Promising but still uncertain steps towards better prediction of functional outcome in ICU patients
Predicting functional outcome
In a recent publication on their ‘Towards RECOVER’ study, an ongoing multicenter project evaluating patient and caregiver outcomes after prolonged mechanical ventilation, Herridge et al. report on functional outcome up to one year after discharge in patients who needed support in an intensive care unit (ICU) for more than one week (1). For this, the ‘Towards RECOVER’—investigators used the Functional Independence Measure (FIM), the Short-Form 36, a 6-minute walking test and Medical Research Counsel score-muscle strength testing. The main findings were that young patients (aged <42 years) who needed shorter ICU-care [length-of-stay (LOS) <2 weeks] had the best functional outcome, while elderly patients (aged >66 years) who needed longer ICU–care (LOS >2 weeks) had the worst functional outcome. Young patients with a LOS >2 weeks, older patients with a LOS <2 weeks, and patients aged 45 to 66 years with a LOS >2 weeks had a functional status in between the first two groups. Based on these results, the ‘Towards RECOVER’—researchers suggest that these age—and LOS cutoffs could be useful in resource planning and informing patients and their families about expected functional outcomes.
While we applaud the ‘Towards RECOVER’—investigators with their successful project and agree that resource planning and informing patients and their families is important, it should be recognized that there was large overlap in the functional outcome results between the age and LOS groups. Future analyses should focus on the predictive accuracy, which was not provided by the investigators in their present report. Interestingly, the suggested age—and LOS cutoffs could also be useful for stratification of patients. Stratification for functional outcome into more homogenous groups of patients is vital, e.g., to improve selection of patient for clinical trials that test rehabilitation programs aiming at better functional outcomes. One intriguing question, however, is why these two variables, age and LOS, after all are associated with functional outcome.
Associations versus causal relations
Age, a non-modifiable factor, may indirectly influence functional outcome, for several reasons. Elderly patients may already have a lower functional status before becoming critically ill, and age has been found to predict e.g., FIM scores irrespective of whether a patient was admitted to the ICU (2). Also, the reasons for ICU admission could be age-dependent, and could have different associations with functional outcome. Finally, older patients could be more ‘fragile’, which increases susceptibility to critical illness—induced injury, and maybe even intervention—associated damage. Indeed, several studies suggest that advanced age alters the response to certain ‘hits’ (3), such as the inflammatory response to a pulmonary insult (4), resulting e.g., in more extensive damage caused by mechanical ventilation. Age, thus, has an understandable association with functional outcomes after critical illness.
It is less understandable why LOS, which may also be seen as a non-modifiable factor, is associated with functional outcome. One could argue that more severely ill patients, and maybe even patients with chronic comorbidities, may simply require longer support of organ functions. Is functional outcome then affected by disease severity, by longer LOS, or both? Also, longer LOS increases or lengthens exposure to interventions that may unintentionally harm patients, such as ventilatory support (5), and increases the chance of all kinds of nosocomial infections (6).
Age and LOS thus may be seen as ‘composites’ of several risk factors. And more importantly, it is uncertain which part of the composite has a direct, or causal, relation with outcome. These specific parts may be modifiable—and provide targets for intervention.
Mediation analysis
Etiological understanding may enhance the usability of predictive models and may even allow for identification of variables that are modifiable. Here, maybe, we should consider using mediation analysis, a way to study intermediate variables between the independent (like age, or LOS) and the dependent variable (like functional outcome), which may explain the mechanism between these two variables. To understand what this type of analysis can do, let us first give two simple examples outside medicine. Complete mediation is the most simple cause and effect chain of events. When the sun shines, plants grow. This is completely mediated through photosynthesis within the chloroplast. When there is more than one intermediate factor between cause and effect, partial mediation occurs. For example, the level of highest education of the parents is associated with the highest level of education of the children. A geneticist could find that this effect is partly mediated through genetic factors while a social scientist may find similar effects for upbringing. Both are right and this can be explained by the influence of parents on their children is partly nature and partly nurture. An example more close to medicine, ICU medicine to be precise, is the one on driving pressure (7). Ventilation strategies that use lower plateau pressures, lower tidal volumes, and higher positive end-expiratory pressures (collectively termed ‘lung-protective strategies’) have been shown to benefit patients with the acute respiratory distress syndrome (ARDS) (8). The different components of lung-protective strategies all could reduce mechanical stresses on the lung, which are thought to induce lung injury. In a recent metaanalysis using individual patient data from several randomized controlled trials involving ARDS patients mediation analysis showed that reductions in tidal volume or increases in PEEP were beneficial only if associated with decreases in the driving pressure. No other ventilation variable had such a mediating effect. Thus, driving pressure could be the modifiable risk factor for lung injury, with tidal volume limitation and PEEP titrations only as two means to reach that goal.
