
Does one year change in quality of life predict the mortality in patients with chronic obstructive pulmonary disease?—Prospective cohort study
Introduction
Chronic obstructive pulmonary disease (COPD) is a leading cause of morbidity and mortality worldwide resulting in a significant economic and social burden. By 2020, COPD is estimated to become the fifth most common cause of morbidity and the third most common cause of death worldwide (1). Factors related with COPD mortality are depressive symptoms (2), smoking (3), comorbidity (3), age and inspiratory capacity (4), PaO2 (3,4), low forced expiratory volume in 1 second (FEV1) (4), increased body mass index (BMI) (4,5) and health-related quality of life (HRQoL) scores (6).
Health status measurement is becoming an important issue for the day-to-day management of COPD patients in both primary and secondary health care (7,8). Studies report that a shorter survival is related to worse HRQoL (9-11). A poor HRQoL also has been shown to be associated with high levels of dyspnea (12), physical impairment (13), depression and anxiety (12), a poor prognosis in terms of readmission to hospital (14) and death (9). Since health status is considered a major goal in managing the COPD.
The objective of this study was to evaluate whether an improvement in QoL after 1 year of proper management is a predictor of survival in a cohort of patients followed up for 10 years.
Methods
Subjects
COPD patients were assessed for eligibility between January 2003 and September 2003 in our clinic (Figure 1).
Eligible subjects were older than 40 years old with an established COPD history (minimum one year from diagnosis), chronic airflow impairment (percentage of FEV1 <80% and FEV1/FVC <0.7), with a change in FEV1 less than 200 mL and 15% in the bronchodilator test, smoking history more than 20 pack-years, no history suggestive of asthma, no exacerbation of airflow limitation in the preceding six weeks, no changes in treatment regimen preceding four weeks, and QoL questionnaire completion.
Study design
The study was prospective, observational, cohort study and follow up time after first year assessment was 10 years. The following data were assessed for all patients included: social demographical findings, medical history, lung function measurements, BMI and QoL questionnaire.
Medical history including the medical treatment of COPD, long term oxygen use, comorbid conditions, smoking status, number of COPD exacerbation, emergency room visits and hospitalization were recorded. Pulmonary function test (PFT) was performed by using the Jaeger Master Screen Pneumo by the same technical person. Spirometric parameters, FEV1, forced vital capacity (FVC), vital capacity (VC), FEV1/FVC, and peak expiratory flow (PEF) were measured. Patients were classified according to GOLD 2014 as stage 1 (FEV1 >70%), stage 2 (70%> FEV1 >50%), stage 3 (50%> FEV1 >30%), and stage 4 (FEV1 <30%). PFT was performed at the beginning of study and at the first year of the study.
Turkish translation of St. George Respiratory Questionnaire (SGRQ) was used for the assessment of HRQoL. SGRQ is a disease specific QoL assessment tool validated in both COPD and asthma (15-17). The questionnaire has four domains; symptoms, impacts, activities, and a total score. Overall scores range from 0 (no effect on QoL) to a maximum score of 100 (maximum perceived distress); thus, higher score means a poorer QoL. SGRQ was applied to patients at the beginning and at the first year of study and difference between two measurements was calculated.
Primary outcome of the study was mortality. It was obtained from hospital records and direct family interviews. Also the exitus day and reason of mortality were recorded. Reason of mortality was classified as respiratory and nonrespiratory.
Results are expressed as mean ± SD, median (25th percentile–75th percentile), or as percentages in the corresponding categories. Deaths are classified as due to respiratory or nonrespiratory. Baseline differences of patients according to their vital status will be tested using the Fisher exact test for proportions, T-test or Mann-Whitney U test, as appropriate. The Kaplan-Meier survival curves and long-rank tests will be performed after stratifying by tertiles of baseline SGRQ scores. Semiparametric Cox models will be used to assess the association between baseline SGRQ total score and survival time. Cox regression analysis for baseline QoL scores and 1 year change in QoL was performed. Statistical significance is accepted at P<0.05. The study was approved by local ethics committee (Celal Bayar University Medical Faculty Ethical Committee, approval number 1205) and all patients gave their informed consent to participate in the study.
