CT-guided blood tattoo for thoracoscopic excision of lung lesions in pediatric patients
Introduction
The role of lung biopsies in pediatric patients can vary from diagnosing a primary malignant versus benign tumor to staging distant malignant disease. Surgical techniques of obtaining lung biopsies have expanded beyond thoracotomy to video-assisted thoracoscopic surgery (VATS) and bronchoscopy which are safe and effective techniques associated with decreased morbidity and length of hospital stay versus the traditional open thoracotomy (1,2). Furthermore, surgical biopsy has a higher diagnostic yield, reported up to 100% with thoracotomy and thoracoscopy, as compared to 80% with the percutaneous approach (3). Successful tissue sampling is particularly important in the pediatric population, as metastatic disease to the lung usually involves atypical or aggressive neoplasms and, in the instance of a single nodule, excisional wedge biopsy can improve survival (4,5).
While pleural based nodules are relatively easily visualized with VATS, a limitation is the restricted ability to palpate nodules that are within the parenchyma. This limitation has led to the development of several preoperative localization techniques, well described in the adult literature (6,7), which can assist in accurate intraoperative localization. Commonly used preoperative techniques include injection of dyes, CT-guided placement of hookwires, or ultrasound-guided biopsy, each of which have demonstrated limitations. Methylene blue may diffuse into the tissues prior to operative treatment, thus distorting the area of intended biopsy (8). Hookwires have been reported to dislodge prior to intraoperative localization, also limiting localization during VATS and the use of ultrasound is highly operator-dependent (9,10). Our aim was to demonstrate the use of CT-guided injection of autologous blood as a safe and effective method for pulmonary nodule localization.
Methods
Data collection
The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. After obtaining local Institutional Review Board (IRB) approval (IRB #00028981), we conducted a retrospective review from 2006 to 2019 of patients (ages 4–18 years old) at our institution that received a blood tattoo with autologous blood under CT guidance for the preoperative localization of a peripheral pulmonary nodules. All patients underwent informed consent prior to performing all procedures. The decision for surgical resection of pulmonary nodules was based on need for tissue diagnosis and accessibility by video-assisted thoracoscopic surgery (VATS). The size of the nodules, pathologic diagnosis, and procedural complications were reviewed. Preoperative CT scans of all patients were reviewed to determine the depth of the nodules from the pleural surface.
Preparation and CT guided localization
Informed consent was obtained from guardians on all patients prior to CT-guided blood tattoo (CGBT) and surgical resection. All procedures were performed with the patient intubated under general anesthesia. Tumor localization was performed using CT Fluoroscopy (Siemens AS320 CT scanner). Scout imaging was reviewed for pre-procedural planning. The distance from the closest pleural surface to the center of the nodule was measured on the initial staging CT. Local anesthesia was administered along the planned needle path. A needle (18–20 G) was advanced adjacent to the pulmonary lesion. Each patient had autologous blood drawn once the needle was in place, which was placed immediately next to the pulmonary nodule and was then subsequently withdrawn with continuous injection of autologous blood. The total injection volumes ranged from 0.5 to 10 mL. The intubated patient was taken directly to the operating room following the procedure or positioned on the operating table in our integrated operating room.
Surgical resection
Surgical procedures were performed after informed consent was obtained by the designated guardians of each patient. All biopsies were obtained after patient transfer to the operating room/or repositioned on the table in our integrated operating room, and patients were placed in the lateral decubitus position according to the side of the mass location. Intercostal nerve blocks were performed prior to typical VATS trocar placement between the rib spaces, followed by carbon dioxide insufflation and visualization was achieved with a 5 mm 30-degree thoracoscope. Once the tattooed areas were visualized, either 45 to 60 mm endoscopic linear cutting staplers or the LigaSure device were utilized to perform a wedge resection for the purpose of excisional biopsy.
Results
Collective results
All 11 cases were completed successfully thoracoscopically and none required conversion to open thoracotomy. Patient ages ranged from 4–18 years old. A total of 22 nodules were localized preoperatively, ranging in size from 2 to 14 mm (Table 1). The nodules were located as deep as 24 mm from the pleural surface. In 82% of the patients, a metastatic malignancy was confirmed by pathologic analysis. 21/22 of the nodules were localized intraoperatively and yielded diagnostic results on pathologic review. The volume of autologous blood injected ranged from 0.5 to 10 mL. No complications were seen following the VATS procedure. Two patients had a small pneumothorax observed after the percutaneous injection of clot, however, one was residual from a previously performed VATS procedure. The average length of hospital stay was two days and 54% of patients were discharged home after the procedure. All except one case were performed using a single-lumen endotracheal tube (ETT) for inhalation anesthesia (one patient with bilateral resections had a double lumen ETT).

