Bronchoscopic interventions for severe COPD
Introduction
Chronic obstructive pulmonary disease (COPD) remains one of the most prevalent lung diseases in the world. Medical treatment options are limited and most only provide symptomatic improvements without mortality benefit. To date, supplemental oxygen for hypoxic patients and pulmonary rehabilitation are the only medical treatments that have been shown to improve mortality in severe COPD. Although surgical lung volume reduction (LVR) in severe COPD patients with heterogeneous emphysema has been available for some time, in 2003 a prospective randomized controlled trial clearly demonstrated that in specific patient categories, lung volume reduction surgery (LVRS) was superior to medical management and offered a mortality benefit (1). Despite this, many patients with severe COPD are not candidates for this surgery due to other comorbid conditions. Minimally invasive therapies utilizing bronchoscopy are actively being studied with the ultimate goal of reproducing the advantages seen in surgical LVR with less risk and morbidity from the procedure. The bronchoscopic techniques that have been reported to date include unidirectional bronchial valves, biologic and polymer based techniques to occlude lung segments, small stents placed through airway walls to allow trapped air to exist (airway bypass stents), thermal/steam vapor ablation and endobronchial coils. Each of these techniques attempts to reproduce some of the benefits seen in LVRS with a less invasive and less morbid procedure. In this chapter we will discuss the concepts and limitations for each of these techniques.
Endobronchial one-way valves
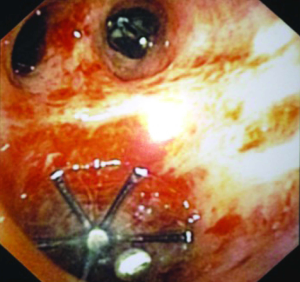
Bronchoscopically placed endobronchial one way valves that occlude airways preventing air from entering severely emphysematous portions of lung yet allow air and mucus to exit have been proposed for the treatment of severe COPD (Figure 1). Initially the hypothesis was that the valves would induce atelectasis of the most severe emphysematous portions of the lung, thus decreasing the air trapping and hyperinflation of the treated lung. Other theoretical methods of action include the shunting or bypassing of severely emphysematous airways directing airflow to the more normal areas of lung to increase ventilation perfusion matching as well as decreasing the dynamic hyperinflation of the lungs during exertion by blocking these severely emphysematous airways. There are currently two types of valves that have been studied. The valves are made by two companies, Spiration Inc. and Pulmonx (previously Emphasys Medical). Both valves are deployed bronchoscopically and are one-way valves. Spiration identifies its valve as an “intrabronchial” valve (IBV) and Pulmonx labels their valve an “endobronchial” valve (EBV) and is also referred to as the Zephyr EBV. The valves have unique designs to achieve the one way valve effect with the IBV being similar to an umbrella design (Figure 2) and the EBV appearing like a fish mouth facing the proximal airways that springs opens when air or mucus is exhaled from the distal airways but stays closed during all other times.
Zephyr EBV
The first pilot study for the endobronchial valves was published in March of 2003, by Toma et al. with eight patients with severe emphysema undergoing unilateral valve placement (2). All of these cases were patients with extremely severe disease, five of these patients had emphysema that was too severe for LVRS and the other three did not wish to undergo surgery. After unilateral valve placement, the median forced expiratory volume in one second (FEV1) increased 34%, diffusing capacity of the lung for carbon monoxide (DLCO) increased 29%, and the computed tomography (CT) scans showed significant reduction in the volume of the treated lobe. Despite the extreme severity of emphysema in this series, complications were limited to two pneumothoracies with only one requiring drainage. This series was followed shortly by a similar study with 10 patients published in September 2003, by Snell et al. describing the implantation of EBVs in patients with severe emphysema and hyperinflation (3). Although no improvement in spirometric, functional or radiologic findings were seen at 30 days, no major complications were noted and the minor complications of COPD exacerbation (n=3), asymptomatic localized pneumothorax (n=1) and lower lobe pneumonia (n=1) were limited, thus adding to the feasibility and safety data for the procedure.
