loss, poor appetite, fatigue, knee pain, lower back pain, pain in the right abdominal region, hematuria, and facial edema. The tumor was located at two sites (superior and anterior mediastinum) in 1 patient, in the superior mediastinum in 1, in the anterior mediastinum in 2, and in the middle mediastinum in 1. Imaging revealed a mean tumor diameter of 1.83±0.85 cm. Preoperative 99mTc-MIBI scintigraphy was performed in all patients. While uptake in the tumor was confirmed in 4 patients, only a slight uptake was noted in 1 patient. Serum calcium, phosphorous, and intact-PTH hormone levels were measured via preoperative blood testing. Hypercalcemia was observed in 4 patients, with serum calcium levels measured at 10.56±1.52 mg/dL. Hypophosphatemia was observed in 1 patient, with serum phosphorous levels measured at 2.84±0.42 mg/dL. Intact-PTH hormone levels were elevated at 221±169.84 pg/dL in all patients.
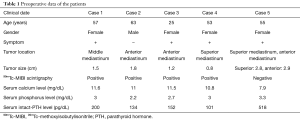
Full table
Table 2 summarizes the intra- and postoperative findings. Single-port mediastinal tumor resection using the subxiphoid approach was performed in 4 patients, whereas multi-port mediastinal tumor resection using the lateral thoracic approach was performed in 1 patient. The total operative time was 134±83.52 min, and the amount of blood loss was 81.8±173.41 mL. In multi-port mediastinal tumor resection using the lateral thoracic approach, the operative time was 255 min, and the amount of blood loss was 392 mL. Meanwhile, in single-port mediastinal tumor resection using the subxiphoid approach, the operative time was 103.75±56.56 min, and the amount of blood loss was 4.25±1.5 mL. In one patient who underwent multi-port mediastinal tumor resection using the lateral thoracic approach and a different operation at another hospital, left lung was completely adherent to the thoracic cavity. Therefore, the operative time was longer, and a higher amount of blood loss was observed. The conversion to thoracotomy intraoperatively and intraoperative complications was not observed in any patient.
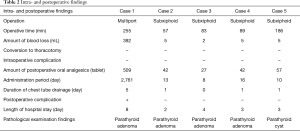
Full table
The amount of postoperative oral analgesics was 135.4±209.12 tablets, and their administration period was 561.6±1,229.5 days. In multi-port mediastinal tumor resection using the lateral thoracic approach, 509 tablets were used, and the administration period was 2,761 days. Conversely, in single-port mediastinal tumor resection using the subxiphoid approach, 42±12.25 tablets were used, and the administration period was 11.75±3.5 days. While no postoperative pain (12) was observed in cases 2 through 5, 1 patient who underwent surgery using the lateral thoracic approach reported postoperative pain. After 7.5 years from operation, the patient still experiences pain.
The duration of chest tube drainage was 1.6±1.95 days, and the length of hospital stay was 4±2.35 days. In multi-port mediastinal tumor resection using the lateral thoracic approach, the duration of chest tube drainage was 5 days, and the length of hospital stay was 8 days. Conversely, in single-port mediastinal tumor resection using the subxiphoid approach, the duration of chest tube drainage was 5 days, and the length of hospital stay was 0.75±0.5 and 3±0.82 days. Pathological examination findings indicated parathyroid adenoma in 4 patients and parathyroid cyst in 1 patient.
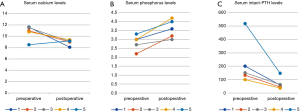
Figure 2 summarizes the pre- and postoperative serum calcium, phosphorous, and intact-PTH hormone levels in all patients. These levels improved postoperatively in all patients. Serum calcium levels decreased from 10.56±1.52 mg/dL preoperatively to 8.96±0.5 mg/dL postoperatively, and serum phosphorous levels increased from 2.84±0.42 mg/dL preoperatively to 3.6±0.51 mg/dL postoperatively. Moreover, intact-PTH hormone levels decreased from 221±169.84 pg/dL preoperatively to 70.2±44.28 pg/dL postoperatively. Recurrence was not observed in any of the cases.
Discussion
Parathyroid adenomas are the most common causes of primary hyperparathyroidism. While most of these adenomas develop near the thyroid gland, 16% are ectopic and develop in sites such as the mediastinum, pharynx, back surface of the esophagus, near the aortic arch, or around the pericardium (13,14). The frequency of parathyroid adenoma arising from a mediastinal tumor is 0.9%.