Results
In this prospective, cohort study, 306 COPD patients were assessed for eligibility between January 2003 and September 2003. Two hundred and fifty one patients with COPD as defined by ATS criteria were included but 233 patients were analyzed at the end of the study. At the beginning, 208 patients (89.27%) were male and mean age was 65.55±8.82 years (43–82 years). There were 92 patients (39.5%) in stage 2, 125 patients (53.6%) in stage 3, and 16 patients (6.9%) in stage 4. Mean duration of disease was 7.0±5.0 years. Mean SGRQ scores, namely, activity, symptom, impact, and total were 58.6±17.2, 57.2±13.9 42.7±16.6, and 48.9±15.4, respectively. One hundred and forty six (62.66%) patients had died by the end of the 10-year follow-up.
Baseline characteristics of patients according to alive and dead status are shown in Table 1. Subjects who died during follow-up were more likely to be current-smoker, and had lower BMI. There were no differences according to disease duration, usage of inhaled corticosteroid therapy and long-term oxygen therapy. HRQoL was found worse in patients who were died during follow up.
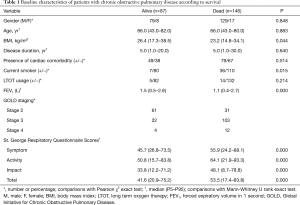
Full table
Of 146 deaths, 85 were due to respiratory cause. Baseline characteristics of dead patients according to reason as respiratory or nonrespiratory were shown in Table 2. The patients died due to nonrespiratory reason were older and had more cardiac comorbidity. There were no differences according to SGRQ scores and FEV1 in both groups.
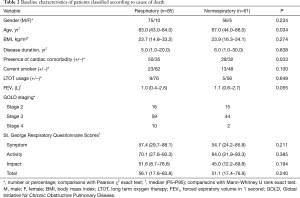
Full table
Change in QoL in a year is more effective than baseline assessment to predict either respiratory or any cause mortality among patients with COPD (Table 3).
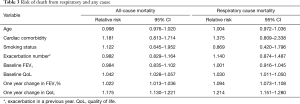
Full table
Discussion
We found that a QoL worsening in the initial year of follow up more strongly predicts 10-year mortality of any cause and respiratory comparing the baseline assessment alone among patients with COPD. The predictive value of baseline assessment of QoL for all-cause mortality was higher than respiratory cause mortality but a QoL worsening in the initial year was more powerful to predict mortality in respiratory cause mortality than all-cause mortality. SGRQ total score was more predictive than other SGRQ scores in all-cause mortality because the comorbidities especially cardiac comorbidities cause COPD like symptoms. In contrast to this, change in SGRQ total score in a year was more useful in estimating the mortality in respiratory cause deaths. Our results provide a different picture by showing that change in HRQoL were consistently associated with mortality. This association was stronger with respiratory than all-cause mortality
Demographic data of the study population are much like in line with recently reported studies with a mean age of 65.55±8.82 years. The demographic profile of the study sample represents a typical COPD stages, most of stage 2 and 3. The mortality rate end of the study was 58.2%. This is relatively high mortality rate when compared to other studies (2,4,6,9,10). Higher mortality rate can be due to the patients who had higher comorbidity especially cardiac and the follow up time was longer.
Many studies investigated the mortality related factors in patients with COPD. The deaths were found to be related with worse lung function, greater age, lower BMI and poorer HRQoL (9). Also more complicated measures like modified BODE index, exercise stress test, and 6-minute walk test were found higher predictors of mortality (18). In our study, non-survived patients were current smoker and had lower BMI, worse lung function, and poorer QoL measured by the SGRQ. Most of mortality (58.2%) over this period was due to respiratory related causes. Patients who were died due to respiratory reasons during follow up period were younger and had more cardiac comorbidity. Lung function and QoL scores were not found different in patient with death due to respiratory or nonrespiratory reasons.
Improvement of health status in COPD patients is one of the key treatment goals according to GOLD management guidelines (19). The SGRQ measurement is known to be a valuable means of consistently assessing deteriorating health status in patients with moderate to very severe COPD (20) and, while several studies have reported the disease specific SGRQ (9) as a being predictive of mortality in COPD (16,21-23). Also in our study SGRQ scores was found to be associated with mortality. Although health status deterioration in COPD over 3–5 years has been previously demonstrated using the SGRQ (20,24) or the CRQ (20,25) to our knowledge this is the longest study to follow it over 10 years. The present study shows that health status continues to deteriorate and degree of this deterioration was more powerful.