In 2004, Yim et al. (4) studied the feasibility, safety, and short-term efficacy of the EBVs in 21 patients. They showed significant improvement in spirometric measurement of FEV1 and forced vital capacity (FVC) at 90 days and all functional parameters [6-minute walk, Short-Form Health Survey, St George’s Respiratory Questionnaire (SGRQ), modified Medical Research Council (mMRC) at both 30 and 90 days]. Although a small study, the results were encouraging.
In 2006, Wan et al. (5) reported on the first multicenter experience (nine centers in seven countries) by retrospectively analyzing 98 cases from a prospective multicenter registry. In this cohort, there was a significant improvement in FEV1, FVC, residual volume (RV), and 6-minute walk at 90 days. Eight point two percent had serious complications including one death. There was also an interesting trend toward improvement in those patients had an entire lobe treated compared to those with just one or two bronchopulmonary segments treated. They concluded that this was further evidence that bronchoscopic valve therapy could produce improvements similar to those seen in LVRS but patient selection needed further study.
In 2010, the Endobronchial Valve for Emphysema Palliation Trial (VENT) was published. In a 2:1 randomization scheme, 321 subjects with heterogeneous emphysema and severe COPD were enrolled and 220 received the EBV treatment. Primary endpoints were FEV1 and 6-minute walk test (6MWT). Safety was assessed using a composite rate of six predetermined complications. The study showed small but statistically significant improvements in lung function (4.3% increase in FEV1), exercise tolerance and quality of life but also showed a significant increase in complications such as COPD exacerbations, pneumonia and hemoptysis in the treated group. At 12 months, the rate of the complications composite was 10.3% in the EBV group versus 4.6% in the control group (P=0.17). Heterogeneity of emphysema and fissure completeness were analyzed using quantitative CT and an association was found suggesting a greater response to the treatment for subjects with greater heterogeneity of emphysema within their lungs and complete fissures (6,7). The European cohort of the VENT was analyzed and reported separately in 2012 by Herth et al. (8). Treatment group consisted of 111 subjects versus 60 in the medical management group. Unlike the initial VENT cohort results (6), the European cohort did not show a significant difference in rates of complications between the treatment and control group yet still had significant improvement in the FEV1, cycle ergometry and SGRQ. Radiographic analysis of the CT scans demonstrated an association with better outcomes in those patients with complete fissures but no association with the degree of heterogeneity of emphysema.
Spiration IBV
In 2007, a multicenter trial using the Spiration IBV in 30 patients was published showing significant improvement in health-related quality of life metrics although no significant difference in physiologic and exercise outcomes (9). Five years later in 2012, Ninane et al. (10) reported a European multicentre, blinded, sham-controlled study evaluating the safety and effectiveness of the Spiration IBV for treatment of bilateral upper lobe emphysema. This trial was specifically designed to evaluate the treatment when performed without the goal of lobar atelectasis. Patients with upper lobe predominant severe emphysema were selected for the study. Seventy three enrolled with 37 randomized to the treatment arm and 36 to the sham treatment arm. Primary outcomes were the SGRQ and lobar volume shift measured by quantitative CT (increase in lower lobe volume in the setting of decreased upper lobe volume post treatment). A positive responder was required to have both a ≥4-point improvement in SGRQ and a lobar volume shift. Only 24% (8/37) of the treatment group and none in the sham group met criteria for a positive response. Overall, there was a significant difference in the lobar volume shift between groups. Both groups improved on the SGRQ. There were no differences between groups in adverse events.
Valve concept comparison
The Spiration IBV studies described above studied a bilateral upper lobe deployment strategy without the intent to produce lobar atelectasis but instead create a redistribution of ventilation to less emphysematous airways. The Zephyr EBV studies have concentrated primarily on the unilateral valve deployment with the goal of producing total lobar atelectasis. Recently, Eberhart et al. [2012] published a randomized trial directly comparing these two techniques. With 11 subjects in each arm, he demonstrated that the unilateral lobar atelectasis approach was significantly superior to a bilateral partially occlusive approach at 30 and 90 days when comparing improvements in pulmonary function tests (PFTs), 6-min walk distance (6MWD), dyspnea score as measured by the mMRC dyspnea score, and quality of life as measured by the SGRQ (11). Although the study was small, the evidence certainly suggests that producing total lobar collapse with the valves is more likely to result in clinical improvement for the patient. The existence of collateral ventilation in the lung was recognized by the work of Van Allen and others in 1931 (12). The evolution of the endobronchial valves and lessons learned from each trial have clearly demonstrated the importance of recognizing and mitigating collateral ventilation within the lungs. Research in devices that can identify areas of collateral circulation in an individual’s lungs are actively being studied and initial studies have confirmed the ability to more effectively guide placement of endobronchial valves (13,14).