Approximately 67–80% of ectopic mediastinal parathyroid tumors are located in the thymus (15,16). In 4 patients in our study, the tumor was located in the thymus. Approaches to the thymus include median sternotomy, lateral thoracic thoracotomy, mediastinoscopy, manubriotomy, cervical collar incision, and thoracoscopic surgeries using the lateral and subxiphoid approaches. Recently, thoracoscopic surgery using the lateral thoracic approach has become the primary option for minimally invasive surgery (2-8). However, intercostal neuralgia is a common complication associated with thoracoscopic surgery performed using the lateral thoracic approach (12). While we performed multi-port mediastinal tumor resection using the lateral thoracic approach for mediastinal tumors from 2008 to 2010, we started using the single-port mediastinal tumor resection using the subxiphoid approach for such cases in 2011 (9). Because single-port mediastinal tumor resection using the subxiphoid approach does not require an intercostal approach, procedures such as thoracoscopic surgery do not cause intercostal neuralgia from the lateral thoracic region, which is considered its advantage (17). In fact, a study comparing postoperative pain in an intercostal thoracoscopic surgery group and a subxiphoid surgery group found that visual analog scale scores were significantly lower in the subxiphoid surgery group than in the intercostal thoracoscopic surgery group (18). In our study, while the postoperative oral analgesics were not necessary on postoperative day 16 for patients who underwent single-port mediastinal tumor resection using the subxiphoid approach, the patient who underwent multi-port mediastinal tumor resection using the lateral thoracic approach presented with postoperative pain and required long-term administration of oral analgesics. The case of the lateral thoracic approach in our study can not be compared with the subxiphoid approach for postoperative pain, because there was a history of ipsilateral surgery in another hospital, and the left lung was completely adherent to the thoracic cavity. However, the single-incision mediastinal tumor resection via the subxiphoid approach, without going through the intercostal space, is a very useful approach for patients in terms of postoperative pain (17). Due to the fact that it is a single-port approach, it has advantages in terms of cosmetics (19). A study comparing single-incision thoracoscopic surgery and three port video-assisted thoracic surgery in terms of patient satisfaction with the wound site has reported that patient satisfaction with single-incision thoracoscopic surgery was significantly higher (20).
No significant differences were noted between the procedures in terms of the duration of chest tube drainage or length of hospital stay. Amer et al. have reported that the duration of chest tube drainage and length of hospital stay in three port video-assisted thoracoscopic surgery for ectopic mediastinal parathyroid tumor were 1±0.57 and 2±2.36 days, respectively (21). Thus, no significant differences were noted in terms of the duration of chest tube drainage and length of hospital stay in single-port mediastinal tumor resection using the subxiphoid approach.
When treating parathyroid adenomas, postoperative metastasis and subsequent recurrence can easily occur as a result of intraoperative damage to the tumor capsule (10,22). Rattner et al. have reported that extreme caution is required during surgery to prevent such metastasis and damage to the capsule or touching the parathyroid tissue (10). Moreover, Akerström et al. have reported that in addition to performing intraoperative procedures with caution, surgeons must not divide the parathyroid gland in the surgical field (22). Thymectomy is not required for patients with ectopic mediastinal parathyroid tumor. However, if sufficient tumor margins cannot be secured or if the tumor is close to the innominate vein and the site of this vein must be confirmed to safely perform surgery, thymectomy may be performed. In all the 5 patients in our study, the thymus was completely resected without grasping the tumor or area around it intraoperatively, thereby preventing damage in the tumor capsule. Taking this into consideration, we believe that any recurrence of hyperparathyroidism was postoperatively prevented.
Conclusions
We performed thoracoscopic surgery in patients with ectopic mediastinal parathyroid tumor and obtained satisfactory results in terms of postoperative pain and cosmetic outcomes. Single-port mediastinal tumor resection using the subxiphoid approach did not result in postoperative pain in 4 patients. However, 1 patient who underwent multi-port mediastinal tumor resection using the lateral thoracic approach reported postoperative pain. The single-incision mediastinal tumor resection via the subxiphoid approach, without going through the intercostal space, is considered as a useful endoscopic surgical approach for the treatment of mediastinal ectopic parathyroid adenomas due to the limited occurrence of post-thoracotomy pain syndrome and the superior esthetic outcomes associated with the procedure as compared to thoracotomy and median sternotomy.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was approved by the Institutional Review Board of Fujita Health University (No. HM18-194).
References
- Matsushima S, Kawamoto M, Iedokoro Y, et al. The assessment of surgical therapy on the mediastinal tumors treated in our department. J Jpn Surg Assoc 1991;52:960-5.