There has recently been some debate about the use of FEV1 as the main single evaluative parameter for COPD. Nishimura and coworkers have reported that categorizing patients with COPD on the level of dyspnea was more closely related with mortality than classification based on disease severity, as assessed by the percentage of predicted FEV1 (26). Celli proposed a systemic evaluation of COPD patients and stressed that there is a need to seek candidates for multidimensional disease staging (27). Exercise capacity and health status may also be important clinical indices to evaluate disease impairment in addition to FEV1. Our results showed that HRQoL scores were associated with mortality. After adjustment for BMI, long-term oxygen therapy, inhaled corticosteroid usage, FEV1, change in FEV1, cardiac comorbidity, age, SGRQ scores, change in SGRQ scores, disease duration, smoking status; SGRQ total score, age, cardiac comorbidity, smoking status, change in SGRQ total score, and change in FEV1 were independently associated with all-cause mortality and respiratory cause of mortality.
FEV1 is both the traditional metric used to define the progression of COPD and the strongest spirometric predictor of mortality in COPD patients (28). Although spirometry is traditionally seen as the most important determinator of the diagnosis and severity of COPD, many studies showed that the relation between health status and all spirometric values—mainly FEV1—is weak (29). In our data, FEV1 was not found as a risk factor for mortality in COPD patients but SGRQ total score was related with all cause and respiratory cause mortality but this relation was more significant in all-cause mortality. In the other hand, change in FEV1 in a year was a risk factor in COPD mortality and this was more prominent in patients with death due to respiratory cause. To predict the mortality in patients with COPD, change in FEV1 in a year was found more useful than baseline assessment of SGRQ total score but the change in SGRQ total score in a year most powerful effect to estimate the mortality and in contrast to the baseline assessment this prediction was more powerful in respiratory cause mortality.
There are some limitations to this study. First, at the beginning of the study SGRQ used for determination of HRQoL was not validated for Turkish people for this reason Turkish translation of SGRQ was used. The Turkish version of SGRQ that was used in this study was validated recently by us. Second, few women were included, and the findings here reported cannot be extended to that gender. The lack of more women in the study was not by design, because the opportunity to join the study was offered independent of sex. Also, when we looked the studies done before, most of their patient population was similar to our study. The other limitation of our study was medical records for mortality. Sometimes this record can be misleading. We tried to eliminate this situation by doing conversation with family members also.
In summary our results have shown that a QoL worsening in the initial year of follow up is an independent risk factor of respiratory and all-cause mortality. Up to now, baseline assessment of QoL has been considered a measure to gauge patients with COPD. Our results highlight the importance of change in health related of QoL in the evaluation of disease progression and prediction of mortality in patients with COPD and support the view that change in HRQoL should be considered, in addition to baseline assessment of HRQoL, to more properly assess patients with COPD.
Acknowledgments
We thank A. Sonia Buist, MD, Diana S. M. Buist, PhD; David H. Au MD; Mary Ann McBurnie, PhD for a critical review of the manuscript in MECOR Turkey Course 3/4.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by local ethics committee (Celal Bayar University Medical Faculty Ethical Committee, approval number 1205) and all patients gave their informed consent to participate in the study.