Lung volume reduction coils (LVRC)
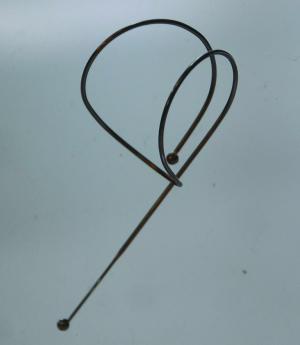
LVRC is a technique for bronchoscopic treatment of severe COPD using a nitinol coil that is delivered to the mid lung airways under fluoroscopy in a sheath which keeps it straightened and then when the sheath is pulled back, the straightened coil returns to its normal shape that resembles the seams on a baseball compressing the surrounding parenchyma and restoring elasticity to the emphysematous lung (Figure 3). This technique is unique because it is unaffected by collateral flow and appears to be effective on heterogeneous and homogeneous emphysema and is also independent of collateral ventilation. Since the proposed mechanism is restoring elasticity to the parenchyma from shortening of the airways, patients with large bullae are unlikely to benefit from the technique and have been excluded from current studies (15,16).
Results of the first pilot study using this device were published in 2010 by Herth et al. with 11 patients that showed safety and some evidence of efficacy. This pilot was followed by another trial in 2012 with 16 patients that demonstrated a significant improvement in SGRQ, FEV1, FVC, RV, and 6MWT at 6 months with an acceptable safety profile (17). The first randomized controlled trial of the device (RESET trial) was published by Shah et al. in 2013. With 47 patients total (23 LVRC, 24 control) there was a significant improvement in the primary endpoint of quality of life as measured on the SGRQ in the treatment group and no difference in the safety endpoints between the groups (18). While LVRC is one of the newer techniques for the bronchoscopic treatment of severe COPD, it has already distinguished itself as one of the more promising because of its safety profile and demonstrated ability to work in patients with both heterogeneous and homogeneous emphysema independently from the effects of collateral ventilation.
Airway bypass
Small endobronchial vents placed bronchoscopically through holes made directly in the airway wall to allow direct flow of trapped air in the emphysematous lung is referred to as airway bypass. Essentially the concept is that by creating holes in the airways and stenting them open with drug eluting stents, they will remain open and allow emphysematous areas of lung with trapped air to escape to the larger airways more easily. A doppler probe is used to interrogate the target site for the hole to ensure there is no vessel at that location. The exhale airway stents for emphysema (EASE) trial was a prospective randomized, double-blind, sham-controlled study published in 2011 that studied 315 subjects with homogenous emphysema and with severe hyperinflation documented by a ratio of RV to total lung capacity of ≥0.65 (19). Primary efficacy endpoint was at least a 12% increase in FVC and at least 1-point decrease in the mMRC dyspnea score from baseline. No difference between treatment and sham groups was seen in the efficacy or safety endpoints at 6 or 12 months. Initially the vents produced an improvement in lung function but the vents tended to become obstructed over time with granulation tissue or mucus and the improvements were not sustainable over time. The issue of vent obstruction was noted on earlier studies and the addition of drug eluting stents for the EASE trial was an attempt to prevent granulation obstruction of the vents. While the concept of airway bypass was confirmed, this technology does not appear to be effective in its current state.
Glue and biologics for bronchoscopic lung volume reduction
Adhesives have been used in the treatment and prevention of persistent air leaks complicating thoracic interventions. Fibrin sealant has been applied successfully via thoracoscopy in the ablation of persistent air leaks following tube thoracostomy or pulmonary resections (20). Additionally the use of surgical sealants has also been examined in the prevention of post-operative persistent air leaks. A recent meta-analysis of 13 studies comprising 1,335 patients concluded that the use of surgical sealants and buttressing decreases the risk of prolonged air leaks after pulmonary resections. The authors cautioned, however, that given the possibility of publication bias their interpretations should be used with caution and that further trials are warranted to confirm the effectiveness of this method (21).