Full table
Example cases
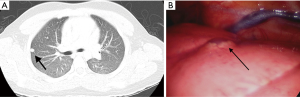
The first patient to utilize this technique at our institution presented with type 1 neurofibromatosis and a 2 cm nodule, and initially underwent two wedge resections without preoperative localization (Figure 1). These resections returned as negative for tumor cells on pathologic analysis. Following the initial resection, a repeat VATS biopsy with preoperative localization using CGBT was performed. The patient was scanned prior to the biopsy and only one of the two nodules in the right lung were present on the scan. The procedure was planned for the 8mm right lower lobe nodule. Using CGBT, a total of 5 mL of autologous blood drawn into a vacuum tube and was subsequently injected. Post injection imaging demonstrated parenchymal hematoma at needle tip. There were no immediate complications and the patient was taken directly to the OR following the procedure (Figure 2). Pathology following wedge resection then showed a 7 mm nodule in the wedge resection, with an additional 2 mm satellite nodule, both representing malignant peripheral nerve sheath tumors. The patient was extubated and suffered no complications.
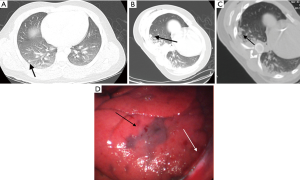
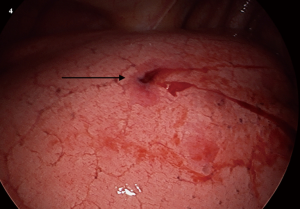
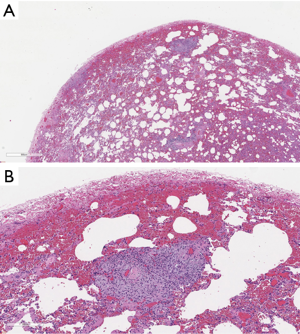
A second example patient underwent MRI which revealed a 7 cm mass behind the left knee, which was biopsied and found to be a synovial sarcoma. He then underwent a PET CT scan, which demonstrated multiple FDG-Avid pulmonary nodules as well as external iliac lymph nodes that were also metabolically active. The iliac nodes seen on PET scan were not easily amenable to biopsy without a radical dissection. CGBT of the largest peripheral pulmonary nodule located in the left upper lobe followed by thoracoscopic lung biopsy and port placement for chemotherapy was recommended and planned (Figure 3). The blood tattoo was visualized intraoperatively (Figure 4) and the nodule was resected successfully, revealing a metastatic synovial sarcoma on pathologic analysis (Figure 5).
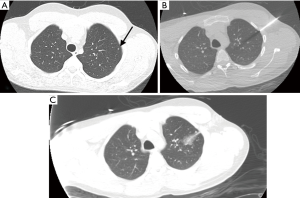
The patient did well during his postoperative course and a follow up CT scan after treatment with chemotherapy demonstrated that some of his pulmonary nodules had regressed, however, three persistent nodules were present and unchanged. The decision was made to resect these nodules using preoperative localization. A total of three nodules were localized and preoperatively injected with autologous blood, whose characteristics are detailed in Figure 3 (Case #2). The 4 mm left lower lobe nodule and a 2 mm right lower lobe nodule were both localized intraoperatively. The blood tattoo for a second right lower lobe 2 mm nodule was not visualized during the VATS procedure and so an excisional wedge biopsy was not performed. For this particular nodule, it was not visualized intraoperatively due to its very posterior location. The patient suffered no complication from either procedure.
Two patients who underwent CGBT were found to have lesions not associated with malignant disease. Case #5 was a 13 years old female with history of acute myeloblastic leukemia (AML-M5) with mixed lineage leukemia (MLL) rearrangement who while awaiting a bone marrow transplant had persistent fevers. CT imaging revealed a 13 mm ground glass opacity approximately 11 mm from the pleural surface. She underwent CGBT and wedge biopsy and pathology revealed an organizing pneumonia. Another patient, Case #8, was a 12 years old male with a history of Crohn’s disease who underwent an MRE to evaluate for active inflammation of the bowel and incidentally found an intrathoracic fluid collection at the level of the right middle lobe. Although initially asymptomatic, the patient later developed a cough and a CT was obtained that demonstrated 3 nodules ranging in size from 6 to 12 mm within the left lung. CGBT was performed in conjunction with a wedge resection and the pathology returned as a cavitary and caseating granulomata, negative for fungi, Bartonella, mycobacteria and non-tuberculous mycobacteria. The lesions were deemed to be associated with Crohn’s and his symptoms resolved.