We are in need of mediation analyses that help us understand which factors mediate the associations between age and LOS on the one hand, and functional outcome on the other hand. It could be that some of these mediating factors are modifiable, helping us to take wiser decision on what could be improved (more) to have a better outcome of critically ill patients.
Mediators
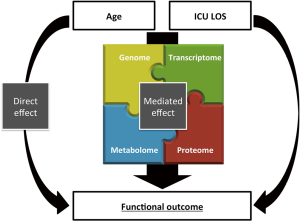
A deeper etiological understanding of the association between age and functional outcomes in critically ill patients may be obtained by studying biochemical processes or biological networks as mediators (Figure 1) (9). A relatively simple example is the association between smoking and lung cancer, which is mediated through carcinoids that lead to mutations in oncogenes and tumor suppressor genes. For more complex situations, the biochemical landscape within a patient can nowadays be captured with ‘omics’ technologies. Omics platforms are used to measure a large variety of molecules, in the form of epigenetic modifications (epigenomics), DNA (genomics), RNA (transcriptomics), proteins (proteomics) or metabolites (metabolomics). The contribution of biological pathways can be reconstructed when this data is combined with statistical tools and reference databases. Using this approach, modifiable risk factors may be identifiable, as certain key molecules within the pathways may be targeted with future treatment. Additionally, patients may be lumped together based on their biochemical profile, which may predict the response to treatment or give a better prognosis of outcome (10). These so called phenotypes may explain the heterogeneity between patients that may not be captured by looking at clinical diagnoses, age and LOS alone (11).
Conclusions
Prediction of functional outcomes is getting more important with recent decreases in mortality rates. The ‘Towards RECOVER’ study has taken the first step to show what certain factors are most strongly associated with functional outcomes. Age and LOS may be good predictors but in itself not or only poorly modifiable, but their association with outcome could be mediated through potentially modifiable, but yet unknown mediating factors.
Acknowledgements
None.
Footnote
Provenance: This is an invited Commentary commissioned by the Section Editor Zhiheng Xu (State Key Laboratory of Respiratory Disease, Guangzhou Institute of Respiratory Disease, Department of Intensive Care, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Herridge MS, Chu LM, Matte A, et al. The RECOVER Program: Disability Risk Groups & One Year Outcome after ≥ 7 Days of Mechanical Ventilation. Am J Respir Crit Care Med 2016. [Epub ahead of print]. [Crossref] [PubMed]
- Inouye SK, Peduzzi PN, Robison JT, et al. Importance of functional measures in predicting mortality among older hospitalized patients. JAMA 1998;279:1187-93. [Crossref] [PubMed]
- Vieira da Silva Pellegrina D, Severino P, Vieira Barbeiro H, et al. Septic Shock in Advanced Age: Transcriptome Analysis Reveals Altered Molecular Signatures in Neutrophil Granulocytes. PLoS One 2015;10:e0128341. [Crossref] [PubMed]
- Schouten LR, Schultz MJ, van Kaam AH, et al. Association between Maturation and Aging and Pulmonary Responses in Animal Models of Lung Injury: A Systematic Review. Anesthesiology 2015;123:389-408. [Crossref] [PubMed]
- Biehl M, Kashiouris MG, Gajic O. Ventilator-induced lung injury: minimizing its impact in patients with or at risk for ARDS. Respir Care 2013;58:927-37. [Crossref] [PubMed]
- Tess BH, Glenister HM, Rodrigues LC, et al. Incidence of hospital-acquired infection and length of hospital stay. Eur J Clin Microbiol Infect Dis 1993;12:81-6. [Crossref] [PubMed]
- Amato MB, Meade MO, Slutsky AS, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med 2015;372:747-55. [Crossref] [PubMed]
- Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med 2013;369:2126-36. [Crossref] [PubMed]
- Wheelock CE, Goss VM, Balgoma D, et al. Application of 'omics technologies to biomarker discovery in inflammatory lung diseases. Eur Respir J 2013;42:802-25. [Crossref] [PubMed]
- Prescott HC, Calfee CS, Thompson BT, et al. Towards smarter lumping and smarter splitting: rethinking strategies for sepsis and acute respiratory distress syndrome clinical trial design. Am J Respir Crit Care Med 2016;194:147-55. [Crossref] [PubMed]
- Auffray C, Adcock IM, Chung KF, et al. An integrative systems biology approach to understanding pulmonary diseases. Chest 2010;137:1410-6. [Crossref] [PubMed]