Investigators have started to examine the effectiveness of bronchoscopic administration of adhesives in the treatment of advanced COPD. The application of a biologic sealant delivered bronchoscopically to sheep had been demonstrated to be effective in collapsing targeted areas of lung and inducing localized scar tissue formation and ultimately reduction of lung tissue volume (22). Using these principles Reilly and others conducted a phase I trial designed to evaluate the safety of biologic lung volume reduction in six patients with severe predominantly upper-lobe COPD based upon CT scan appearance. A biogel composed of fibrin and thrombin was instilled via a flexible bronchoscope through which a dual lumen catheter was placed. Three patients had two subsegments treated and three patients had four subsegments treated. There were no serious adverse effects and small improvements were observed in mean vital capacity, mean RV, mean RV/total lung capacity ratio (RV/TLC), mean 6MWT, and medical research council dyspnea (MRCD) score (23).
A larger phase II study was performed on patients with global initiative for chronic obstructive lung disease (GOLD) stage III and IV using the bronchoscopically delivered fibrin and thrombin hydrogel. Two different doses of the hydrogel were delivered into 50 patients with upper lobe predominant emphysema. All patients had eight subsegments targeted (four in each upper lobe) based upon the most diseased portion of the lung determined with pre-procedural high resolution CT scan (HRCT). Twenty-eight patients had 10 mL and 22 patients had 20 mL of the hydrogel applied to each targeted subsegment. There were no procedure related deaths, but there was an 8% incidence of serious cardiopulmonary adverse events. At 6 weeks of follow-up there were statistically significant improvements in FEV1, FVC, RV/TLC, MRCD score, and health-related quality of life (HRQOL) score in both the low-dose (LD) and high-dose (HD) groups. However, at 6 months only the HD group had sustained significant improvements in all physiologic outcome measures (24).
The two previous studies focused on patients with heterogeneous upper-lobe predominant emphysema. Another study examined the effect of the application of fibrin and thrombin hydrogel to patients with homogeneous emphysema and severe airflow obstruction defined as a FEV1/FVC <70% and FEV1 <45%. In this non-randomized study patients were selected to receive either the LD (n=8) or HD (n=17) dose as described in the previous study. The subsegments were chosen based upon the results of both CT and radionucleotide lung perfusion scanning and each patient had eight subsegments treated in the upper lobes or superior segments of the lower lobes. There were no procedure related deaths, though the majority of the patients experienced transient leukocytosis, fever, or malaise. There were also two COPD exacerbations in the LD group and three in the HD group. At 3 months of follow-up only the HD group had statistically significant improvement in the primary end-point, RV/TLC ratio (–6.9). There were also significant improvements in FEV1, MRCD score, and SGRQ. The authors do note that the responses in patients with homogeneous disease were smaller than those with upper lobe heterogeneous disease reported in prior studies (25).
A synthetic polymer emphysematous lung sealant (ELS, AeriSeal®, Aeris Therapeutics,Woburn, MA) has recently been developed. The foam sealant is delivered via a single lumen catheter placed through the working channel of a flexible bronchoscope. Unlike the fibrin and thrombin hydrogel the foam sealant is not delivered as two separate components to the target site, but is rather mixed prior to instillation through the catheter. In a prospective, non-controlled study of 25 patients with heterogeneous emphysema the ELS was applied to up to six different subsegments during one or two treatment sessions. Similar to the patients that received the fibrin and thrombin hydrogel a transient inflammatory reaction was common. There were no treatment-associated mortalities, but there were ten acute or sub-acute COPD exacerbations. There were improvements from baseline at 24 weeks in FEV1 (+10.0), FVC (+15.86), RV/TLC (–4.7), SGRQ score (–7.5 units) and 6MWT (+24.6 m), however, only the FVC has statistically significant improvements when corrected for multiple comparisons. The physiologic improvements in ELS therapy were greater in patients with GOLD stage III disease (26).