Conclusions
VATS excision has decreased morbidity and mortality when compared with open thoracotomy, however it remains limited by the inability to palpate pulmonary nodules (1,2). Suzuki et al. reported that when pulmonary nodules are <10 mm in size or >5 mm deep to the pleural surface, there is a 63% rate of localization failure by instrument palpation (11). The inability of VATS to localize these lesions, or non-palpable lesions such as ground glass opacities poses a challenge for accurate lesion excision in the absence of preoperative marking.
The importance of preoperative localization for pulmonary metastases is further underscored by the variety of techniques developed over the past two decades. Multiple techniques including the use of methylene blue, hookwires, India ink, microcoils, ultrasound and the placement of technetium 99m macro-aggregated albumin have been described and have had varying diagnostic yield (5,8,9,12-15). Percutaneous K-wires can become dislodged during insufflation of pleural air and can have a higher rate of dislodgement when placed in superficial lesions (9,16). The success rate for excisional biopsy with the hook-wire technique ranges from 58% to 97% and the most commonly associated complication is pneumothorax and increases the risk of tearing the lung parenchyma. Ultrasound-guided biopsy carries a localization success rate of 93% to 100%, however is highly operator dependent and requires deflation of the lung to minimize air within the lung which limits visualization.
Localization utilizing methylene blue has been described in the pediatric population with some studies showing similar complications as in the adult cohorts (17). Patrick et al. used methylene blue for preoperative localization successfully in 12 patients, however, one patient was not successfully localized likely due to the diffusivity of methylene blue (18). Waldhausen successfully located 3 nodules in patients using a combination of a Homer mammographic needle and methylene blue (19). Heran described using a combination of a microcoil and fluoroscopy to confirm resection of pulmonary nodules in 6 pediatric patients (20). The diffuse spreading into surrounding tissue after injection of methylene blue is the characteristic that hinders its effectiveness in localizing the actual lesions.
We describe a technique that uses autologous blood alone for localization prior to VATS wedge biopsy. This method creates a distinct hematoma at the site of intended resection. This technique is safe and demonstrated a very high yield of successful localization and excision of lesions without the need for intraoperative ultrasound and complete lung deflation or use of a Geiger counter to detect radio nucleotide labelled albumin. The utility of this technique has been hinted at in one study, where localization of a pulmonary nodule was possible by identifying a hematoma in 3/4 patients whose hookwires dislodged (9). McDonnell et al. used Methylene blue mixed with autologous blood to prevent dissipation of the methylene blue (21). With this technique any blood that may be present outside of the hematoma can be easily suctioned and the delineated hematoma will remain, as opposed to methylene blue which has a lasting stain. Our technique eliminates the use of methylene blue, alleviating the potential risk of allergy. An additional theoretical benefit of the technique is the autologous clot serving as a blood patch as suggested by Filippo’s cohort where fine needle aspirations of pulmonary nodules had a lower incidence of pneumothorax when there was hemorrhage around the needle tract or high-grade local hemorrhage (>6 mm) (22).
We demonstrated a high success rate using autologous blood for preoperative localization of pulmonary lesions as small as 2 mm. A 2 mm nodule located 10 mm deep to the pleural surface was not localized intraoperatively with this technique, the nature of which is indeterminate. Our study is limited by the small cohort size, therefore studies in larger patient groups may need to be done to further validate the effectiveness of the technique. This technique, if successful in larger studies, may represent a cost-conscious alternative to other cited methods of preoperative pulmonary nodule localization.
Acknowledgments
Michael L. Baker, MD, Dartmouth-Hitchcock Medical Center, Department of Pathology, Division of Pediatric and Perinatal Pathology, provided pathology slides for manuscript. Presented at the Annual Meeting Canadian Association of Pediatric Surgeons (CAPS), Vancouver, Canada. September 22-25, 2016.
Funding: None.
