
Innovative operation concept and practice: preoperative precise planning is benefit for lung function protection of early esophageal squamous cell carcinoma by robotic surgical system
Postoperative complications of esophageal squamous cell carcinoma (ESCC) patients emerge in an endless stream with a high incidence rate. Pulmonary complications are the most common complications and one of the main causes of death in patients with esophageal cancer after operation. The incidence rate is about 15.1% (1). To overcome this dilemma, we propose the innovative operation concept of “preoperative precise planning is benefit for lung function protection of radical resection of early ESCC by robotic surgical system”. The purpose of this innovative operation concept is to improve individualized identification of pulmonary branch of vagus nerve, recurrent laryngeal nerve and bronchial artery perfectly. This innovative technology concept aims to reduce the overall incidence of postoperative complications, improve the long-term quality of life of patients, and accelerate postoperative rehabilitation.
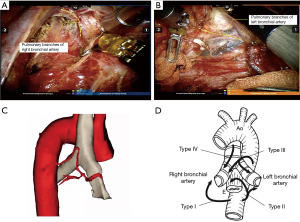
3D reconstruction of bronchial artery was performed before operation based on bronchial artery CTA data. According to Japanese bronchial artery classification (2), the patient had bilateral bronchial arteries that dried together and originated from the thoracic aorta, which was type I. Thoracoscopic esophagectomy was performed through four 2-cm assist ports. Robotic surgical system was monitored with Da Vinci Si surgical System. First, intraoperative exploration showed the tumor was located in the middle thoracic segment and the upper pole was at the level of the right lower pulmonary vein. No fibrous membrane was invaded. According to the preoperative three-dimensional reconstruction image combined with intraoperative bronchial artery, the azygos vein arch and bronchial artery should be reserved (Figure 1). Next, pay attention to preserve the pulmonary branch of vagus nerve during the process of free upward along the pulmonary vein and cut off esophageal branch of vagus nerve. Searching lymph nodes and expose bilateral recurrent laryngeal nerve from arterial level below the right clavicle and left tracheal gully 106tbl station respectively. The process of removing peripheral lymph nodes of recurrent laryngeal nerves should avoid exposing the nerves. And protection of bleeding is also requested (Video 1). The abdominal and cervical surgical sections were same as the traditional endoscopes.
The operation took 187 minutes. The blood loss was 55 mL. Postoperative pathology: Medullated squamous cell carcinoma of the esophagus (esophagus + partial stomach), no infiltrating fibrous membranes and no invasion of nerves. No tumors were found in the “esophageal incision” and “gastric incision”. No metastatic cancer was found in the lymph nodes. TNM staging: T2N0M0 G2IIA. The patient was discharged on the 7th day after operation without postoperative complications.
Postoperative complications and quality of life are greatly affected by surgical techniques and surgical concept. First of all, some scholars conducted animal experiments on bronchial artery dissection, which indicated that the bronchial artery was severed several days later, and autopsy revealed bronchial ulcer or even perforation (3). Secondly, during the dissection lymph nodes, if recurrent laryngeal nerve and pulmonary branch of vagus nerve, which may affect patients’ cough and sputum. In addition, traditional thoracoscopy has a 2-dimensional field of vision with low magnification and poor mobility of the instrument, which has obvious limitations and increases the risk of accidental injury during the operation.
Facing the above difficulties and bottlenecks, we firstly propose the innovative operation concept and design to intraoperative precision preserve bilateral bronchial artery, pulmonary branch of vagus nerve and recurrent laryngeal nerve damage. Combining with 3D reconstruction technology and robotic surgery system, we expect to reduce postoperative chronic cough, improve the long-term quality of life. At present, 16 cases of functional minimally invasive radical resection of esophageal cancer assisted by robots have been achieved in our department. No serious pulmonary infection, anastomotic fistula and hoarseness have occurred after surgery.
Based on the current clinical results and theoretical basis, we believe that this innovative surgical concept is feasible and effective, which could be promoted in early esophageal cancer and provide better functional protection results.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.116). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent for publication was obtained from all participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yamamoto S, Kawahara K, Maekawa T, et al. Minimally invasive esophagectomy for stage I and II esophageal cancer. Ann Thorac Surg 2005;80:2070-5. [Crossref] [PubMed]
- Hayasaka K, Ishida H, Kimura R, et al. A new anatomical classification of the bronchial arteries based on the spatial relationships to the esophagus and the tracheobronchus. Surg Today 2017;47:883-90. [Crossref] [PubMed]
- Fujita H, Kawahara H, Hidaka M, et al. An experimental study on viability of the devascularized trachea. Jpn J Surg 1988;18:77-83. [Crossref] [PubMed]