The ELS system was used in another small trial of 20 patients with advanced emphysema, 10 with upper lobe and 10 with homogeneous disease. The procedure was bilateral with two subsegments targeted in each upper lobe. The procedure was performed only with conscious sedation and was fairly short (approximately 15 minutes) with an average hospitalization of about 1 day. The primary end-point of reduction in upper lobe volume assessed by quantitative CT scan at 3 months was successful with a statistically significant reduction of 895 mL. There were additional physiologic improvements at 6 and 12 months in FEV1, RV/TLC, DLCO, MRCD score, and SGRQ. One serious procedure complication occurred and there were seven significant respiratory adverse events during follow-up (27).
Similar to vapor therapy ELS has been demonstrated to lead to physiologic improvements despite the integrity of lung fissures. A report by Magnussen et al. summarized the results of three trials of patients that had undergone ELS treatment. Of the patients enrolled only 28 had complete data sets that allowed analysis. ELS therapy reduced lung volumes independent of interlobar fissure integrity in patients with heterogeneous upper-lobe emphysema. Additionally there were similar improvements in gas trapping, spirometry, functional capacity, and quality of life between those patients with complete and incomplete fissures (28).
Overall this data suggests that the application of adhesives in the treatment of emphysema has a safety profile better than surgical lung volume reduction and comparable to other methods of bronchoscopic lung volume reduction. There appears to be physiologic improvements in spirometry, functional ability, and quality of life. Both fibrin/thrombin hydrogels and a synthetic polymer have been used, but never compared in a single trial. This procedure leads to permanent subsegmental collapse and is not affected by fissure integrity. Despite the promise of several small studies, larger, randomized controlled trials are needed.
Vapor therapy for lung volume reduction
Vapor therapy for COPD is a new technology that delivers thermal energy in the form of heated water vapor to target subsegments of the lung. It is performed via a disposable catheter introduced through the working channel of a flexible bronchoscope and thus can be done in a minimally invasive manner to patients that are under moderate sedation. The InterVapor™ (Uptake Medical Corp., Tustin, CA) consists of a vapor generator and a flexible catheter. Each procedure is specifically tailored to the individual based upon software analysis performed on a HRCT. The subsegments are targeted based upon the degree of heterogeneity and an energy dose of 5 to 10 calories per estimated gram of tissue is delivered to the selected subsegments. This thermal energy leads to an inflammatory response that ultimately causes contraction fibrosis and atelectasis with subsequent lung volume reduction. The results of this procedure are permanent unlike the placement of one-way endobronchial valves or coils that can theoretically be removed at a later date (29).
A feasibility study was performed in 11 patients with severe heterogeneous COPD. These patients underwent unilateral application of vapor therapy at five calories per estimated gram of tissue. Compared with the patients baseline data there were significant improvements in DLCO (16%) as well as improvement in the SGRQ at 6 months. There were, however, no significant improvements in FEV1, FVC, RV or 6MWT during the same amount of follow-up. The improvement in SGRQ was reportedly superior to other methods of bronchoscopic lung volume reduction and the DLCO improvements were similar to those of surgical lung volume reduction. Side effects of the procedure included nausea, cough, hemoptysis, fatigue, and COPD exacerbations. There were seven COPD exacerbations in four patients three of which were judged to be infectious and four noninfectious in nature (19).
A larger study was performed in 44 patients with heterogeneous upper lobe emphysema. Once again the patients underwent unilateral treatment with the targets based upon prior CT scan evaluation. A calculated amount of energy of 10 calories per gram of tissue was applied to each targets lung segment for 3 to 10 seconds. Twenty-four patients were treated in the right upper lobe and 20 patients in the left upper lobe. At the 6-month post-procedure evaluation the patients had improvement in FEV1 of 141 mL, and a reduction in RV of 406 mL. There was also an improvement in SGRQ of –14 units as well as 6MWT of 46.5 m. The most common adverse events were COPD exacerbations, which occurred in 11 patients most often within the first 30 days following treatment (30).