Footnote
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-19-3800
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-19-3800). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013) and the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonization. After obtaining local Institutional Review Board (IRB) approval (IRB #00028981), we conducted a retrospective review from 2006 to 2019 of patients (ages 4–18 years old) at our institution that received a blood tattoo with autologous blood under CT guidance for the preoperative localization of a peripheral pulmonary nodules. All patients underwent informed consent prior to performing all procedures.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kuo E, Bharat A, Bontumasi N, et al. Impact of video-assisted thoracoscopic surgery on benign resections for solitary pulmonary nodules. Ann Thorac Surg. 2012;93:266-72; discussion 272-3. [Crossref] [PubMed]
- Gow KW, Chen MK, C, et al. American Pediatric Surgical Association New Technology Committee review on video-assisted thoracoscopic surgery for childhood cancer. J Pediatr Surg 2010;45:2227-33. [Crossref] [PubMed]
- Hayes-Jordan A, Connolly B, Temple M, et al. Image-guided percutaneous approach is superior to the thoracoscopic approach in the diagnosis of pulmonary nodules in children. J Pediatr Surg 2003;38:745-8. [Crossref] [PubMed]
- Daw NC, Chou AJ, Jaffe N, et al. Recurrent osteosarcoma with a single pulmonary metastasis: a multi-institutional review. Br J Cancer 2015;112:278-82. [Crossref] [PubMed]
- Tronc F, Conter C, Marec-Berard P, et al. Prognostic factors and long-term results of pulmonary metastasectomy for pediatric histologies. Eur J Cardiothorac Surg 2008;34:1240-6. [Crossref] [PubMed]
- Lin MW, Chen JS. Image-guided techniques for localizing pulmonary nodules in thoracoscopic surgery. J Thorac Dis 2016;8:S749-55. [Crossref] [PubMed]
- Kleedehn M, Kim DH, Lee FT, et al. Preoperative Pulmonary Nodule Localization: A Comparison of Methylene Blue and Hookwire Techniques. AJR Am J Roentgenol 2016;207:1334-9. [Crossref] [PubMed]
- Wicky S, Mayor B, Cuttat JF, et al. CT-guided localizations of pulmonary nodules with methylene blue injections for thoracoscopic resections. Chest 1994;106:1326-8. [Crossref] [PubMed]
- Ciriaco P, Negri G, Puglisi A, et al. Video-assisted thoracoscopic surgery for pulmonary nodules: rationale for preoperative computed tomography-guided hookwire localization. Eur J Cardiothorac Surg 2004;25:429-33. [Crossref] [PubMed]
- Khereba M, Ferraro P, Duranceau A, et al. Thoracoscopic localization of intraparenchymal pulmonary nodules using direct intracavitary thoracoscopic ultrasonography prevents conversion of VATS procedures to thoracotomy in selected patients. J Thorac Cardiovasc Surg 2012;144:1160-5. [Crossref] [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
- Magistrelli P, D'Ambra L, Berti S, et al. Use of India ink during preoperative computed tomography localization of small peripheral undiagnosed pulmonary nodules for thoracoscopic resection. World J Surg 2009;33:1421-4. [Crossref] [PubMed]
- Grogan EL, Jones DR, Kozower BD, et al. Identification of small lung nodules: technique of radiotracer-guided thoracoscopic biopsy. Ann Thorac Surg 2008;85:S772-7. [Crossref] [PubMed]
- Su TH, Fan YF, Jin L, et al. CT-guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol 2015;25:2627-33. [Crossref] [PubMed]
- Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc 2011;25:1723-9. [Crossref] [PubMed]
- Seo JM, Lee HY, Kim HK, et al. Factors determining successful computed tomography-guided localization of lung nodules. J Thorac Cardiovasc Surg 2012;143:809-14. [Crossref] [PubMed]
- Parida L, Fernandez-Pineda I, Uffman J, et al. Thoracoscopic resection of computed tomography-localized lung nodules in children. J Pediatr Surg 2013;48:750-6. [Crossref] [PubMed]
- Partrick DA, Bensard DD, Teitelbaum DH, et al. Successful thoracoscopic lung biopsy in children utilizing preoperative CT-guided localization. J Pediatr Surg 2002;37:970-3; discussion 970-3. [Crossref] [PubMed]
- Waldhausen JH, Shaw DW, Hall DG, et al. Needle localization for thoracoscopic resection of small pulmonary nodules in children. J Pediatr Surg 1997;32:1624-5. [Crossref] [PubMed]
- Heran MK, Sangha BS, Mayo JR, et al. Lung nodules in children: video-assisted thoracoscopic surgical resection after computed tomography-guided localization using a microcoil. J Pediatr Surg 2011;46:1292-7. [Crossref] [PubMed]
- McConnell PI, Feola GP, Meyers RL. Methylene blue-stained autologous blood for needle localization and thoracoscopic resection of deep pulmonary nodules. J Pediatr Surg 2002;37:1729-31. [Crossref] [PubMed]
- De Filippo M, Saba L, Silva M, et al. CT-guided biopsy of pulmonary nodules: is pulmonary hemorrhage a complication or an advantage? Diagn Interv Radiol 2014;20:421-5. [Crossref] [PubMed]