- Du H, Shi M, Zhu L, et al. Comparison of video-assisted thoracic surgery with open surgery in the treatment of ectopic mediastinal parathyroid tumors. J Thorac Dis 2017;9:5171-5. [Crossref] [PubMed]
- Said SM, Cassivi SD, Allen MS, et al. Minimally Invasive Resection for Mediastinal Ectopic Parathyroid Glands. Ann Thorac Surg 2013;96:1229-33. [Crossref] [PubMed]
- Tcherveniakov P, Menon A, Milton R, et al. Video-assisted mediastinoscopy (VAM) for surgical resection of ectopic parathyroid adenoma. J Cardiothorac Surg 2007;2:41. [Crossref] [PubMed]
- Nilubol N, Beyer T, Prinz RA, et al. Mediastinal hyperfunctioning parathyroids: incidence, evolving treatment, and outcome. Am J Surg 2007;194:53-6. [Crossref] [PubMed]
- Wang X, Zhu YM, Huang H, et al. Surgery for Ectopic Parathyroid Adenoma in Lower Part of Superior Mediastinum through a Transcervical Incision. Chin Med J 2017;130:1376-7. [Crossref] [PubMed]
- Fatimi SH, Inam H, Chagan FK, et al. Management of mediastinal parathyroid adenoma via minimally invasive thoracoscopic surgery: Case report. Int J Surg Case Rep 2017;40:120-3. [Crossref] [PubMed]
- Ismail M, Maza S, Swierzy M, et al. Resection of ectopic mediastinal parathyroid glands with the da Vinci® robotic system. Br J Surg 2010;97:337-43. [Crossref] [PubMed]
- Suda T, Sugimura H, Tochii D, et al. Single-Port Thymectomy Through an Infrasternal Approach. Ann Thorac Surg 2012;93:334-6. [Crossref] [PubMed]
- Rattner DW, Marrone GC, Kasdon E, et al. Recurrent hyperparathyroidism due to implantation of parathyroid tissue. Am J Surg 1985;149:745-8. [Crossref] [PubMed]
- Nagano H, Suda T, Ishizawa H, et al. Single-port mediastinal tumor using the subxiphoid approach. Asvide 2019;6:204. Available online: http://www.asvide.com/watch/32887
- Miyazaki T, Sakai T, Tsuchiya T, et al. Assessment and follow-up of intercostal nerve damage after video-assisted thoracic surgery. Eur J Cardiothorac Surg 2011;39:1033-9. [Crossref] [PubMed]
- Maeshiro K, Ono R, Akamine K, et al. Video-assisted thoracoscopic removal of an ectopic mediastinal parathyroid adenoma on co2 insufflation. J Jpn Surg Assoc 2016;77:1347-52. [Crossref]
- Phitayakorn R, McHenry CR. Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 2006;191:418-23. [Crossref] [PubMed]
- Wang C, Gaz RD, Moncure AC. Mediastinal Parathyroid Exploration: A Clinical and Pathologic Study of 47 Cases. World J Surg 1986;10:687-95. [Crossref] [PubMed]
- Norton JA, Schneider PD, Brennan MF. Median Sternotomy in Reoperations for Primary Hyperparathyroidism. World J Surg 1985;9:807-13. [Crossref] [PubMed]
- Suda T, Hachimaru A, Tochii D, et al. Video-assisted thoracoscopic thymectomy versus subxiphoid single-port thymectomy: initial results. Eur J Cardiothorac Surg 2016;49:i54-8. [PubMed]
- Wang BY, Chang YC, Chang YC, et al. Thoracoscopic surgery via a single-incision subxiphoid approach is associated with less postoperative pain than single-incision transthoracic or three-incision transthoracic approaches for spontaneous pneumothorax. J Thorac Dis 2016;8:S272-8. [PubMed]
- Kido T, Hazama K, Inoue Y, et al. Resection of Anterior Mediastinal Masses Through an Infrasternal Approach. Ann Thorac Surg 1999;67:263-5. [Crossref] [PubMed]
- Yang HC, Cho S, Jheon S. Single-incision thoracoscopic surgery for spontaneous pneumothorax using the SILS port compared with conventional three-port surgery. Surg Endosc 2013;27:139-45. [Crossref] [PubMed]
- Amer K, Khan AZ, Rew D, et al. Video assisted thoracoscopic excision of mediastinal ectopic parathyroid adenomas: a UK regional experience. Ann Cardiothorac Surg 2015;4:527-34. [PubMed]
- Akerström G, Rudberg C, Grimelius L, et al. Recurrent hyperparathyroidism due to peroperative seeding of neoplastic or hyperplastic parathyroid tissue. Acta Chir Scand 1988;154:549-52. [PubMed]