A follow-up study was performed in the same group at 12 months. The overall finding was that the treated patients continued to have improvement at the 1 year mark, although it was to a lesser degree that that seen at 6 months. The improvements in FEV1 fell to 86 mL and RV to –303 mL. The SGRQ score was –11 units and the distance in 6MWT was only 18.5 m above pretreatment baseline. On subgroup analysis it was found that improvements in lung function and exercise capability were similar at the 6-month evaluation, but greater at 12 months in those patients with GOLD stage IV disease compared to stage III. Twenty-three patients experienced 39 serious adverse events, 22 of which were respiratory. Two patients died during the follow-up period. One was secondary to end-stage lung disease at 67 days post-treatment and another occurred at 350 days post-treatment secondary to surgical complications following a lobectomy for aspergillus in the untreated lung (31).
Collateral circulation likely accounts for the failure of some patients to achieve atelectasis after large airway occlusion by endobronchial valves. This may be due to lack of fissure integrity. In a retrospective analysis of the study involving 44 patients discussed previously it was found that there was no to minimal association between lobar fissure integrity and the effectiveness of bronchoscopic thermal vapor ablation (BTVA). This is explained by the fact that areas of the lung that have undergone remodeling following contraction fibrosis are unlikely to re-inflate despite the presence of collateral ventilation. As such patients with incomplete fissures identified on HRCT may achieve more effective lung volume reduction than if they underwent large airway occlusion with a prosthetic device (32-51).
These small studies suggest that the application of steam to carefully selected sub segments of the lung in patients with heterogeneous upper lobe predominant emphysema may improve lung function, exercise tolerance and quality of life. These improvements may be more sustained in those patients with more severe disease. Unlike prosthetics such as endobronchial valves or coils the success of vapor therapy is independent of fissure integrity. Although promising, larger studies with prolonged follow-up are needed prior to wide application of this technology to the general population of patients with COPD (Figures 1-3).
Conclusions
Bronchoscopic interventions to treat severe COPD have made great progress over the last decade offering benefit to patients with few treatment options available. While trying to achieve the benefits seen LVRS with less morbidity and mortality, several diverse techniques described above have been developed. These various techniques have unique approaches that have uncovered some of the critical obstacles to success such as collateral ventilation and incomplete occlusion of the target lobe. As these techniques advance, we may continue to see that in the wide spectrum of severe COPD patients, refinement of selection criteria for the respective techniques may have a significant impact on the results for the patient.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Fishman A, Martinez F, Naunheim K, et al. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059-73. [PubMed]
- Toma TP, Hopkinson NS, Hillier J, et al. Bronchoscopic volume reduction with valve implants in patients with severe emphysema. Lancet 2003;361:931-3. [PubMed]
- Snell GI, Holsworth L, Borrill ZL, et al. The potential for bronchoscopic lung volume reduction using bronchial prostheses: a pilot study. Chest 2003;124:1073-80. [PubMed]
- Yim AP, Hwong TM, Lee TW, et al. Early results of endoscopic lung volume reduction for emphysema. J Thorac Cardiovasc Surg 2004;127:1564-73. [PubMed]
- Wan IY, Toma TP, Geddes DM, et al. Bronchoscopic lung volume reduction for end-stage emphysema: report on the first 98 patients. Chest 2006;129:518-26. [PubMed]