References
- Murray CJL, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: global burden of disease. Lancet 1997;349:1498-504. [Crossref] [PubMed]
- de Voogd JN, Wempe JB, Koëter GH, et al. Depressive symptoms as predictors of mortality in patients with COPD. Chest 2009;135:619-25. [Crossref] [PubMed]
- Nizet TA, van den Elshout FJ, Heijdra YF, et al. Survival of chronic hypercapnic COPD patients is predicted by smoking habits, comorbidity, and hypoxemia. Chest 2005;127:1904-10. [Crossref] [PubMed]
- Tantucci C, Donati P, Nicosia F, et al. Inspiratory capacity predicts mortality in patients with chronic obstructive pulmonary disease. Respir Med 2008;102:613-9. [Crossref] [PubMed]
- Tsimogianni AM, Papiris SA, Stathopoulos GT, et al. Predictors of outcome after exacerbation of chronic obstructive pulmonary disease. J Gen Intern Med 2009;24:1043-8. [Crossref] [PubMed]
- Halpin DM, Peterson S, Larsson TP, et al. Identifying COPD patients at increased risk of mortality: predictive value of clinical study baseline data. Respir Med 2008;102:1615-24. [Crossref] [PubMed]
- Jones PW. Issues concerning health-related quality of life in COPD. Chest 1995;107:187S-193S. [Crossref] [PubMed]
- Jones PW. Health status measurement in chronic obstructive pulmonary disease. Thorax 2001;56:880-7. [Crossref] [PubMed]
- Domingo-Salvany A, Lamarca R, Ferrer M, et al. Health-related quality of life and mortality in male patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:680-5. [Crossref] [PubMed]
- Fan VS, Curtis JR, Tu SP, et al. Using quality of life to predict hospitalization and mortality in patients with obstructive lung diseases. Chest 2002;122:429-36. [Crossref] [PubMed]
- Yorgancioglu A, Havlucu Y, Celik P, et al. Relation between quality of life and morbidity and mortality in COPD patients: Two-year follow-up study. COPD 2010;7:248-53. [Crossref] [PubMed]
- Hajiro T, Nishimura K, Tsukino M, et al. A comparison of the level of dyspnoea vs. disease severity in indicating the health-related quality of life of patients with COPD. Chest 1999;116:1632-7. [Crossref] [PubMed]
- Hu J, Meek P. Health-related quality of life in individuals with chronic obstructive pulmonary disease. Heart Lung 2005;34:415-22. [Crossref] [PubMed]
- Osman IM, Godden DJ, Friend JA, et al. Quality of life and hospital re-admission in patients with chronic obstructive pulmonary disease. Thorax 1997;52:67-71. [Crossref] [PubMed]
- Jones PW. Quality of life measurement for patients with diseases of the airways. Thorax 1991;46:676-82. [Crossref] [PubMed]
- Jones PW, Quirk FH, Baveystock CM. The St George’s Respiratory Questionnaire. Respir Med 1991;85:25-31. [Crossref] [PubMed]
- Polatlı M, Yorgancıoğlu A, Aydemir Ö, et al. Validity and reliability of Turkish version of St. George's respiratory questionnaire. Tuberk Toraks 2013;61:81-7. [Crossref] [PubMed]
- Martinez FJ, Foster G, Curtis JL, et al. Predictors of mortality in patients with emphysema and severe airflow obstruction. Am J Respir Crit Care Med 2006;173:1326-34. [Crossref] [PubMed]
- Pauwels RA, Buist AS, Calverley PM, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001;163:1256-76. [Crossref] [PubMed]
- Oga T, Nishimura K, Tsukino M, et al. Longitudinal deteriorations in patient reported outcomes in patients with COPD. Respir Med 2007;101:146-53. [Crossref] [PubMed]
- Oga T, Nishimura K, Tsukino M, et al. Analysis of the factors related to mortality in chronic obstructive pulmonary disease: role of exercise capacity and health status. Am J Respir Crit Care Med 2003;167:544-9. [Crossref] [PubMed]
- Gudmundsson G, Gislason T, Lindberg E, et al. Mortality in COPD patients discharged from hospital: the role of treatment and co-morbidity. Respir Res 2006;7:109. [Crossref] [PubMed]
- Almagro P, Calbo E, Ochoa de Echaguen A, et al. Mortality after hospitalization for COPD. Chest 2002;121:1441-8. [Crossref] [PubMed]
- Spencer S, Calverley PMA, Burge PS, et al. Health status deterioration in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2001;163:122-8. [Crossref] [PubMed]
- Oga T, Nishimura K, Tsukino M, et al. Longitudinal changes in health status using the Chronic Respiratory Disease Questionnaire and pulmonary function in patients with stable chronic obstructive pulmonary disease. Qual Life Res 2004;13:1109-16. [Crossref] [PubMed]
- Nishimura K, Izumi T, Tsukino M, et al. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 2002;121:1434-40. [Crossref] [PubMed]
- Celli BR. The importance of spirometry in COPD and asthma: effect on approach to management. Chest 2000;117:15S-9S. [Crossref] [PubMed]
- Agustí AG. Systemic effects of chronic obstructive pulmonary disease. Proc Am Thorac Soc 2005;2:367-70; discussion 371-2. [Crossref] [PubMed]
- Tsiligianni I, Kocks J, Tzanakis N, et al. Factors that influence disease-specific quality of life or health status in patients with COPD: a review and meta-analysis of Pearson correlations. Prim Care Respir J 2011;20:257-68. [Crossref] [PubMed]