- Strange C, Herth FJ, Kovitz KL, et al. Design of the Endobronchial Valve for Emphysema Palliation Trial (VENT): a non-surgical method of lung volume reduction. BMC Pulm Med 2007;7:10. [PubMed]
- Sciurba FC, Ernst A, Herth FJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med 2010;363:1233-44. [PubMed]
- Herth FJ, Noppen M, Valipour A, et al. Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort. Eur Respir J 2012;39:1334-42. [PubMed]
- Wood DE, McKenna RJ Jr, Yusen RD, et al. A multicenter trial of an intrabronchial valve for treatment of severe emphysema. J Thorac Cardiovasc Surg 2007;133:65-73. [PubMed]
- Ninane V, Geltner C, Bezzi M, et al. Multicentre European study for the treatment of advanced emphysema with bronchial valves. Eur Respir J 2012;39:1319-25. [PubMed]
- Eberhardt R, Gompelmann D, Schuhmann M, et al. Complete unilateral vs partial bilateral endoscopic lung volume reduction in patients with bilateral lung emphysema. Chest 2012;142:900-8. [PubMed]
- Van Allen CM, Lindskog GE, Richter HG. Collateral respiration. Transfer of air collaterally between pulmonary lobules. J Clin Invest 1931;10:559-90. [PubMed]
- Herth FJ, Eberhardt R, Gompelmann D, et al. Radiological and clinical outcomes of using Chartis™ to plan endobronchial valve treatment. Eur Respir J 2013;41:302-8. [PubMed]
- Votruba J, Collins J, Herth FJ. Successful treatment of ventilator dependent emphysema with Chartis treatment planning and endobronchial valves. Int J Surg Case Rep 2011;2:285-7. [PubMed]
- Herth FJ, Eberhard R, Gompelmann D, et al. Bronchoscopic lung volume reduction with a dedicated coil: a clinical pilot study. Ther Adv Respir Dis 2010;4:225-31. [PubMed]
- Slebos DJ, Klooster K, Ernst A, et al. Bronchoscopic lung volume reduction coil treatment of patients with severe heterogeneous emphysema. Chest 2012;142:574-82. [PubMed]
- Papaioannou M, Pitsiou G, Manika K, et al. COPD assessment test: a simple tool to evaluate disease severity and response to treatment. COPD 2014;11:489-95. [PubMed]
- Shah PL, Zoumot Z, Singh S, et al. Endobronchial coils for the treatment of severe emphysema with hyperinflation (RESET): a randomised controlled trial. Lancet Respir Med 2013;1:233-40. [PubMed]
- Shah PL, Slebos DJ, Cardoso PF, et al. Bronchoscopic lung-volume reduction with Exhale airway stents for emphysema (EASE trial): randomised, sham-controlled, multicentre trial. Lancet 2011;378:997-1005. [PubMed]
- Thistlethwaite PA, Luketich JD, Ferson PF, et al. Ablation of persistent air leaks after thoracic procedures with fibrin sealant. Ann Thorac Surg 1999;67:575-7. [PubMed]
- Malapert G, Hanna HA, Pages PB, et al. Surgical sealant for the prevention of prolonged air leak after lung resection: meta-analysis. Ann Thorac Surg 2010;90:1779-85. [PubMed]
- Ingenito EP, Berger RL, Henderson AC, et al. Bronchoscopic lung volume reduction using tissue engineering principles. Am J Respir Crit Care Med 2003;167:771-8. [PubMed]
- Reilly J, Washko G, Pinto-Plata V, et al. Biological lung volume reduction: a new bronchoscopic therapy for advanced emphysema. Chest 2007;131:1108-13. [PubMed]
- Criner GJ, Pinto-Plata V, Strange C, et al. Biologic lung volume reduction in advanced upper lobe emphysema: phase 2 results. Am J Respir Crit Care Med 2009;179:791-8. [PubMed]
- Refaely Y, Dransfield M, Kramer MR, et al. Biologic lung volume reduction therapy for advanced homogeneous emphysema. Eur Respir J 2010;36:20-7. [PubMed]
- Herth FJ, Gompelmann D, Stanzel F, et al. Treatment of advanced emphysema with emphysematous lung sealant (AeriSeal®). Respiration 2011;82:36-45. [PubMed]
- Kramer MR, Refaely Y, Maimon N, et al. Bilateral endoscopic sealant lung volume reduction therapy for advanced emphysema. Chest 2012;142:1111-7. [PubMed]
- Magnussen H, Kramer MR, Kirsten AM, et al. Effect of fissure integrity on lung volume reduction using a polymer sealant in advanced emphysema. Thorax 2012;67:302-8. [PubMed]
- Snell GI, Hopkins P, Westall G, et al. A feasibility and safety study of bronchoscopic thermal vapor ablation: a novel emphysema therapy. Ann Thorac Surg 2009;88:1993-8. [PubMed]
- Snell G, Herth FJ, Hopkins P, et al. Bronchoscopic thermal vapour ablation therapy in the management of heterogeneous emphysema. Eur Respir J 2012;39:1326-33. [PubMed]
- Herth FJ, Ernst A, Baker KM, et al. Characterization of outcomes 1 year after endoscopic thermal vapor ablation for patients with heterogeneous emphysema. Int J Chron Obstruct Pulmon Dis 2012;7:397-405. [PubMed]
- Gompelmann D, Heussel CP, Eberhardt R, et al. Efficacy of bronchoscopic thermal vapor ablation and lobar fissure completeness in patients with heterogeneous emphysema. Respiration 2012;83:400-6. [PubMed]
- Tsakiridis K, Mpakas A, Kesisis G, et al. Lung inflammatory response syndrome after cardiac-operations and treatment of lornoxicam. J Thorac Dis 2014;6:S78-98. [PubMed]
- Tsakiridis K, Zarogoulidis P, Vretzkakis G, et al. Effect of lornoxicam in lung inflammatory response syndrome after operations for cardiac surgery with cardiopulmonary bypass. J Thorac Dis 2014;6:S7-20. [PubMed]
- Argiriou M, Kolokotron SM, Sakellaridis T, et al. Right heart failure post left ventricular assist device implantation. J Thorac Dis 2014;6:S52-9. [PubMed]
- Madesis A, Tsakiridis K, Zarogoulidis P, et al. Review of mitral valve insufficiency: repair or replacement. J Thorac Dis 2014;6:S39-51. [PubMed]
- Siminelakis S, Kakourou A, Batistatou A, et al. Thirteen years follow-up of heart myxoma operated patients: what is the appropriate surgical technique? J Thorac Dis 2014;6:S32-8. [PubMed]
- Foroulis CN, Kleontas A, Karatzopoulos A, et al. Early reoperation performed for the management of complications in patients undergoing general thoracic surgical procedures. J Thorac Dis 2014;6:S21-31. [PubMed]
- Nikolaos P, Vasilios L, Efstratios K, et al. Therapeutic modalities for Pancoast tumors. J Thorac Dis 2014;6:S180-93. [PubMed]
- Koutentakis M, Siminelakis S, Korantzopoulos P, et al. Surgical management of cardiac implantable electronic device infections. J Thorac Dis 2014;6:S173-9. [PubMed]
- Spyratos D, Zarogoulidis P, Porpodis K, et al. Preoperative evaluation for lung cancer resection. J Thorac Dis 2014;6:S162-6. [PubMed]
- Porpodis K, Zarogoulidis P, Spyratos D, et al. Pneumothorax and asthma. J Thorac Dis 2014;6:S152-61. [PubMed]
- Panagopoulos N, Leivaditis V, Koletsis E, et al. Pancoast tumors: characteristics and preoperative assessment. J Thorac Dis 2014;6:S108-15. [PubMed]
- Visouli AN, Darwiche K, Mpakas A, et al. Catamenial pneumothorax: a rare entity? Report of 5 cases and review of the literature. J Thorac Dis 2012;4:17-31. [PubMed]
- Zarogoulidis P, Chatzaki E, Hohenforst-Schmidt W, et al. Management of malignant pleural effusion by suicide gene therapy in advanced stage lung cancer: a case series and literature review. Cancer Gene Ther 2012;19:593-600. [PubMed]
- Papaioannou M, Pitsiou G, Manika K, et al. COPD Assessment Test: A Simple Tool to Evaluate Disease Severity and Response to Treatment. COPD 2014;11:489-95. [PubMed]
- Porpodis K, Zarogoulidis P, Spyratos D, et al. Pneumothorax and asthma. J Thorac Dis 2014;6:S152-61. [PubMed]
- Papaiwannou A, Zarogoulidis P, Porpodis K, et al. Asthma-chronic obstructive pulmonary disease overlap syndrome (ACOS): current literature review. J Thorac Dis 2014;6:S146-51. [PubMed]
- Zarogoulidis P, Porpodis K, Kioumis I, et al. Experimentation with inhaled bronchodilators and corticosteroids. Int J Pharm 2014;461:411-8. [PubMed]
- Bai C, Huang H, Yao X, et al. Application of flexible bronchoscopy in inhalation lung injury. Diagn Pathol 2013;8:174. [PubMed]
- Zarogoulidis P, Kioumis I, Porpodis K, et al. Clinical experimentation with aerosol antibiotics: current and future methods of administration. Drug Des Devel Ther 2013;7:1115-34. [PubMed]